- Volume 71 , Number 2
- Page: 95–100
Should household contact examination in a low endemic situation of leprosy continue?
ABSTRACT
After more than 40 yrs of effort, leprosy is finally under control in Shandong province with only 50 to 70 new cases detected each year in the past 10 yrs. Contact examination is still compulsory and household contacts will be followed for 5 to 10 yrs, as directed by the guidelines of the national leprosy control program. In order to assess the value of contact examination in terms of case finding in a low endemic situation of leprosy in Shandong, we analyzed the data regarding all newly diagnosed leprosy cases in the past 11 yrs using the data abstracted f rom the national leprosy recording and reporting system, and a questionnaire-based survey to see how many incident leprosy cases would be detected if we followed the policy for contact examination of leprosy in Shandong.The results showed that 252 out of 547 leprosy cases diagnosed f rom 1990 to 2001 reported they had contact with different categories of primary leprosy cases. Among them, 90 cases had household primary leprosy cases. The mean incubation of the 252 index cases was 23 yrs. If we followed the national policy for contact tracing for 5 or 10 yrs, then only 12 (13.3%) and 10 (11.1%) of the 90 cases whose source of infection was household contacts would have been detected, respectively. Therefore, other approaches should be sought, in order to detect the few incident leprosy cases as early as possible in such a low endemic situation of leprosy in Shandong.
RÉSUMÉ
Après plus de 40 années d'effort, la lèpre est maintenant mieux contrôlée dans la province de Shandong, avec seulement entre 50 et 70 nouveaux cas détectés chaque année, durant ces dix dernières années. L'examen des sujets contacts est encore obligatoire et les contacts vivant sous le même foyer seront suivis pendant 5 à 10 ans, comme spécifié par les directives du programme national de contrôle de la lèpre. Afin d'évaluer l'intérêt d'examiner les contacts en terme de détection de cas dans un contexte de faible endémicité de lèpre dans le Shandong, nous avons analysé les données de tous les cas de lèpre nouvellement diagnostiqués ces 11 dernières années en utilisant les données extraites du système national d'en-registrement et de rapport de la lèpre, ainsi que d'une enquête basée sur un questionnaire visant à voir comment de nombreux cas incidents de lèpre seraient détectés si nous suivions les règles nationales de l'examen des contact de cas de lèpre à Shandong.Les résultats ont montré que 252 parmi 547 cas de lèpre diagnostiqués entre 1990 et 2001 ont mentionnés qu'ils ont eu un contact avec les différentes catégories de cas primaires de lèpre. Parmi ces derniers, 90 cas ont eu des cas primaires de lèpre sous le même toit. L'incubation moyenne de ces 252 propositus était de 23 ans. Seulement 12 (13,3%) et 10 (11,1%) de ces 90 cas dont la source de l'infection ont été des cas primaires de lèpre sous le même toit auraient été détectés si nous avions suivi la politique nationale pour le suivi des cas. Il apparaît donc que d'autres approches devraient être recherchées, afin de détecter les quelques nouveau cas de lèpre le plus tôt possible dans cette situation d'endémicité particulièrement faible de lèpre à Shandong.
RESUMEN
Después de más de 40 años de esfuerzo, la lepra está ahora bajo control en la provincia de Shandong, con 50 a 70 casos nuevos detectados cada año en los últimos 10 años. El examen de los contactos es obligatorio y los contactos familiares deben ser vigilados durante 5 a 10 años, como lo indica el reglamento del Programa Nacional de Control Contra la Lepra. Con objeto de establecer la importancia del control de los contactos en el descubrimiento de nuevos casos en un área de baja endemia como la Provincia de Shandong, analizamos los registros de los casos nuevos de lepra descubiertos en los últimos 11 años. Utilizamos los datos extraídos del Sistema Nacional de Registro de la Lepra y aplicamos un cuestionario para calcular cuantos casos incidentes de lepra podrían ser detectados si se aplicara la política del examen de contactos en Shandong.Los resultados indicaron que 252 de 547 casos de lepra diagnosticados entre 1999 y 2001 habían tenido contacto con algún caso de lepra y que dentro de ellos, 90 habían sido contactos intrafamiliares de pacientes con lepra. El tiempo promedio de incubación de los 252 casos índice fue de 23 años. De haberse aplicado la política nacional para la detección de casos que implica un periodo de seguimiento de 5 o 10 años, solo se hubieran podido detectar 12 (13.3%) o 10 (11.1%) de los 90 casos, respectivamente, cuya fuente de infección fue un contacto intrafamiliar. Es claro que deben considerarse otras alternativas para detectar, lo más temprano posible, los pocos casos incidentes de lepra en una región de baja endemia como Shandong.
