- Volume 65 , Number 3
- Page: 328–36
Progress of impairment scores following commencement of chemotherapy in multibacillary leprosy patients
ABSTRACT
Study aim: To investigate the progress of impairment over time in multibacillary (MB) leprosy patients. Study design: Retrospective cohort study. Study population: One-thousand-eightytwo MB patients newly registered in nine field clinics in the Western Region of Nepal between 1980 and 1993. Methods: Data on impairment at diagnosis and at yearly intervals afterward were collected f rom patient records of MB patients already released f rom multidrug therapy (MDT). The World Health Organization (WHO) 1988 "disability" grading scale (0- 2, for both eyes, hands and feet-six sites) was used as a measure of impairment. For the analysis we summed the WHO grading for the six sites into an eyes-hands-feet (EHF) sum score (minimum 0, maximum 12). The EHF score at 2 years of follow up was used to compute the main outcome measures: impairment at 2 years, yes or no, and deterioration of impairment compared with diagnosis. The combined effect of age, sex, classification and impairment status at diagnosis on the outcome was examined with logistic regression. Results: At diagnosis, 55.8% of the patients had some impairment. This proportion decreased over 2 years to 43.9%. Among patients without initial impairment, 31/310(10%) developed impairment during the study period. This was 81/396 (20.5%) among patients with impairment at diagnosis. The adjusted odds ratio (OR) for developing impairment was 1.87 [95% confidence interval (CI) 1.06-3.32J for patients with initial sensory impairment (WHO grade 1) and 1.98 (95% CI 1.15-3.4) for those with initial visible deformity (WHO grade 2). Among patients with impairment at diagnosis, 195/396 (49.2%) had improved after 2 years. Conclusions: The proportion of patients with impairment after 2 years of antileprosy treatment was 12% less than at diagnosis. Among patients without initial impairment, 10% had developed some impairment after 2 years. The risk of developing impairment was almost double for those with sensory impairment or visible deformity at diagnosis. For purposes of monitoring, evaluation and planning, both the proportion of patients with sensory impairment (WHO grade 1) and the proportion with visible deformity (WHO grade 2) should be reported at diagnosis and at reléase f rom treatmcnt.RÉSUMÉ
But de l'étude: analyser la progression des incapacités avec le temps chez des malades présentant une lèpre multibacillaire (MB). Protocole: Etude de cohorte rétrospective. Population d'étude: Mille quatre-vingt-deux patients MB nouvellement enregistrés dans neuf centres dans la région Ouest du Népal entre 1980 et 1993. Méthodes: Les données sur les incapacités au diagnostic et ensuite à intervalles annuels ont été récoltées à partir des fiches de patients de malades MB déjà libérés de la polychimiothérapie (PCT). L'échelle de gradation des incapacités de l'Organisation Mondiale de la Santé (OMS) de 1988 (0-2 pour les deux yeux, mains et pieds - six sites) a été utilisée comme mesure d'incapacité. Pour l'analyse, nous avons fait la somme des scores OMS pour les six sites pour obtenir un score total yeux-mains-pieds (YMP) (minimum 0, maximum 12). Le score YMP après 2 ans de suivi a été utilisé pour calculer les principales mesures de devenir: présence d'incapacités à 2 ans, oui ou non, et détérioration de l'état du point de vue incapacités par rapport au moment du diagnostic. L'effet combiné de l'âge, du sexe, de la classification et du statut d'incapacité à la détection sur le devenir final a été analysé par la méthode de régression logistique. Résultats: Au diagnostic, 55,8% des patients avaient une certaine incapacité. Cette proportion a diminué en 2 ans à 43,9%. Parmi les patients sans incapacité au départ, 31/310 (10 %) ont développé une incapacité au cours de la période d'étude. Cette proportion était de 81/396 (20,5 %) chez les patients qui présentaient une incapacité au moment du diagnostic. Le rapport de cotes ajusté pour le développement d'incapacités était 1,87 [limites de confiance à 95 % (LC) 1,06-3,32] pour les patients avec une capacité sensorielle initiale (grade 1 de l'OMS) et 1,98 (LC à 95 % 1,15-3,4) pour ceux présentant des difformités visibles au départ (grade 2 de l'OMS). Parmi les patients avec des incapacités au moment du diagnostic, 195/396 (49,2 %) étaient améliorés après 2 ans. Conclusions: La proportion de patients avec des incapacités après deux ans de traitement antilèpre était 12 % inférieure à celle au moment du diagnostic. Parmi les patients sans incapacité initiale, 10 % avaient développé une incapacité après 2 ans. Le risque de développer des incapacités était presque double pour ceux présentant des altérations de la sensibilité ou des difformités visibles au diagnostic. Pour le monitoring, l'évaluation et la planification, la proportion de patients avec des altérations de la sensibilité (grade 1 de l'OMS) et la proportion de patients présentants des altérations visibles devraient toutes deux être rapportées au montem du diagnostie et à la lin du traitentent.RESUMEN
