- Volume 71 , Number 3
- Page: 248–56
"Elimination" of leprosy and the need to sustain leprosy services, expectations, predictions and reality
The International Leprosy Association (ILA) Technical Forum report, The Current Leprosy Situation, Epidemiology and Control and the Organization of Leprosy Services (5), gives a lot of attention to the goal for elimination of leprosy as a public health problem. In 1991, this was defined by the World Health Organization (WHO) as a prevalence smaller than one per 10,000 population (9). Underlying this elimination strategy was the hypothesis that because leprosy patients are assumed to be the sole source of infection, early detection and treatment with multidrug therapy (MDT) would reduce transmission of Mycobacterium leprae (11). It was expected that once the prevalence fell below this level, the chain of transmission would be broken, and leprosy would disappear naturally (10). In 1993, WHO made predictions regarding the expected trends of the prevalence, number of registered cases, incidence, and number of cases detected till the year 2000 (Fig. 1) (12).
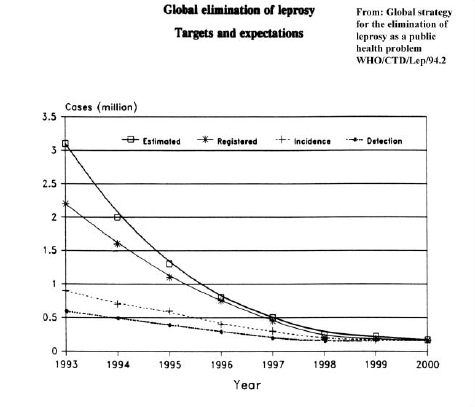
Fig. 1. Global elimination of leprosy, targets and expectations.
The expectation was that by the end of the year 2000, the prevalence and incidence would both be about 200,000. But, what was the actual situation by the end of 2000 (Fig. 2)?
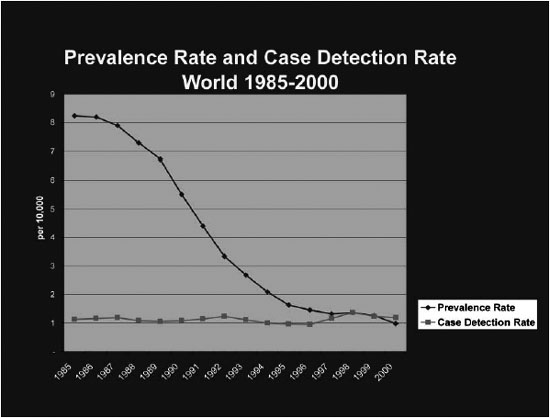
Fig. 2. Prevalence rate and case detection rate world, 1985–2000.
By the end of the year 2000, both the registered prevalence (597,000) and the number of cases detected (719,000) were much higher than the predicted 200,000. The global prevalence of registered cases came just below the level of 1 per 10,000. This is a great change, because it represents a reduction of 90% from the prevalence reported in 1985. Of course, we do not know the actual prevalence or the actual incidence, but it is well known that the actual prevalence and incidence can be very different from the prevalence of cases registered for treatment or the number of cases detected during the year, respectively.
A goal for the elimination of an infectious disease makes sense only if it means reduction of transmission of infection and, consequently, reduction of incidence of disease. However, despite a dramatic reduction in the number of leprosy patients registered for treatment, the number of newly detected cases at the global level has not shown a comparable decline. On the contrary, it has increased (Fig. 3).
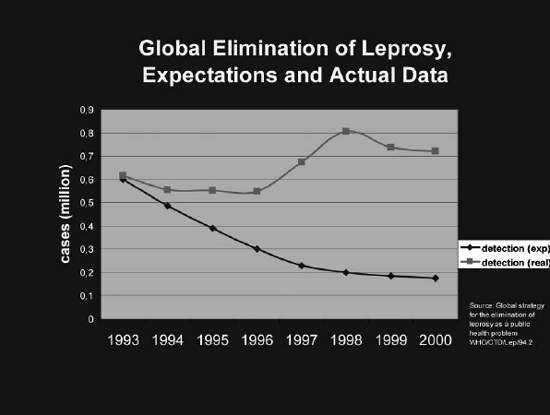
Fig. 3. Global elimination of leprosy, expectations for case detection and actual data.
The expectation that a reduction of prevalence to very low levels would lead to a reduction of transmission of infection has shown to be a fundamental miscalculation. Transmission is probably decreasing, but it is a very slow process and we have more evidence that it is caused by socio-economic improvement and bacillus Calmette-Guérin (BCG) than by an additional impact of MDT as compared with the impact of dapsone monotherapy (1,6,7,8).
