- Volume 71 , Number 3
- Page: 227–30
"Relatively spared zones" in leprosy: a clinicopathological study of 500 patients
ABSTRACT
In this study, clinically all forms of lesions like macules, plaques, and nodules were found in all the "relatively spared zones," except groins. Histopathology confirmed that the disease process was established and the acid-fast bacilli were not present as a part of bacteremic settlement. Hence, it appears that practically no area on the surface of skin is immune to invasion by M. leprae. However, as the incidence of lesions and AFB in these regions is relatively less, especially over axilla and groin, these areas can be considered as relatively spared zones but not completely resistant to development of lesions of leprosy.RÉSUMÉ
Dans cette étude, toutes les formes lésionnelles cliniquement observables telles que des macules, plaques et des nodules furent trouvées dans toutes les « zones relativement épargnées , à l'exception des aines. L'examen histopathologique confirma que le processus morbide était établi et que les bacilles AAR n'étaient pas présents comme composante d'une localisation secondaire à une bactériémie. Ainsi, il apparaît qu'il n'existe pas pratiquement d'aires cutanées qui soit indemnes de l'invasion par M. leprae. Cependant, compte tenu de l'incidence moindre des lésions et des bacilles AAR dans ces régions, en particulier au niveau des aisselles et des aines, ces zones peuvent être considérées comme relativement épargnées mais pas complètement résistantes au développement de lésions de lèpre.RESUMEN
Se hizo un estudio histopatológico sobre la presencia de lesiones de la lepra en la superficie corporal de los pacientes con esta enfermedad. Se encontraron lesiones de todas las formas clínicas de la lepra (máculas, placas y nódulos) aun en las llamadas zonas respetadas por la enfermedad, con excepción de las ingles. Esto indica que no hay ningún área de la superficie de la piel que sea inmune a la invasión por M. leprae. Sin embargo, como la incidencia de lesiones y de BAAR en estas regiones es relativamente escasa, especialmente en la zona de las axilas y las ingles, estas áreas pueden considerarse como zonas relativamente respetadas pero no completamente resistentes al desarrollo de lesiones de la lepra.Leprosy is a chronic infectious disease with varied presentations caused by Mycobacterium leprae. The fact that few anatomic regions are relatively exempt from leprosy lesions was reported by earlier workers (5,8). The term "relatively spared zones" ("immune zones") is used in a non-immunological sense and it does not pertain to local immunity but only to relative sparing of certain anatomical sites from leprosy lesions. However, some studies have cast doubts on the existence of "relatively spared zones," especially in lepromatous leprosy (4,12,16). We undertook this study to learn more about these interesting but poorly understood so called "relatively spared zones" of leprosy across the spectrum of disease.
MATERIALS AND METHODS
Five hundred leprosy patients irrespective of age, sex, type of disease and treatment were enrolled in the study over a period of 2 years from the leprosy clinic of our institute and the patients residing in a local leprosy colony. Demographic data and findings on complete cutaneous examination were noted. Slit skin smear and skin biopsy were done and patients were classified according to Ridley-Jopling (11). Clinical description of lesions present in the "relatively spared zones" in addition to all other sites was recorded in a predesigned proforma. Skin biopsies were taken randomly in every spectrum from 37 lesions present over "relatively spared zones" to study histopathological changes. Involvement of palms, soles, and other "relatively spared zones" was correlated with different parameters like type and duration of disease, age, and sex, reactional states, treatment status etc. In addition, 30 multibacillary borderline leprosy/lepromatous leprosy (BL/LL) cases were studied by slit skin smear examination to act as controls without any apparent lesions over palms, soles, scalp, axillae, and groin.
RESULTS
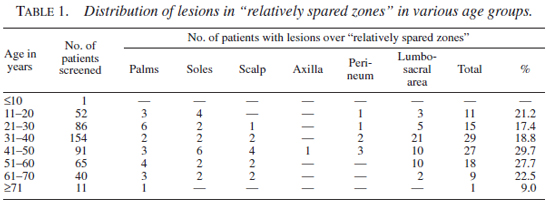
Age and sex distribution. Of the 500 patients studied, 351 were males and 149 females of ages ranging from 8-90 years (mean age 34 ± 3.2 years). Clinically apparent lesions over "relatively spared zones" were found in 110 (22%) patients. There was no statistically significant difference in the frequency of distribution of lesions of leprosy in these zones, between the different age groups (p >0.1). Involvement of the "relatively spared zones" occurred at an almost equal frequency in males (20.8%) and females (24.8%), with slight predilection for palmoplantar involvement in the females than in the males (10.7% vs. 6.8%). Distribution of lesions in "relatively spared zones" in various age groups is given in Table 1.