The distribution of leprosy in a population tends to be in a cluster pattern, and it is generally accepted that contact examination is one of the important methods in case finding of new leprosy cases in any leprosy control program. This is evidenced by the fact that people living in the same household as leprosy patients have an increased risk for developing the disease (6,13,16). Furthermore, in high endemic areas chemoprophylaxis has even been suggested and used for household contacts to reduce the risk for getting the disease (12,14). Like any other leprosy control program, contact examination has been one of the routine methods in case finding in China, including the Shandong province, since the leprosy control program started in the 1950's (1).
According to the "Guidelines for the Leprosy Control Program" issued by the Ministry of Public Health of China in 1975, household contact examination should be carried out for any newly diagnosed leprosy cases. Once a person in the family is diagnosed with leprosy, consecutive physical examinations for household members should be done once a year for 10 yrs for multibacillary (MB) leprosy patients and for 5 yrs for paucibacillary (PB) leprosy patients. This policy has not been changed much up to now, although the epidemiological situation of leprosy has changed dramatically. The "Manual of Leprosy Control" published recently still recommends that family members of a newly diagnosed leprosy patient should be physically examined yearly for up to 6 yrs (5). However, the negative impact of frequent contact examination is that it often creates social stigma for the disease, the patient, and the contacts being tested, which needs to be a concern (11).
The elimination of leprosy was achieved in 1994 in Shandong, a former endemic province located in the northeastern part of China, with a population of 90 million. The prevalence of leprosy remains as low as less than 0.1/10,000 and 50-70 new cases were detected each year in the past 10 yrs. In such a low endemic situation of leprosy in Shandong, what is the value of contact examination in terms of case finding? Should this policy in case finding of leprosy continue? And what is the other option in dealing with the problem? In order to address these questions, we retrospectively analyzed the data for all newly diagnosed leprosy patients in the past 11 yrs, using the data abstracted from the national leprosy recording and reporting system, and a questionnaire-based survey to see how many incident leprosy cases would be detected if we followed the policy for contact examination of leprosy in Shandong.
MATERIALS AND METHODS
Study population and definition. This study was based on all newly diagnosed leprosy cases from 1990 to 2001 in Shandong. A contact of leprosy patient can be defined as any person who has a history of contact with a known leprosy patient for any reasons. It can be a household member, a neighbor, a friend, or a co-villager. In the leprosy control program in Shandong province (as well as elsewhere in China), a contact generally means a household member, sometimes including relatives outside the family household of an index leprosy patient. In this study we categorized the contacts into three groups: (1) Relatives, which were sub-divided into first-, second- and third-degree family members according to the hereditary relationships, no matter whether they lived under the same roof or not, because we generally believed that they had more chance of contact with each other culturally; (2) Non-heredity-related contacts including neighbors and co-villagers; (3) Social contacts such as friends or a business associates outside of the village.
In the calculation of infectious sources for different categories of contacts, the following definitions were used. Index case means any newly diagnosed leprosy case during the study period from 1990 to 2001. Primary case is defined as any leprosy case which an index case reported to be an infectious source. If more than one leprosy case in the family had occurred, the last one was supposed to be the primary case in the calculation of the incubation period. Incubation period means the time from the onset of the disease of a primary case to the time when the onset of the disease of the index case was noticed.
Procedure of data collection. First, from the national recording and reporting system for leprosy, which was designed based on OMSLEP System (4), we abstracted all new cases diagnosed from 1990 to 2001. Then a questionnaire was designed and distributed to all the leprosy control institutions at the county level according to the information on the system. The local staff of leprosy control institutions at the county level filled in the questionnaires according to the information kept in the patients' files. We asked that the questionnaires be mailed back to our institute, where the data were entered into a database and analyzed with SPSS software version 10.0.
RESULTS
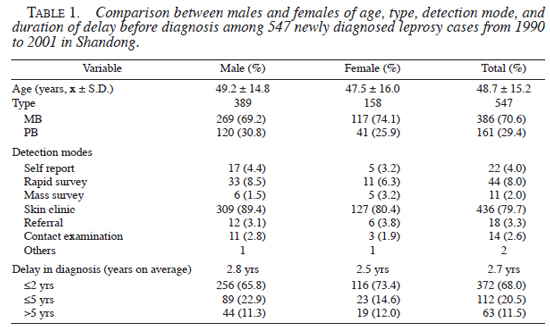
In the recording and reporting system, 558 newly diagnosed leprosy cases were registered during the period of 1990 to 2001. We received 547 questionnaires from 120 counties (there were no new cases in some former low endemic counties during the period). The majority (71%) of new cases were male, and were MB cases (70%). The most common detection method was through skin clinic (80%). Most cases (68%) were diagnosed within 2 yrs after the onset of the disease, with a mean delay duration of 2.74 ± 3.26 yrs, ranging from several months to 25 yrs. Male and female comparisons of age at diagnosis, leprosy type, detection mode, and duration of delay before diagnosis are presented in Table 1.
