- Volume 65 , Number 2
- Page: 230–7
Fixed-duration multidrug therapy in multibacillary leprosy
ABSTRACT
Six-hundred-fifty-seven active multibacillary (MB) leprosy patients were put on fixed-duration multidrug therapy (FD-MDT) between 1985 and 1992 (190 had had no and 235 had had previous treatment with dapsone) and were followed for 5 years after therapy. Two relapses occurred during year 5 of surveillance and both had received dapsone prior to chemotherapy, giving an overall relapse rate of 0.08/100 person-years (py). Excluding the two relapses, 99.4% of the MB patients converted to smear negativity at year 6 after a regular course of FD-MDT. The relapse rate for 35 MB patients with an initial bacterial index (BI) of >4 with 5 years of surveillance was 0.24/100 py. Reactions occurred more frequently during the first 6 months of MDT, decreasing gradually thereafter, and reaching 0 in year 4 of surveillance. The deformity rate at intake was 22.7% and only 1.8% of MB patients developed new deformities or an increased grade in deformity during therapy.RÉSUMÉ
Six cent cinquante-sept patients lépreux multibacillaires (MB) ont été mis sous polychimiothérapie d'une durée fixe (PCT DF) entre 1985 et 1922 (190 d'entre eux n'avaient eu aucun traitement antérieur et 235 avaient eu un traitement antérieur à la dapsone), et ont été suivis pendant 5 ans après le traitement. Deux rechutes sont survenues durant la cinquième année de la surveillance, et toutes deux avaient reçu un traitement à la dapsone antérieur à la PCT, donnant un taux de rechute global de 0.08/100 personnes-années. Si on exclut ces deux rechutes, 99.4% des patients MB sont devenus négatifs aux frottis cutanés à la sixième année après la PCT DF. Le taux de rechute pour 35 patients MB avec un index bactérien initial (IB) de plus de 4 avec cinq ans de suivi était de 0.24/100 personnesannées. Des réactions sont survenues plus souvent pendant les six premiers mois de PCT, ont diminué par la suite, et ont disparu à la quatrième année de suivi. Le taux d'incapacité au départ était de 22.7% et seulement 1.8% des patients MB ont développé de nouvelles incapacités ou ont aggravé leur score durant le traitement.RESUMEN
Entre 1985 y 1992, 657 pacientes con lepra activa multibacilar (MB) se sometieron a tratamiento con poliquimioterapia de duración fija (PQT DF), y se mantuvieron bajo supervisión durante 5 años después de la misma. Ciento noventa pacientes habían tenido tratamiento previo con dapsona y 235 no habían sido tratados con la droga. Durante el año 5 del seguimiento, dos pacientes que habían recibido dapsona antes de la PQT presentaron recaída, lo que representa una frecuencia global de recaída de 0.08/100 personaaños (pa). Excluyendo estos dos casos, el 99.4% de los pacientes MB se hicieron baciloscópicamente negativos en el año 6, después de un curso regular de PQT DF. La tasa de recaída para 35 pacientes MB con un índice bacteriano inicial (BI) de >4 con 5 años de seguimiento, fue de 0.24/100 pa. Las reacciones ocurrieron más frecuentemente durante los primeros 6 meses de PQT, disminuyendo gradualmente después, y alcanzando O en el año 4 del seguimiento. La tasa de deformidad inicial fue del 22.7'7r y durante el tratamiento sólo el 1.8% de los pacientes MB desarrollaron nuevas deformidades o incrementaron el grado de las ya existentes.When multidrug therapy (MDT) was introduced in 1982, because of the time in years required to determine the risk of relapse in leprosy, the World Health Organization (WHO) recommended that "combined therapy be given for at least two years and be continued, wherever possible, up to smear negativity" (10). With the purposes to enhance leprosy control and to achieve the national goal of eliminating leprosy (prevalence of 0.1/10,000/county, Guangzhou 1981) (3) within this century, we established a field study in 1983 involving two independent teams on the therapeutic effect of MDT by ending the regimen for active multibacillary (MB) patients after 24-27 monthly dosages (fixed-duration or FD-MDT). At the annual clinical and bacteriological surveillance, it was noticed that the clinical appearance of lesions, routine smear examinations and the specific histopathological findings continue to improve after the termination of MDT (4). Encouraged by these preliminary results and with the aim to confirm these findings for wider application, the present study was planned to cover 500 MB leprosy patients to study the relapse rates after FD-MDT, the critical bacterial index (BI) before MDT which is necessary to prevent relapse, and if relapse occurs, if the patient can still be treated effectively with FD-MIT.