The Technical Forum concluded that there is no consistent evidence that the introduction of MDT has accelerated the decline of the incidence of leprosy. Several explanations are possible for the lack of acceleration: (i) the increased case detection efforts, (ii) the increased coverage of leprosy services, (iii) there may be other important sources of transmission than untreated patients, (iv) the long incubation period of leprosy, or (v) the patients with the infectious type of the disease have transmitted the infection in their environment before they are detected and treated.
The Technical Forum concluded that, whereas early diagnosis and regular treatment by MDT will remain the cornerstones of leprosy control for the foreseeable future, additional strategies should be developed, based on better understanding of the epidemiology of the disease (R). The 'R' means that this is an area recommended for further research.
In this context the Technical Forum has formulated three recommendations. (i) Vaccination with BCG as part of childhood immunization must be continued in countries in which leprosy still exists (EB), where 'EB' means that this recommendation is evidence based. (ii) The possible role of chemoprophylaxis based on bactericidal drugs should be further studied (R). (iii) More research is needed, particularly on transmission of M. leprae, the role of sub-clinical infection, progression from infection to disease, and trends of incidence of the disease, including the impact of MDT (R).
What does explain the declining prevalence? In the epidemiological definition, the prevalence is equal to the product of the incidence and the duration of disease (P = I x D). 'P' is the point prevalence, i.e., the number of leprosy cases in need of chemotherapy at a defined point of time, usually the end of the year. 'I' is the incidence, i.e., the number of new cases of leprosy that occur during a year. 'D' is the duration of disease.
The operational definition of prevalence chosen for the WHO elimination campaign is quite different. The prevalence of cases registered for chemotherapy is equal to the annual number of cases detected times the duration of treatment with MDT (Preg = CD x Dmdt). This (registered) prevalence is subject to many influences, such as: (i) shortening of duration of treatment [Since 1993, the treatment of multibacillary (MB) leprosy has been shortened from 24 months to 12 months and in some major leprosy endemic countries single lesion leprosy is treated with a single dose of ROM (a combination of rifampicin, ofloxacin, and minocycline)], (ii) methods of case finding (active vs. passive case finding activities), (iii) updating of the registers ("cleaning" of the registers has contributed tremendously to the decline, which in some countries was sufficient to "eliminate" leprosy).
Since case detection figures are basically unchanged, it can be concluded that the decrease of the registered prevalence is mainly the result of shortening of treatment duration and cleaning of the registers, and does not reflect an actual reduction of the transmission of M. leprae.
This is also illustrated by the data from Ethiopia where I was working as the WHO adviser to the National Tuberculosis and Leprosy Control Program from 1996 to 2000 (Fig. 4).
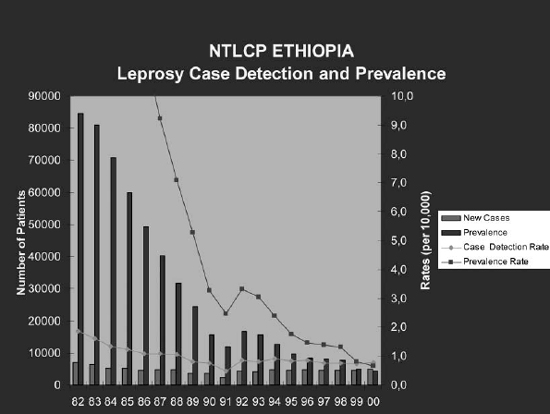
Fig. 4. NTLCP Ethiopia, leprosy case detection and prevalence.
There was an impressive decline of registered prevalence in Ethiopia from 85,000 in 1982 to 5000 in the year 2000, but the annual case detection remains stable around 5000, during the last decade. In 1998, Ethiopia changed the 24 months MDT regimen for MB patients to 12 months, and suddenly, but of course not unexpectedly, the 'prevalence' dropped the following year from just above to just below the magic 1/10,000 and WHO stated that leprosy had been eliminated in Ethiopia. According to various WHO publications, including the recently published WHO booklet, "The Final Push to Eliminate Leprosy as a Public Health Problem, Questions and Answers" (10), leprosy will now die out naturally in Ethiopia. But the only thing that has happened is that the duration of MDT for MB leprosy has been shortened. Nothing else has changed. The annual number of new cases is still the same as it was during the time when leprosy was not yet eliminated as a public health problem.
Epidemiologists have been very skeptical regarding the statement that leprosy will die out naturally after a prevalence rate below 1 per 10,000 has been reached. And the skepticism only became stronger when a few years ago a new slogan was launched by WHO: "The Final Push" strategy with the message that 2.5 million remaining cases have to be detected and cured, suggesting that there will be no transmission anymore after the target of 1 per 10,000 has been reached (10).