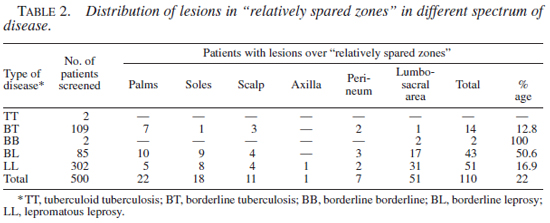
Sites involved. Various types of lesions, i.e. macules, papulo-plaques, nodules, alopecic patches, were observed over the "relatively spared zones." These lesions were found more frequently (50.6%, 43/85) in BL than in LL (16.9%, 51/302). The distribution of leprosy lesions in various "relatively spared zones" in relation to the spectrum of the disease is given in Table 2.
Reactions. Twenty-eight (18 males, 10 females) patients at the time of screening had reaction (Type 1 in 16, Type 2 in 12). Lesions over "relatively spared zones" were seen much more frequently in those undergoing reaction 18/28 (64.3%) compared to those who were not in reaction (92/472, 19.5%). This difference was found to be statistically significant (p <0.01).
Treatment status. Screened patients were either fresh untreated, or were taking treatment, or had completed treatment and were on follow up. Of the 110 patients with lesions over "relatively spared zones," 12 were untreated, 70 were on multidrug therapy (MDT) multibacillary (MB), 8 on MDT paucibacillary (PB) regimens, 5 had completed treatment and 15 patients had taken a combination of regimens from other places. No correlation could be established between presence of lesions over "relatively spared zones" and treatment status of the patients.
Duration of disease. Duration of disease in patients with lesions over "relatively spared zones" varied from 1 month to 17 years. Majority (78/110,70.9%) had the disease for less than 5 years. However, no correlation was found between the occurrence of lesions over "relatively spared zones" and the duration of disease.
Histopathology. Histopathological changes were studied from 37 patients with lesions in the "relatively spared zones." Diagnosis of leprosy could be clearly made on histopathology in 34 specimens. Two cases (BL-1, LL-1) with diffuse ichthyotic lesions over the lower back, and one case (LL) with alopecic patch over scalp showed evidence of chronic inflammation but no definite evidence of leprosy. Acid-fast bacilli (AFB) in the sections varied from occasional bacilli (11/34) to the presence of globi (1/34).
Of the 34 leprosy lesions confirmed on histopathology, clinicopathological correlation could be made in 26 cases (8/12 palmar lesions, 7/8 plantar lesions, 6/9 lumbosacral lesions, 2/2 scalp lesions, 2/2 perineal lesions, 1/1 axillary lesion).
Study of apparently normal skin of the "relatively spared zones.". In the control group, AFB in the "relatively spared zones" on slit skin smears were found in 12/30 (40%) cases [6 lepromatous leprosy polar (LLP), 4 lepromatous leprosy subpolar (LLS), 2 BL]. Among the various "relatively spared zones" studied, palms were the most common site for presence of AFB followed by soles, scalp, and groin. No AFB could be detected in the SSS from axillae. Bacterial Index (BI) at the "relatively spared " sites was less than the average of routine sites in 9, and equal in 3 cases.
DISCUSSION
The distribution of leprosy lesions, affecting predominantly the skin, nasal mucosa, and peripheral nerves particularly more superficial ones is the evidence for suggesting that M. leprae prefer a growth temperature of less than 37ºC (7,15,16). Certain anatomical sites like scalp, groin, axillae, perineum, and a transverse strip of skin over lumbosacral region were considered relatively unsusceptible to the development of leprosy by many workers (6,8,11,17). The unsusceptibility was attributed to the relative warmth of these regions (2). Palms and soles were also included in the over "relatively spared zones" by some workers (1,2,9). The thick epidermis of palms and soles along with the good amount of fibro fatty tissue provide an insulating property and hence a high nerve bed temperature, which renders the palmoplantar localization of M. leprae less likely.
Clinically apparent lesions over the over "relatively spared zones" were found in 22% (110/500) of the patients in the present study. Lesions over "relatively spared zones" were seen most frequently over the lumbosacral region, followed by palms and soles, scalp, perineum, and axilla in the descending order. Lesions of leprosy occurring over the over "relatively spared zones" have been reported by other workers also (10,13,14,17). Sahni, et al. (17) reported lumbosacral region to be the most common, and the groin to be the least affected site. The increased incidence of lesions over over "relatively spared zones" in patients with reactions, especially Type 1 reaction, could be due to the fact that clinically unapparent lesions become obvious during reaction. The incidence of palmoplantar lesions in reactions is reported to be high as shown by Arora, et al. (3) who found 50% of the patients with palmoplantar lesions to be in Type 1 reaction. Involvement of over "relatively spared zones" occurred more or less at an equal frequency in males and females with slight predilection of palmoplantar lesions in females. This may be due to the fact that most of these female patients were in reaction.