MATERIALS AND METHODS
This study is part of a larger project assisted by WHO, the Leprosy Control Program with FD-MDT in Yunnan, Guizhou and Sichuan Provinces which was initiated in 1985 covering some of the most difficult terrain and the most leprosy-prevalent areas in China.
The original plan was to select 500 active MB patients who may have had some years of irregular dapsone treatment but never had received rifampin before MDT in Liangshan and Panzhihua Prefectures, Sichuan Province. All MB patients admitted to the study were checked clinically, bacteriologically and confirmed histopathologically by the specialized staff of the Provincial Institute of Dermatology (PIOD), Chengdu. Routine drug delivery, supervision of monthly drug intake as well as clinical examinations were carried out by the leprosy workers (LW) From the 20 County Skin Disease Control Stations (SDCS) (The Figure). After 12 months of MDT and again at the time of completing the 24-month course of FD-MDT in 36 months (i.e., at least 75% of daily drug intake/month, 75% monthly supervised drug intake/year), the above examinations were repeated by the staff of the PIOD. All MB patients admitted to the present study meet the above criteria of regularity, and >95% of the MB patients completed MDT by the end of 2 years. An annual surveillance with clinical and slitskin smear examinations was performed by the respective county LW, and if severe leprosy/drug reactions or suspected relapses were detected, the PIOD was notified and verification of the diagnosis and treatments given at the SDCS. In severe cases such services were provided at the patient's home, usually within 2-4 weeks. A few patients with severe leprosy reactions were admitted to the township health center or county leprosy hospital.
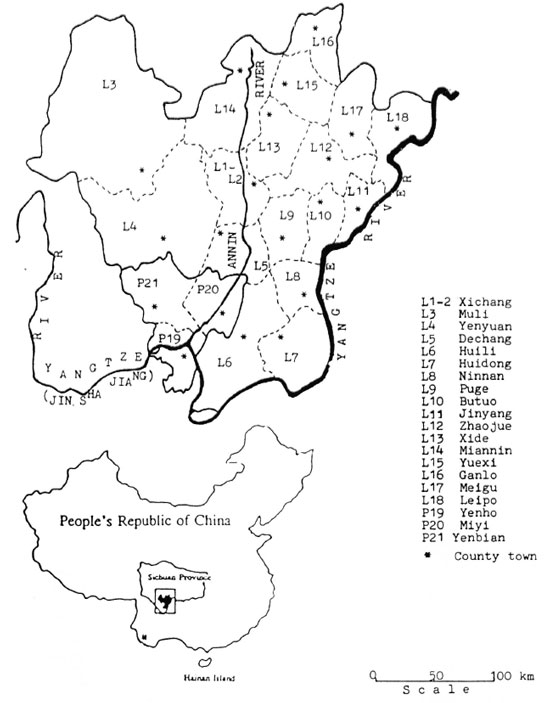
The Figure. Counties of Liangshan and Panzhihua Prefectures, Sichuan Province, China.
All confirmed relapses were required to complete a special form with all the relevant data before, during and at the end of MDT, plus data at each annual follow-up examination by the leprologist From the PIOD.
Criteria of relapse: insidious appearance of new lesions, enlargement of old lesions, increase of acid-fast bacilli (AFB) >2+ From the same site of the previous examination and positive histopathology.
All data on MB patients admitted to this study were entered into the databank of the PIOD in Chengdu and compiled and analyzed in Beijing. Relapse rates were calculated by mean rates per person-years (py) of observation and the cumulative probability of relapse by annual cohorts completing 24 months of MDT. During this study the reactional episodes in relation to FD-MDT was also studied. All data were analyzed by age, sex, type and by dapsone therapy before FD-MDT.
RESULTS
Between 1986 and 1994 all together 657 active MB patients (402 without and 255 with previous dapsone treatment) were admitted From the 17 counties of Liangshan and three counties of Panzhihua Prefectures of Sichuan Province. The male/female ratio is 4:1 (323/79) for MB patients without and 6:1 (218/37) for MB with previous dapsone therapy. Until the end of 1995, only 190 MB patients without and 235 MB patients with previous dapsone met the required surveillance period of 5 years (8).