The Technical Forum has done an extensive literature search for evidence supporting this statement, but that was not found and therefore, the conclusion is that there is no evidence that once a predefined level of prevalence rate is reached, leprosy will necessarily die out.
So, it is obvious that the prevalence of cases registered for treatment is not an appropriate indicator for progress towards real elimination. Are there better indicators? I will answer this question by first showing an example from the Indonesian Province Central Jawa (Fig. 5).
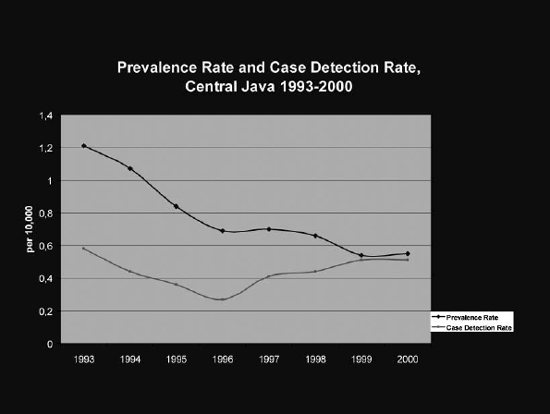
Fig. 5. Prevalence rate and case detection rate Central Jawa 1993–2000.
In 1995, the elimination target was achieved. We are often so impressed by the prevalence curve, that we do not realize what actually happens with the case detection figures. But what does "elimination" look like, if we look at case detection only? (Fig. 6).
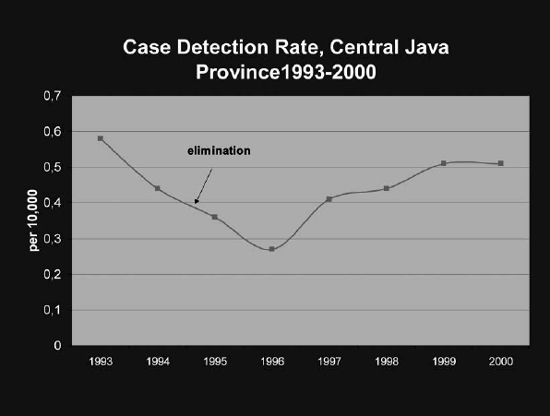
Fig. 6. Case detection rate Central Jawa 1993–2000.
How can one logically explain that since the indicated point in time, leprosy has been eliminated and is going to die out naturally?
There is a great risk that irrational interpretation of the elimination goal results in situations in which countries claim that the leprosy control service has successfully eliminated the disease, and as a consequence, could be discontinued. The danger is that we will end up with continuing transmission and hundreds of thousands of new cases every year, but without leprosy services that can deal with them.
Two mistakes have been made. In the first place, the wrong indicator (the prevalence of patients registered for MDT) has been selected to reflect the progress towards elimination of leprosy (i.e., reduced transmission and incidence). The second mistake is a classical error that is often made in public health: instead of using the indicator as a limited tool to reflect the progress towards the goal of reduced transmission, the indicator itself has become the goal, and the actual goal has practically gotten out of sight.
Regarding the use of indicators, the Technical Forum concluded that prevalence alone is of limited value as an indicator of leprosy control. The new-case detection-rate may be a better indicator, in conjunction with other indicators. The treatment completion rate is an important indicator of the effectiveness of patient management (BP). "BP" means that this is considered as the best practice.
The new-case detection-rate is the most logical proxy-indicator of incidence. However, it also poses some problems of interpretation. (i) It is directly influenced by the frequency and quality of detection. (ii) A number of newly detected cases may have developed leprosy several years earlier. But at the same time, (iii) some people who develop symptoms will be detected only after a number of years, and thus will not be included in the current year's case detection rate.
In spite of these limitations, trends of case detection reflect trends of incidence, on condition that there has been no important change of detection activities.
For routine use in integrated programs the most appropriate indicators are: (i) number (rate) of new cases, both paucibacillary (PB) and MB; (ii) proportion of newly detected patients with disability grade 2, which reflects the degree of delay before detection, and if it is stable the trends of case detection reflect trends of incidence; and (iii) treatment completion rate.
These indicators are also useful for self-evaluation by the health workers. They can be easily translated into their major responsibilities: find patients before they have developed disability and cure them.
