- Volume 71 , Number 2
- Page: 101–5
Ovarian function in female patients with multibacillary leprosy
ABSTRACT
Eighty six adult female patients with multibacillary leprosy were included to study the sex hormone profile LH, FSH, and prolactin, as well as their gynecological events like menstrual function and fertility status. Athird of the patients gave a history of irregularity of periods. The mean levels of LH and FSH were significantly higher in patients with multibacillary leprosy vis-à-vis the controls. Of the 24 married women with irregularity of periods, 12 (50%) were infertile. Seven of these patients had elevated levels of FSH and LH, almost reaching castration levels.RÉSUMÉ
Quatre vingt six patientes avec lèpre multibacillaire furent incluses dans une étude d'évaluation des profils hormonaux de LH, FSH et prolactine ainsi que d'évènements gynécologiques tels que les menstruations et la fertilité. Un tiers des patientes rapportèrent des règles irrégulières. Les concenterations moyennes de LH et de FSH étaient significativement plus élevés parmi les patientes multibacillaires que parmi les témoins. Parmi 24 femmes mariées avec règles irrégulières, 12 (50%) n'étaient pas fertiles. Sept de ces patientes présentaient des concentrations élevées de LH et de FSH, niveaux atteignant ceux observés après ovariectomie.RESUMEN
Se estudiaron, en 86 mujeres adultas con lepra multibacilar, los niveles de las hormonas LH, FSH, y prolactina, así como su estado ginecológico en cuanto a menstruación y fertilidad. Un tercio de las pacientes tuvieron una historia de periodos irregulares de menstruación. Comparadas con las mujeres control, los niveles promedio de LH y FSH en las pacientes con lepra multibacilar estuvieron significativamente elevados. De las 24 pacientes casadas con periodos irregulares, 12 (50%) fueron infértiles. Siete de estas pacientes tuvieron niveles elevados de FSH y LH, similares a los de castración.Leprosy is a multi-system infection, and leprous granulomata have been demonstrated in several organs such as the liver, lymph nodes, adrenals, bone marrow, and testis (1,3,4). The involvement of the male reproductive system in multibacillary leprosy has been studied extensively. The testis is commonly affected in leprosy, resulting in sexual dysfunction and testicular atrophy (3). The hypofunction of the testis is due to the acute inflammatory exudate, as well as due to the leprous granulomata (3), and results initially in sterility and later in impotence, as well. The levels of serum follicle stimulating hormone (FSH), leutinizing hormone (LH), and estrogens are elevated while levels of serum testosterone are depressed (6,10,11,14).
There is, however, a paucity of literature on the involvement of female reproductive organs in patients with leprosy. Though there is a report on "ovarian leprosy" quoted by Mitsuda (12,13), and a host of contradictory reports on the effect of leprosy on menstrual function (2,5,15), there is a dearth of information on the profile of sex hormones and ovarian function in female patients with leprosy. As a result, this study was undertaken, to assess the hormonal profile (serum levels of FSH, LH, and prolactin) and the menstrual function in patients with multibacillary leprosy.
MATERIALS AND METHODS
Patient selection. Eighty-six female patients between the ages 20-40 years, with clinically suspected multibacillary (borderline, borderline lepromatous, and lepromatous) leprosy attending the Leprosy Clinic of All India Institute of Medical Sciences, New Delhi, India were taken up for the study. The diagnosis of multibacillary leprosy was confirmed by a slit smear and histopathological examination, and in 24 patients additionally using delayed hypersensitivity to lepromin.
Exclusion criteria. Patients taking oral contraceptives, women who were pregnant, and any patient on anticancer chemotherapy/radiotherapy were excluded. Patients with confounding factors like anemia and a history of concomitant tuberculosis or overt tuberculosis on clinical examination were also excluded from the study.
Methods. Apart from history pertaining to their disease, the patients were interrogated in depth about their menstrual history, including age of attaining menarche, regularity, and flow of periods. Any alteration of menstrual periods in relation to leprosy, if any, was noted. In married females, a detailed obstetric history and the course of pregnancy/leprosy were noted. All patients were examined in detail, with special attention being given to the physical development of secondary sexual characteristics. In patients with irregular periods, an ultrasonographic examination of the pelvis was done. In all patients, an estimation of serum LH, FSH, and prolactin was done by radio-immunoassay (using Immunoteck kits). In women with regular periods, the blood sample for hormone estimation was taken in the early follicular phase, while in those with irregular cycles, the sample was taken at any time of the menstrual cycle. Fifty age-matched controls who had no menstrual irregularities were also bled for hormone estimation in the early follicular phase. Informed consent was taken both from the patients and controls.