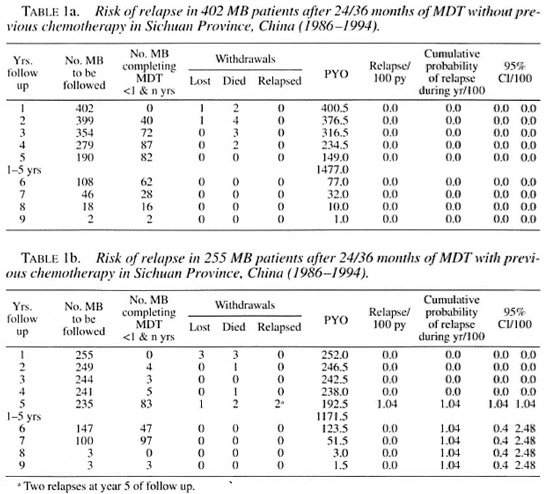
Surveillance and relapse. The mean relapse rate is 0/100 py for MB patients without (0/1477 py) and 0.17/100 py (2/1172 py) of observation in MB with previous dapsone at year 5 after FD-MDT. The cumulative probability of relapse is 0 and 1.04/100, respectively, for the same period (Table la and b). The two relapses were successfully retreated with FD-MDT.
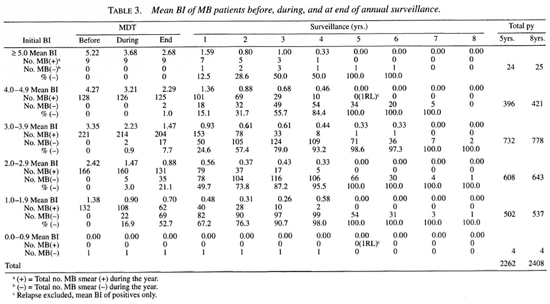
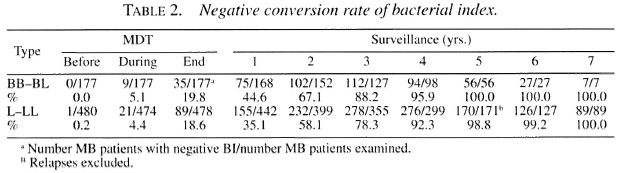
Decrease of BI after FD-MDT. The Bl-negative conversion rate for the nonre-lapsed patients reached 99.6% (226/227) at year 5 of follow up; one LL patient remained at Bl 0.33 in years 5 and 6 after MDT, and was not yet examined for year 7 of surveillance. The Bl-negative conversion rate is faster in borderline than in lepromatous patients (Table 2); excluding the two relapses and the LL patient mentioned above, all MB patients converted to negativity at year 5 of surveillance, irrespective of the initial BI value (Table 2).
Relapse and BI before FD-MDT. There were 35 MB patients with an initial BI of >4.0 who have been followed for 5 years, and only one relapse occurred, giving a relapse rate of 0.24/100 py (1/420 py). If the total follow-up period for MB patients with a BI of >4.0 is considered, the relapse rate is 0.22/100 py (1/446 py). Counting all MB patients with a BI of >3.0 before MDT, the relapse rate is 0.08/100 py (1/1224 py).
The other relapse was initially BI negative (M24, histopathology L, AFB 1+), remained smear negative during the first 4 years after MDT, developed facial infiltration plus more macules and nodules than before FD-MDT with a BI of 2.834-at year 5 of follow up. Both relapses had taken dapsone irregularly (20 and 5 years, respectively) before MDT (Table 3).
Leprosy reactions. Reactions occurred more frequently during the first 6 months (12%), decreasing gradually From months 7 to 24 of MDT, rose significantly and more for reversal reactions during the first year after MDT, finally reaching 0 in year 4 of surveillance (Table 4).
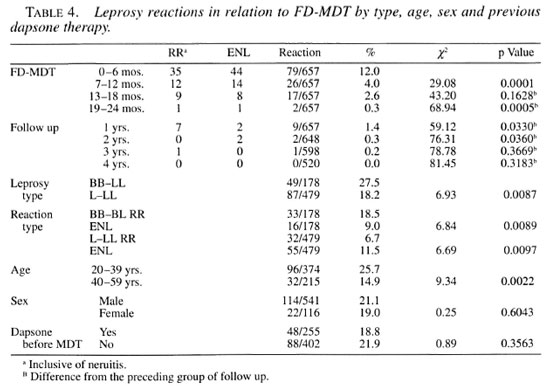
As expected, there were significantly more reactions and, particularly, reversal reactions in borderline and erythema nodosum leprosum (ENL) reactions in lepromatous leprosy. No significant differences in reactions were noticed by sex or by dapsone therapy before MDT, but significantly more reactions occurred in the 20-39 age group than in the 40-59 age group in the present study (Table 4).