Another relevant indicator is the proportion of children among new cases. A large proportion is a sign of recent transmission of the infection. Thus, it is an important epidemiological indicator, even though the proportion can also be influenced by operational factors, such as school surveys. In 2000, the global data showed a child proportion of 17%. The Technical Forum does not recommend routine reporting on this indicator in integrated programs. If needed, the information can be collected through a special study, sentinel surveillance, during supervisory visits, etc.
The issue of indicators for routine programs brings us from the chapter on epidemiology and control to the chapter on the organization of services. We have seen that the number of new cases detected globally has changed very little over the years. Moreover, some countries that had not reached the elimination target by the end of 2000, may have difficulties reaching it by the year 2005 (Fig. 7).
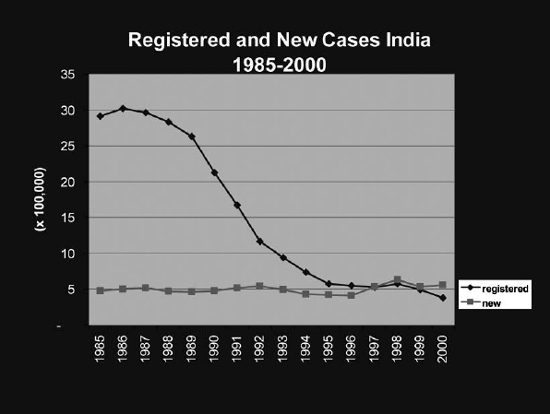
Fig. 7. Registered and new cases in India.
To reach the elimination target the number of registered cases has to reach a level of about 100,000. In many states in India it will not be feasible to achieve the elimination target, unless we reduce case detection activities, or further reduce the duration of MDT.
The Technical Forum concluded that significant numbers of new patients will continue to present for many years. Thus, it is essential to ensure that leprosy control activities have to be sustained, even in countries or areas that have officially reached the elimination target (BP).
For many years to come, every year hundreds of thousands of new cases will occur. They must be detected at an early stage and given regular and complete treatment with MDT. Some of the new patients will have disability at diagnosis, and many are at risk to develop disability after diagnosis. Moreover, about 3 million "cured" cases are disabled and in need of care. Leprosy services will need to be sustained far into this century (3).
Disease control can be defined as reduction of the incidence and prevalence of the disease, and of the morbidity and mortality resulting from the disease to a locally acceptable level as a result of deliberate efforts. Continued intervention is required to maintain the reduction (2). The strategy to achieve control of leprosy has four major elements: (i) early case detection, (ii) adequate chemotherapy (MDT), (iii) prevention of leprosy related impairments, and (iv) rehabilitation.
Implementation of this strategy ideally requires accessible, cost-effective, and sustainable health services that cover the population fully, and are accepted by the community and the patients. This strategy implies that leprosy control activities should be implemented by the general health services. Several integrated programs have shown that leprosy control can be effectively implemented by general health workers (4). There is a broad consensus on the need to integrate leprosy services into the general health system. WHO, the International Federation of Anti-Leprosy Associations (ILEP), and ILA see this as the most realistic strategy to sustain cost-effective leprosy services. Integration is also a central element of the health sector reforms.
Integration means that day-to-day patient management will become the responsibility of general health staff. Integration does not mean that specialized elements need to disappear from the health service. On the contrary, specialized components must be available within the general health service at the central and intermediate levels for planning, evaluation, training, technical supervision, referral services, and research. Depending upon local conditions, each country or region must decide at which level of the health system such specialized support should be available.
Where case-detection rates are low, a focused approach is appropriate, whereby services are provided mainly in selected general health facilities in the areas in which leprosy still occurs. The skills of general health workers will be limited mainly to suspecting leprosy and referral of suspects to specialized staff at the intermediate levels to confirm the diagnosis and begin treatment. Continuation of treatment could be delegated to the peripheral health facility serving the community in which the patient resides. The resources devoted to leprosy must be in balance with those required for other, often much more serious, public health problems (BP).
The Technical Forum report gives recommendations on the requirements for effective integration. In summary:
• Government must make a commitment to sustained leprosy control activities.
• General health service infrastructure must function adequately.
• The integration process must be carefully planned, appropriate to the local situation.
• Maintain a well-functioning central leprosy unit, usually housed in the Ministry of Health.
• An uninterrupted supply of anti-leprosy drugs must be guaranteed.
• Follow appropriate (simplified) field procedures, including recording and reporting.
• National strategies should clearly define the role of the private sector.
• Non-governmental organizations supporting leprosy control continue to be important partners with governments in integrated leprosy control programs.
• It is important that the various agencies involved in leprosy control collaborate and coordinate their activities, in order to increase their effectiveness.