Lesions occurred more frequently in the BL than in LL. The lesions in borderline disease are numerically more in number, and this increases the chances of occurrence of lesions over over "relatively spared zones" as well. Though the disease in LL is even more widespread, clinically discernable lesions, especially like infiltration over the palms, soles, and scalp, is difficult to appreciate in the diffuse infiltrative form (non-nodular), and hence may explain the lower incidence of lesions over "relatively spared zones" in LL. No correlation was found between the occurrence of lesions over "relatively spared zones" and duration of disease or treatment status. This could be because lesions once present are likely to take a long time for clearance/disappearance.
AFB in "relatively spared zones" were found more commonly in LL disease than in BL disease, thereby indicating presence of bacillemia in lepromatous disease. In the past, some Indian workers have reported changes suggestive of leprosy in the clinically normal looking skin in multibacillary disease (4,10,12).
REFERENCES
1. Aggarwal, S.K., Arora, P.N., Chattopadhyay, S.P. and Ramakrishnan, K.R. Primary involvement of sole in leprosy. Indian J. Lepr. 59(1987)472-473.
2. Anish, S.A. The relationship between surface temperature and dermal invasion in lepromatous leprosy. Int. J. Lepr. Other Mycobact. Dis. 39(1971)848-851.
3. Arora, S.K., Mukhija, R.D., Mohan, L., Girdhar, M. and Sharma, S.P. A study of palmoplantar lesions in leprosy. A preliminary report. Indian J. Lepr. 61(1989)206-208.
4. Bedi, T.R., Kumar, B. and Kaur, S. Histopathologic study of clinically normal appearing skin in lepromatous leprosy. Lepr. India. 51(1979)78-80.
5. Cochrane, R.C. Signs and symptoms. In: Leprosy in Theory and Practice, 1st edn. Bristol: John Wright & Sons Ltd, 1959, p. 129
6. Fox, H. and Knott, J. Leprous nodules of male genitalia. Int. J. Lepr. 2(1932)445-446.
7. Hastings, R.C. The microbiology of leprosy. In: Leprosy. 1st edn. Edinburgh: Churchill Livingstone, 1985, p. 37
8. Hopkins, R., Denney, O.E. and Jonansen, F.A. Immunity of certain anatomic regions from lesions of skin leprosy. Arch. Dermatol. 20(1929)767-779.
9. Indira, D., Kaur, I., Sharma, V.K. and Das, A. Palmoplantar lesions in leprosy. Indian J. Lepr. 71(1999)167-172.
10. Jayakumar, J., Aschhoff, M., Renuka, G. and Meyers, W.M. Involvement of scalp, axillae, and groins in lepromatous leprosy. Indian J. Lepr. 64(1992)541-544.
11. Jopling, W.H. and McDougall, A.C. The disease. In: Handbook of Leprosy, 4th edn. New Delhi: CBS Publishers and distributors, 1992, p. 2487
12. Kaur, S. and Kumar, B. Study of apparently uninvolved skin in leprosy as regards bacillary population at various sites. Lepr. India. 50(1978)38-44.
13. Murthy, M.P., Hedge, R. and Chandrasekhar, H.R. Immune zones in leprosy. Indian J. Dermatol. Venerol. Leprol. 58(1992)356
14. Ramanujan, K. Leprosy lesions at unusual sites. Indian J. Lepr. 62(1990)402-440.
15. Sabin, T.D. Temperature-linked sensory loss. A unique pattern in leprosy. Arch. Neurol. 20(1969)257-262.
16. Sabin, T.D., Hackett, E.R. and Brand, P.W. Temperatures along the course of certain nerves often affected in lepromatous leprosy. Int. J. Lepr. Other Mycobact. Dis. 42(1974)38-42.
17. Sahni, U., Reddy, B.S.N. and Malik, R. Clinico-pathological study of so-called immune zones in leprosy. Lepr. India. 54(1982)256-262.
1. M.D., MNAMS; Department of Dermatology, Venereology & Leprology and Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
2. M.D.; Department of Dermatology, Venereology & Leprology and Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
3. M.D., MNAMS; Department of Dermatology, Venereology & Leprology and Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
4. M.D., MNAMS; Department of Dermatology, Venereology & Leprology and Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
5. M.D.; Department of Dermatology, Venereology & Leprology and Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
6. M.D., MNAMS, Department of Dermatology, Venereology & Leprology and Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India.
Reprint requests to: Dr. Inderjeet Kaur, Additional Professor, Dept. of Dermatology, Venereology & Leprology, PGIMER, Chandigarh-160 012, India. FAX: +91 (0172) 744401, 745078, E-mail: Kaur_inderjeet@yahoo.com
Received for publication on 24 September 2002.
Accepted for publication on 17 June 2003.