Reactions were treated with prednisone (30-60 mg/day), gradually tapering off within 6 months. Severe reactions, plus two patients (M46 LL, BI 4.75; F29 BL, BI 2.75) with laryngeal edema 15-19 months after the first dose of MDT, received hydrocortisone 300 mg/day intravenously for 7-14 days, and were subsequently successfully treated with prednisone. Some ENL reactions received thalidomide 200-300 mg/day in addition to prednisone.
All together 20.2% (133/657) of the MB patients had reactions at some time during this study; whereas in Xichang County, where the training course on MDT was conducted (14-23 November 1985), field work was comparatively of a higher standard and significantly more reactions (25/73 = 34.2%, p <().()05) were diagnosed.
New deformities. The overall deformity rate (WHO sirade II + III, 1980) when MDT was prescribed was 22.77* (149/657), with more deformities in MB patients (79/255 = 31 %) who had had dapsone therapy before MDT. More deformities were found on hands (102/149 = 69%) than on other sites. During the course of MDT, 1.8% of the MB patients (12/657) developed new deformities, and more new deformities or an increased grade of deformity developed on the hands (13) than in the eyes (3) or on the feet (4). A program for the prevention of deformity in these two prefectures was introduced 4 years later in 1990.
Leprosy in children. All together there were 10 children (1.5%) in this MB group of patients. The mean age was 11.2 years (range 7-14 years); mean BI 2.96+ (range 1.25-4.2). One child (F9, BI 2.2, H-P BL 4+) had a grade II deformity of the left hand. All diagnoses were confirmed by histopathology and nine children had 4-6+ AFB in their biopsies. They were all successfully treated with FD-MDT.
Drug reactions. Eleven patients developed hypersensitivity reactions to dapsone (dermatitis 4, exfoliative dermatitis 4, dapsone syndrome 3) and all were treated with prednisone and subsequently received 24 months of rifampin plus clofazimine. Three patients developed liver damage with abnormal liver function tests after 3-20 months'administration of MDT. They received palliative therapy for liver damage and MDT was continued after a temporary break. Another patient had a gastro-enteric problem after 1 month of MDT and the gastro-intestinal symptoms recurred when MDT was resumed. He was changed to monthly rifampin plus daily dapsone therapy.
DISCUSSION
The long-term effects of 24 months of MDT in MB leprosy patients have stimulated wide interest in the last few years (1,2,4-7,9) Because of the uncertainty about late relapses, we have advised our teams to follow a MB patient for 10 years after FD-MDT if the patient showed marked clinical improvement and a decrease in the BI of >1.0 at the end of therapy. In the present study only 66% (425/657) of MB patients reached the limit of 5 years' surveillance (8). Two relapses occurred in year 5 of follow up, giving an overall relapse rate of 0.08/100 (2/1477 +1172) person-years of observation, which is much lower than the world-wide figure of 0.23/100 py, and the relapse occurred later than the figure that 50% of relapses occur within the first 3 years after stopping MDT (9).
A high initial BI does not seem to predispose to relapse. Thirty-six MB patients with an initial BI of >4.0 were followed for 5 years and only one relapse occurred. The overall relapse rate for 137 MB patients with an initial BI of 4.27-5.22 is 0.2/100 py (1/439 py) of observation. It is hard to explain the difference From the high relapse rate reported by Jamet, et al.: seven relapses occurred in 35 MB patients with a BI of >4.50 between 2 to 7 years after 2 years of MDT (1). On the other hand, a study in India on 11 LL patients with a BI of 3.2-4.4 before MDT showed that although they were AFB positive in skin and lymph nodes after 5 years of dapsone supplemented with 2 years of MDT, there was no growth in the foot pads of mice inoculated with AFB From these patients (7). It is known that the prevalence of leprosy is inversely associated with socioeconomic development (3); perhaps poverty not only predisposes to the disease itself but also to an increased possibility of relapse after an effective course of chemotherapy. The living standard of the MB patients reported earlier (4) has risen and their nutrition has much improved since being declared "cured" in May 1985 (11). No relapses were detected for year 10 of surveillance after FD-MDT in the 43/47 MB patients (91% survey, four deaths due to other causes) examined in Menla County, Yunnan Province, in January 1996. In the same study in Weifang, Shandong Province (4), no relapses were detected in the 25/33 MB patients (76% survey, six deaths and two emigrations) 10 years after FD-MDT (unpublished data).
Although the mean relapse rate between MB patients without previous dapsone therapy (0/100 py) and MB patients who had had varying periods of dapsone monotherapy (0.15/100 py) before FD-MDT is of no statistical significance (p = 0.12), nevertheless it might be interesting to test for drug sensitivity in these two relapses, even though they may be successfully retreated with FD-MDT.