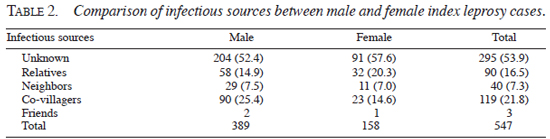
Among the 547 newly diagnosed leprosy cases, 295 (53.9%) cases reported that they had not known any contact with a leprosy case. Ninety (16.5%) index cases reported that they had a family background of at least one leprosy case in the family. One hundred sixty two (29.6%) index cases reported that they had contact with non-relative leprosy patients, which were either neighbors, co-villagers, or friends. The comparison of infectious sources between male and female index cases is shown in Table 2.
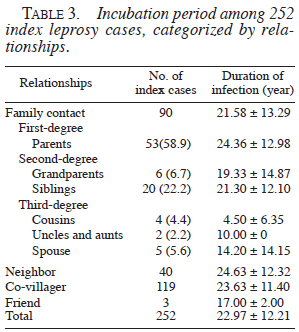
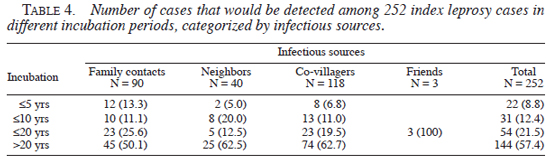
Among the 90 index cases with a family background of leprosy cases, the most common infectious sources were from the first generation (58.9%) and the second generation, including siblings (22.2%) and grandparents (6.7%). The incubation time among the 252 index cases, which had known contact with a leprosy patient, was 23 yrs on average, ranging from 1 yr to 55 yrs (Table 3 ). If we had followed the policy in household contact examination, only 12 index cases would have been detected. This constitutes only a small proportion (2.2%) of the newly diagnosed leprosy cases in the province from 1990 to 2001. The number of cases, which would be detected in different periods by infectious sources among 252 index leprosy cases, is presented in Table 4.
DISCUSSION
It is supposed that leprosy is at least as infectious as tuberculosis (9), but development of the clinical disease will depend on immunologically specific resistance of the individual to Mycobacterium leprae (M. leprae), which is, to a great extent, controlled by genetic host factors. The more frequent occurrence of leprosy in certain clusters, particularly family clusters, is well recognized (6,13). However, the most debated issue is whether this is due to the clusters sharing the same environment or the same genetic predisposition, or a combination of both. Practically, in contact examination of a leprosy patient in China, as well as in Shandong, "household members" not only means the people living under the same roof, but also includes relatives, especially the first-degree relatives, whether they actually live in the same house, or whether they lived together for a long period of time when contact examination was executed. In general, all relatives culturally keep close contact with family and social affairs in the society of Shandong. Therefore, it is reasonable to assume that they are more at risk for infection by the primary leprosy cases in the families.
Earlier and recent studies demonstrated that both the intimacy of contact and the type of disease played an important role in the transmission of the disease (6,13). However, in these studies the hereditary relationships between the index cases and their contacts were not clear. We speculate that the closer the contact of these persons, the more they are related to each other genetically, as is the case in Shandong. Therefore, both infection of M. leprae and immunological resistance to M. leprae determine the occurrence of the disease (9). An earlier seroprevalence study based on enzyme-linked immunosorbent assay (ELISA), using albumin coupled to synthetic disaccharide antigen to test for antibody, showed the proportion of ELISA positives among household and non-household relatives was not significantly different compared to that among neighbors (7). This evidence could not explain why the household contacts were at higher risk for developing leprosy than their neighbors, as demonstrated in some studies. Apparently, the shared immunological status of the relatives to M. leprae also plays a role, and makes the household contacts at higher risk for occurrence of the disease under the same prevalence of M. leprae infection.
On the other hand, the problem with the point of onset after exposure mainly relates to the clear identification of the source of the infection, which is not always easy, since the onset of the disease is insidious, with long incubation period. Furthermore, if there are several leprosy cases in the village, it is difficult to determine which one is the infectious source for a particular index case. In practice, routine household examination does not include neighbors and other people in the community, due to both the difficulty in determining contact outside of the family and stigma, although their contribution to the total number of new cases is greater than family contacts in this group of patients (Table 2 ).
Early detection and treatment has benefits not only for the termination of infection transmission, but also for the prevention of the disabilities of leprosy. However, in such a low endemic situation of leprosy in Shandong, active case finding such as mass survey and even rapid survey is no longer cost-effective (Table 1 ). Contact examination for household members is still compulsory for the leprosy control program in Shandong Province, according to the national guidelines of the leprosy control program in China. Our results showed that if all relatives of the primary leprosy patients were followed once a year for 5 yrs or 10 yrs, only 13.3% and 11% of the index leprosy cases would be detected, respectively (Table 4 ). If we define contacts as the people living in the same household, which often are parents, grandparents, and siblings, the proportion of index leprosy cases detected through contact examination would be even less than these figures.