• In integrating leprosy control into general health services, equity and quality of care for leprosy patients should be assured.
This implies that the services for leprosy patients should provide the same level of quality as do the services for other health problems (not less, but not more either).
• Training of all categories of staff involved in leprosy control should be task-oriented. Leprosy should be included in the curricula of medical faculties and paramedical schools (BP).
• Information, Education and Confirmation (IEC) activities result in increased knowledge, change of behavior, and reduction of stigma (EB). They should preferably be combined with IEC for other health problem (BP).
• Leprosy elimination campaigns (LEC) can play an important role in the process of integration. Case-finding in LEC must be based on self-reporting to the general health staff (BP).
Although there is consensus on the need for integration and the consequent need for simplification of the leprosy control activities and procedures, there is a serious disagreement on the interpretation of the word "simplification." Simplified guidelines should still respect well defined, minimal acceptable levels of quality and effectiveness, and in this regard the Technical Forum believes that a number of recent WHO guidelines concerning diagnosis, treatment, and prevention of disability are unacceptably oversimplified. These issues are discussed in the other three chapters of the Technical Forum report: the diagnosis and classification of leprosy, chemotherapy, and prevention of disabilities and rehabilitation.
The conclusion of this discussion on the chapters of the ILA Technical Forum report on epidemiology, control, and organization of services is that the WHO elimination goal has created a broad and strong commitment to the fight against leprosy. However, the number of new cases detected globally has changed very little. This is mainly explained by the disappointing additional impact of MDT on transmission. The strong decrease in registered prevalence is not based on a decreasing incidence, and can be explained by the shortening of treatment duration and cleaning of the registers. Since leprosy will continue to be a problem beyond 2005, leprosy services have to be sustained. This should be done by integrating leprosy activities into the general health services.
Detailed information and extensive literature references are available in the full report.
- Pieter Feenstra, M.D., M.P.H.
Head, Leprosy Unit
KIT (Royal Tropical Institute)
Amsterdam, The Netherlands
REFERENCES
1. Convit, J., Sampson, C., Zuniga, M., Smith, P.G., Plata, J., Silva, J., Molina, J., Pinardi, M.E., Bloom, B.R. and Salgado, A. Immunoprophylactic trial with combined Mycobacterium leprae/BCG vaccine against leprosy: preliminary results. Lancet. 339(1992)446-450.
2. Dowle, W.R. The principles of disease elimination and eradication. Bull. WHO. 67(1998)22-25.
3. Feenstra, P. Sustainability of leprosy control in low-endemic situations. Int. J. Lepr. Other Mycobact. Dis. 62(1994)599-608.
4. Feenstra, P. and Visschedijk, J. Leprosy control through the general health services-revisiting the concept of integration. Lepr. Rev. 73(2002)111-122.
5. ILA Technical Forum Report. The current leprosy situation, epidemiology and control and the organization of leprosy services. Int. J. Lepr. Other Mycobact. Dis. 70 suppl.(2002).
6. Karonga Prevention Trial Group. Randomized controlled trial of single BCG, repeated BCG, or combined BCG and killed Mycobacterium leprae vaccine for prevention of leprosy and tuberculosis in Malawi. Lancet. 348(1996)17-24.
7. Lwin, K., Sundaresan, T., Gyi, M.M., Bechelli, L.M., Tamondong, C., Garbajosa, P.G., Sansarricq, H. and Noordeen, S.K. BCG vaccination of children against leprosy: fourteen-year findings of the trial in Burma. Bull. WHO. 63(1985)1069-1078.
8. Saikawa, K. The effect of rapid socio-economic development on the frequency of leprosy in a population. Lepr. Rev. 52 Suppl.(1981)S167-S175.
9. World Health Assembly. Leprosy Resolution WHA 44.9, Forty-fourth World Health Assembly, 13 May 1991.
10. World Health Organization. The final push strategy to eliminate leprosy as a public health problem. Questions and answers. 1st edn. 2002.
11. World Health Organization. Expert Committee on Leprosy. Seventh Report, Geneva, 1997.
12. World Health Organization. Global strategy for the elimination of leprosy as a public health problem. Geneva, 1994.
This review is based on a presentation under the same title made by Dr. Feenstra at the 16th International Leprosy Congress, Salvador, Brazil.
Mailing address: Pieter Feenstra, Head, Leprosy Unit, KIT (Royal Tropical Institute) Wibautstraat 137j, 1097 DN, Amsterdam, The Netherlands. E-mail: p.feenstra@kit.nl
Received for publication on 5 November 2002.
Accepted for publication on 15 March 2003.