It is unfortunate that 12 MB patients developed new/increased deformities at the end of MDT. Prevention of disability is difficult to introduce in the field once the MDT program is already in progress, especially if there are only one or two patients in the village in this mountainous, socioeconomically less-advanced area with a high rate of illiteracy.
The low child rate (1.5%) but high Mycobacterium leprae load in the 10 MB children detected is alarming. Some of these children may have been infected before MDT was introduced, and the three MB children <10 years of age had apparently been infected From "hidden," undetected cases of leprosy. The last known child case (F9, LL, BI 4.16) was put on MDT in February 1990. Leprosy control before MDT in these two prefectures was unsatisfactory as evidenced by the disproportionate male/female ratio (6:1) for MB patients having had previous dapsone therapy. More emphasis on contact examination and more training in the examination for early lesions in children and females are called for.
Competent, experienced leprosy workers are an invaluable asset to any leprosy control program, and they should be maintained on the job as long as possible, even when the elimination goal has been reached.
Acknowledgment. This study is supported by the UNDP/ World Bank/WHO Special Programme for Research and Training in Tropical Diseases. We are deeply grateful to the late Dr. M. Christian who drafted the manual of leprosy control with MDT and to Dr. R. R. Jacobson who conducted, together with Dr. Christian, the MDT Training Course. In addition Dr. Jacobson's visits to Xichang for reviewing the progress and his advice on reactions for these patients are appreciated. Thanks also go to Yuan Lian-Chao for assisting in the statistical analysis.
REFERENCES
1. JAMET, P., JI, B. and THE MARCHOUX CHEMOTHERAPY STUDY GROUP. Relapse after long-term follow up of multibacillary patients treated by WHO multidrug regimen. Int. J. Lepr. 63(1995)195-201.
2. Li, H.-Y. Problems of leprosy relapse in China. Int. J. Lepr. 61(1993) 1-7.
3. Li, H.-Y. WENG, X.-M., TONG LI, ZHEN, D.-Y, MAO, Z.-M., RAN, S.-Pand Liu, F.-W. Long-term effect of leprosy control in two prefectures of China, 1955-1993. Int. J. Lepr. 63(1995)213-221.
4. Li, H.-Y, Yu, X.-L., ZHANG, M.-S., DUAN, C.-X., HUANG, W.-B., ZHANG, S.-B., ZHU, K. and MA, J.-F. Short-term multidrug therapy in multibacillary leprosy-review of 80 cases in two provinces of China (1983-1988). Int. J. Lepr. 57(1989)622-627.
5. MARCHOUX CHEMOTHERAPY STUDY GROUP. Relapses in multibacillary leprosy patients after stopping treatment with rifampin-containing combined regimens. Int. J. Lepr. 60(1992)525-535.
6. PONNIGHAU.S, J. M. and BOERRIGTER, G. Are 18 doses of WHO/MDT sufficient for multibacillary leprosy; results of a trial in Malawi. Int. J. Lepr. 63(1995)1-7.
7. SIVAPRASAD, N., SNEHALATHA, S., LOBO, D., ASCHHOFF, M. and JOB, C. K. Viability of Mycobacterium leprae in lepromatous patients after five years of dapsone monotherapy supplemented with two years of multidrug therapy. Indian J. Lepr. 67(1995)427-433.
8. WHO EXPERT COMMITTEE ON LEPROSY. Sixth report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
9. WHO LEPROSY UNIT. Risk of relapse in leprosy. Indian J. Lepr. 67(1995)13-26.
10. WHO STUDY GROUP. Chemotherapy of leprosy for control programs. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
11. ZHAO, Z.-Y. [Develop new path and get rid of poverty.] China Lepr. J. 12(1996)122.
1. H.-Y. Li, M.D., M.P.H., Senior Researcher, Beijing Tropical Medicine Research Institute, 95 Yong An Lu, Beijing 100050, China.
2. L.-F. Hu, M.D., Director; Bacteriologist, Sichuan Provincial Institute of Dermatology, Changdu, Sichuan Province, China.
3. J.-S. Luo, M.D., Histopathologist; Bacteriologist, Sichuan Provincial Institute of Dermatology, Changdu, Sichuan Province, China.
4. X.-M. Liu, B.S., Bacteriologist, Sichuan Provincial Institute of Dermatology, Changdu, Sichuan Province, China.
5. P.-W. Wu, M.D., Team Leader (retired), Xichang County SDCS, Liangshan, Sichuan Province, China.
Received for publication on 8 July 1996.
Accepted for publication in revised form on 6 January 1997.