From a leprosy control point of view, household contacts only contribute a small proportion of the total of new leprosy cases in the population. Their contribution is no more than 30% in a situation in which leprosy is highly or moderately endemic (10). The results in this study showed roughly 16% of the index leprosy cases could be related to household primary leprosy cases. In an analysis of the detection modes for newly diagnosed leprosy cases from 1981 to 1998 in China, the proportion of leprosy cases detected by contact examination alone accounted for only 8.7% to 9.1% of the total number of cases detected during the same period (3), whereas only 14 (2.6%) new cases were detected by contact examination in this group of patients (Table 1 ). Therefore, in such a low endemic situation of leprosy in Shandong, in terms of early diagnosis and treatment of leprosy, contact examination is not effective. Another important issue is that frequent contact examination often causes stigma and discrimination for the patient, and even the whole family, because it impresses upon the public that the disease is very infectious and incurable (11).
In spite of this, when a new case is detected, household contacts of the patient should be examined for evidence of leprosy once, then they should be educated on the early signs of the disease and their significance, and asked to return if any suspected skin lesions develop or motor or sensory changes occur (15). Another option in dealing with this problem is to strengthen training for health workers and dermatologists in skin clinics at different levels to pick up a few incident leprosy cases (2). In order to do this, a CD Rom with early signs of leprosy and diagnostic procedure is under preparation and will be presented in dermatological meetings and circulated in the province.
REFERENCES
1. Chen, S.M. Options for leprosy control program in Shandong Province, China. Thesis, Royal Tropic Institute, Amsterdam, 1995.
2. Chen, S.M., Han, C.L., Li, B., Zheng, R. and Zhang, L. A survey on knowledge and skills in the early diagnosis of leprosy in general health services at different levels in Shandong Province, The People's Republic of China. Lepr. Rev. 71(2000)57-61.
3. Chen, X.S., Li, W.Z., Jiang, C., Zhu, C.B. and Ye, G.Y. Studies on mode of detection of leprosy in China during the years 1981-1998. Lepr. Rev. 72(2001)302-310.
4. Chen, X.S., Li, W.Z., Jiang, C., Zhu, Z.L. and Ye, G. Computerization of leprosy records: national leprosy recording and reporting system in China. Lepr. Rev. 71(2000)47-56.
5. Chen, X.Y. Manual for Leprosy Control. Beijing: Science Press, 2002, p. 61
6. Fine, P.E., Sterne, J.A., Ponnighaus, J.M., Bliss, L., Saui, J., Chihana, A., Munthali, M. and Warndorff, D.K. Household and dwelling contact as risk factors for leprosy in northern Malawi. Am. J. Epidemiol. 146(1997)91-102.
7. Gonzalez-Abreu, E., Mora, N., Perez, M., Pereira, M., Perez, J. and Gonzalez, A.B. Serodiagnosis of leprosy in patients' contacts by enzyme-linked immunosorbent assay. Lepr. Rev. 61(1990)145-150.
8. Hastings, R.C. and Opromolla, D.V.A. Leprosy. 2nd edn. Edinburgh: Churchill Livingstone, Longman Singapore Publishers Pte Ltd., 1994.
9. Klatser, P.R. Strategies for pro-active case-finding in leprosy control. Lepr. Rev. 71(suppl.). (2000)S30-S32.
10. Noordeen, S.K. Prophylaxis-scope and limitations. Lepr. Rev. 71(suppl.). (2000)S16-S20.
11. Scott, J. The psychosocial needs of leprosy patients. Lepr. Rev. 71(2000)486-491.
12. Tin, K. Population screening and chemoprophylaxis for household contacts of leprosy patients in the Republic of the Marshall Islands. Inter. J. Lepr. 67(suppl. 4). (1999)S26-S29.
13. van Beers, S.M., Hatta, M. and Klatser, P.R. Patient contact is the major determinant in incident leprosy: implications for future control. Inter. J. Lepr. 67(2)(1999)119-128.
14. Vijayakumaran, P., Jesudasan, K., Mozhi, N.M. and Samuel, J.D. Does MDT arrest transmission of leprosy to household contacts? Inter. J. Lepr. 66(2)(1998)125-130.
15. WHO. Expert Committee on Leprosy. Seventh report. Geneva: World Health Organization, 1997. Tech. Rep. Ser. 874.
16. Xu, K. and Jiang, C. A preliminary approach on clustering of disease in leprosy families: application of probability density function model of poisson distribution. J. Chinese Dermatol. 13(5)(1984)9-11 (in Chinese).
Shandong Provincial Institute of Dermatovenereology, Shandong, China.
Received for publication on 15 October 2002.
Accepted for publication on 1 April 2003.