Statistical analysis. Descriptive statistics (mean and standard deviation and frequency distribution) were calculated for the continuous and discrete variables, respectively. The differences between cases and controls, and within cases according to categories (fertile/infertile and regular/irregular periods), were statistically evaluated using students' t-tests (unpaired), taking p value for unequal variance. To determine the association between the regularity of periods and fertility, a chi square test was applied between the cases and controls. A p value of <0.05 was considered as statistically significant.
RESULTS
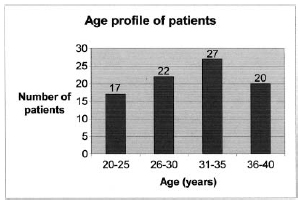
A total of 86 female patients, between the ages 20-40 years, were taken up for the study. The age profile of the patients is shown in Fig. 1. Twenty (23.25%) patients were unmarried, 2 (2.32%) were separated or divorced from their husbands (and will be considered single for the purpose of analysis), while 64 (74.42%) were married.
Thirty three (38.37%) patients were diagnosed as having Borderline borderline leprosy (BB), while 43 (50%) were diagnosed as having borderline lepromatous (BL) leprosy, and 10 (11.63%) were diagnosed as having lepromatous leprosy (LL). In 24 patients, the diagnosis was based on clinical, histological, immunological (lepromin), and bacteriological parameters, while in 62 patients the final diagnosis was based only on clinical, histological, and bacteriological parameters because lepromin tests could not be done due to shortage of availability of the antigen.
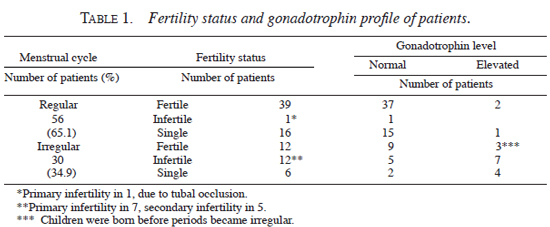
All patients, save one, had attained menarche at a normal age, and all patients had developed secondary sexual characteristics normally. Thirty (34.9%) women, however, gave a history of irregularity of periods. In 26 patients, the irregularity of periods started 1-6 yrs after the onset of leprosy. Six of the patients who had irregular periods were unmarried (or separated from their husbands) and their fertility status could not be ascertained. Of the 24 married women with irregular periods, 12 (50%) were infertile; seven (29.1%) having primary infertility while 5 (20.8%) had secondary infertility. Seven (29.1%) of the 12 patients who had infertility, had elevated levels of FSH and LH almost reaching castration levels, while 1 patient had evidence of tubal occlusion. All other 12 patients with irregular periods who had children, had conceived before their periods had become irregular. Of the 56 patients with regular periods, only 1 patient had primary infertility and, on further investigations, was found to have tubal occlusion. Two other patients had elevated levels of FSH, LH, and prolactin. Both these patients conceived before the onset of their leprosy lesions. The fertility status and the gonadotrophin profile of the patients with irregular periods, vis-à-vis those with regular periods, is shown in Table 1.
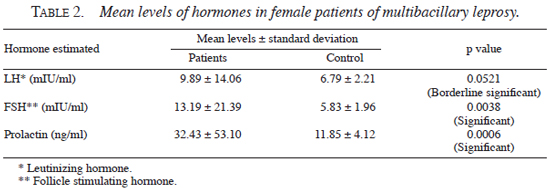
The mean levels of hormones in the patients and the controls are shown in Table 2. Though the mean levels of LH, FSH, and prolactin were all elevated in patients with multibacillary leprosy vis-à-vis the controls, the difference between cases and controls was statistically significant only in cases of serum LH and FSH levels (p <0.05).
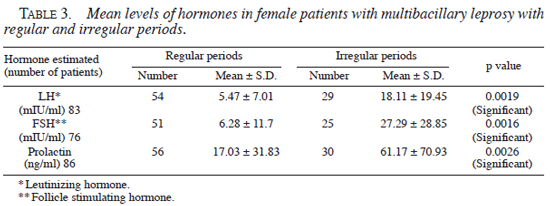
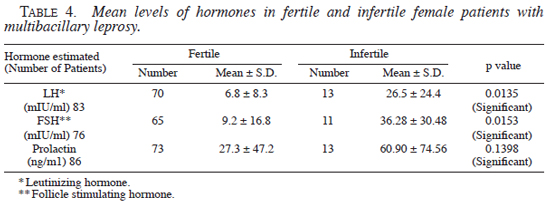
When we compared the levels of FSH, LH, and prolactin in patients of multibacillary leprosy with regular and irregular periods, there was statistically a highly significant elevation of mean levels of all hormones in patients with irregular periods, vis-à-vis patients with regular periods (Table 3 ). Similarly, the levels of FSH and LH were statistically significantly higher in patients with infertility, vis-à-vis those who were fertile (Table 4 ).
DISCUSSION
Leprosy is a multisystem infection in which leprous granulomata have been demonstrated in several organs like testis, liver, adrenals, lymph nodes and bone marrow (1,3). Gonadal involvement in males with lepromatous leprosy is very common and results in sexual dysfunction and testicular atrophy. The testicular dysfunction has been attributed to the acute inflammatory exudate and edema, and subsequent fibrosis, which occurs in leprous orchitis. Desikan and Job (3) showed that the testis is usually small, firm, and atrophic and the cut surface shows a fibrotic white appearance. Initially, the exocrine portion atrophies and this leads to sterility, and later when the interstitial cell atrophy occurs, the patients complain of impotence.
Garg, et al. (6), in a study on the hormone profile in male patients of leprosy without any clinical manifestation of testicular dysfunction, found that the levels of serum FSH, LH, and estrogen were elevated, while the level of serum testosterone was depressed in lepromatous leprosy. Several other studies have also corroborated this hormonal imbalance in male patients with leprosy (11,14). High levels of serum FSH have been attributed to damage of the seminiferous tubules by Koshy, et al. (10).
There is, however, a paucity of literature on the involvement of the female gonads in patients of leprosy. Mitsuda (12,13) described the occurrence of lepra cells in the endometrium, fallopian tubes, and in the capillaries of the vaginal mucosa, but completely ruled out that leprosy in women can cause sterility.
Flegar, et al. (5) found that 54% of the cases studied by them were sterile while 35% of the patients reported scanty periods. King and Marks (9) also reported gross menstrual abnormalities in patients of leprosy, but they did not study the hormonal profile of these patients. Bogush (2) reported that the early institution of therapy could prevent menstrual dysfunction, but did not comment on the fertility status of his patients.
Hardas (7) noted that though obstetric events could alter the course of leprosy, leprosy had no effect on gynaecological events like menstrual cycle or fertility in their patients. Interestingly, only 18% of their patients' endometrial biopsies in the premenstrual phase showed secretory phase, indicating that though fertility was not affected, there was some hormonal imbalance. Sharma, et al. (15), in a recent study of 35 adult female patients with bacillary positive leprosy, found that leprosy had no direct effect on menarche, menstrual cycle, fertility, and menopause. Significantly, 3 (8.57%) of their lepromatous leprosy patients had never conceived. Though little is known about the level, pattern, and determinants of infertility in women in India, a prevalence of 6% has been mentioned (8).
In our study, all patients (except 1) had attained menarche at a normal age. All patients had normal development of secondary sexual characteristics. A third of the patients, however, gave history of irregularity of periods. Interestingly in 26 patients, the irregularity of periods started 1-6 yrs after the onset of leprosy. Six of the patients who had irregular periods were unmarried (or separated from their husbands). Of the 24 married women, 12 (50%) were infertile; of these 7 (29.1%) had primary infertility and 5 (20.8%) had secondary infertility. There was a strong correlation between infertility, irregular periods, and elevated levels of LH, FSH, and prolactin. The 12 patients, with irregular periods who had children, had conceived before their periods had become irregular. Seven (29.1%) patients who had infertility also had elevated levels of FSH and LH almost reaching castration levels. The mean levels of FSH and LH were significantly higher in patients with multibacillary leprosy vis-à-vis the controls.
Of the 56 patients who had regular periods, 16 were unmarried. Only 1 patient was infertile and she had evidence of tubal occlusion. There were 2 other patients who had elevated levels of FSH and LH, but they had conceived long before the onset of their leprosy lesions.
The findings of this study are significant in view of the fact that it is generally believed that ovarian dysfunction does not occur in leprosy. However, none of the earlier studies looked at the hormonal levels of female leprosy patients, and the present study distinctly shows that even in the absence of confounding factors like anemia and tuberculosis, leprosy may be associated with menstrual irregularities, infertility, and elevation of gonadotropin hormones.
Acknowledgments. We acknowledge the help provided by Dr. Khurana, Department of Endocrinology, in carrying out the hormonal assays. We appreciate the secretarial assistance provided by Mr. Any Chacko, Mr. M. John, and Ms. Meenu Kohli in typing the manuscript.
REFERENCES
1. Bernard, J.C. and Vazquez, C.A.J. Visceral lesions in lepromatous leprosy. Study of sixty necropsies. Int. J. Lepr. 41(1973)94-101.
2. Bogush, T.G. The question of the menstrual function in women with lepromatous leprosy before pubescence. Sci. Works Lepr. Res. Institute. 9(1976)116-118.
3. Desikan, K.V. and Job, C.K. Visceral lesions caused by M leprae; a histopathological study. Indian J. Path. Bact. 23(1969)123
4. Dharmendra and Ramu, G. Some systemic manifestations of leprosy. Int. J. Lepr. 49(1981)68-71.
5. Fleger, J., Biric, B. and Prica, S. Importance of leprosy in gynaecology and midwifery. Trop. Dis. Bull. 60(1963)446-447.
6. Garg, R., Agarwal, J.K., Singh, G. and Bajpai, H.S. Hormone profile in leprosy. Indian J. Lepr. 61(1989)428-439.
7. Hardas, U., Survey, R. and Chakravarty, D. Leprosy in gynaecology and obstetric. Int. J. Lep. 40(1972)399-400.
8. Jejeebhoy, S.J. Infertility in South Asia: priorities for social science research. In: Issues in Women's Reproductive Health. Baroda: Population Council, 1995, pp. 117-165.
9. King, J.A. and Marks, R.A. Pregnancy and leprosy. Am. J. Obstet. Gynaecol. 76(1958)438-442.
10. Koshy, T.S., Rolston, R., Mathews, M. and Taylor, P.M. Hormone profile in lepromatous leprosy. Int. J. Lepr. 49(1981)31-36.
11. Martin, F.R., Maddocks, I., Brown, J.B. and Hudson, B. Leprous endocrinopathy. Lancet. (ii) (1968)1320-1321.
12. Mitsuda, K. The significance of the vacuole in the Virchow lepra cells and the distribution of lepra cells in certain organs. Int. J. Lepr. 4(1936)491
13. Mitsuda, K. and Ogawa, M. A study of 150 autopsies on cases of leprosy. Int. J. Lepr. 5(1937)50
14. Morely, J.E., Distiller, L.A., Sagel, J., Kok, S.H., Kay, G., Carr, P. and Katz, M. Hormone changes associated with testicular atrophy and gynaecomastia in patients with leprosy. Clin. Endocrinology. 6(1977)299-303.
15. Sharma, S.C., Kumar, B., Dhall, K., Kaur, S., Malhotra, S. and Aikat, M. Leprosy and the female reproductive organs. Int. J. Lepr. 49(1981)177-179.
1. M.D., Additional Professor, Department of Dermatology and Venereology;
2. M.D., Department of Endocrinology;
3. M.B.B.S., Department of Dermatology and Venereology;
4. M.D., Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi - 110 029, India.
Reprint requests to: Khanna Neena, Additional Professor Department of Dermatology & Venereology, All India Institute of Medical Sciences, New Delhi - 110 029, India.
Tel: 91-11-4350514/4353898; Fax: 91-11-4352665; E-mail: akhanna@mantraonline.com
Received for publication on 17 May 2002.
Accepted for publication on 9 March 2003.