Objetivo: investigar en los pacientes con lepra rnultibacilar (MB), el progreso de discapacidad en función del tiempo de la enfermedad. Diseño: Se trata de un estudio retrospectivo de cohortes. Población de estudio: Un mil ochenta y dos pacientes MB nuevos registrados en nueve clínicas rurales de la región occidental de Nepal, entre 1980 y 1993. Métodos: Se revisaron los expedientes de pacientes MB que habían sido dados de alta después de terminar su tratamiento con poliquimioterapia (PQT) y se recopilaron los datos sobre discapacidad en el momento del diagnóstico y a intervalos anuales después del tratamiento. Como medida de discapacidad, se utilizó la escala de la Organización Mundial de la Salud propuesta en 1988 (0-2, para ambos ojos, manos y pies- seis sitios). Para el análisis sumamos los puntos para los seis sitios en una calificación global para ojos-manospies (OMP) (mínimo 0, máximo 12). La calificación OMP a los dos años de seguimiento se usó para calcular las principales consecuencias resultantes: discapacidad a los 2 años, sí o no, y deterioro de la discapacidad en comparación con la discapacidad al momento del diagnóstico. Usando un procedimiento de regresión logística, se examinó el efecto combinado de la edad, sexo, clasificación y estado de la discapacidad al momento del diagnóstico, sobre el resultado encontrado. Resultados: En el momento del diagnóstico, el 55% de los pacientes tuvieron alguna discapacidad. Este porcentaje disminuyó en dos años al 43.9%. Entre los pacientes sin discapacidad inicial, 31/310 (10%) desarrollaron alguna discapacidad durante el tiempo del estudio. El porcentaje fue de 81/396 (20.5%) entre los pacientes con discapacidad en el tiempo del diagnóstico. La tasa de probabilidad ajustada para discapacidad en desarrollo fue de 1.87% [95% de intervalo de confianza (IC) 1.06-3.32] para pacientes con discapacidad sensorial inicial (Grado 1 de la OMS) y de 1.98 (95% CI 1.15-3.4) para aquellos con una deformidad inicial visible (OMS grado 2). Entre los pacientes con discapacidad al momento del dignóstico, 195/396 (49.2%) mejoraron en los 2 años siguientes. Conclusiones: La proporción de pacientes con discapacidad después de 2 años de tratamiento antileproso fue 12% menor que al momento del diagnóstico. Entre los pacientes sin diseapacidad inicial, 10% desarrollaron algún tipo de discapacidad después de 2 años. El riesgo de dearrollar discapacidad fue casi del doble para aquellos con discapacidad sensorial o deformidad visible al momento del diagnóstico. Para propósitos de seguimiento, de evaluación y planificación, se recomienda que tanto la proporción de pacientes con discapacidad sensorial (grado 1, OMS) como la proporción de pacientes con deformidad visible (grado 2, OMS), deberían ser reportadas en el momento del diagnóstico y cuando los pacientes son liberados del tratamiento.Deformity and disability-the inability to perform activities of daily living-are major outcome "measures" of interest for leprosy patients. It has, therefore, been suggested that "disability" indicators should be used to monitor and evaluate progress in leprosy control (11, 17, 18). This paper uses the terms "impairment" and "disability" as defined in the World Health Organization's (WHO) publication International Classification of Impairments, Disabilities and Handicaps (ICIDH) (25). We will, therefore, refer to the "WHO disability grade" as the "WHO impairment grade."
It is only when disabilities are understood from a functional point of view, which is relevant to the patient, and in their relationship to impairments that more appropriate disability prevention programs can be initiated. A study is being carried out in our Leprosy Control Project (LCP) in West Nepal to find any associations between impairments and disabilities in leprosy patients. To get some baseline information, a retrospective study was undertaken of WHO impairment grades of a large number of field patients. In particular, the progress of those impairment grades over time after the patients had started chemotherapy was reviewed.
Study questions. 1. In what ways do WHO impairment grades of leprosy patients progress over time following commencement of chemotherapy? 2. How does that differ for patients without impairment at the commencement of treatment compared with those already impaired? 3. Does age, sex and type of leprosy affect the progress mentioned in 1?
SUBJECTS AND METHODS
A record review was done of all multibacillary (MB) patients registered between 1980 and 1993 and already released from treatment (RFT) at nine mobile clinic treatment centers in the Western Region. Case finding has been based on voluntary reporting. The diagnosis "leprosy" was made by experienced paramedical field staff. The MB/PB classification was based only on clinical criteria and skin smears as described previously (20). The ballpoint pen method was used to test sensibility at 10 sites on the palm of the hand and 10 on the sole of the foot. From each patient card, the following information was collected: registration and RFT dates, age, sex, leprosy type, WHO impairment grades at diagnosis and any other recording at yearly intervals. The WHO grading used in these clinics was either the 4-point scale introduced in 1970 (23) or the 3-point scale introduced in 1988 (24). When the former grading was used, it was recoded to the 1988 format by grouping the grades "2" and "3 " together as "2" (= visible deformity). In the case of impairment, the former grade 3 (severe visual impairment) became the new grade 2.
Statistical methods. To assess the progress of the impairment status of our study patients over time, an impairment sum score was employed. We used essentially the same score as de Rijk, et al. (4), but included eye impairment as well. The sum score is thus the sum of the WHO impairment grades of both eyes, hands and feet (EHF score: minimum 0 = no impairment; maximum 12 = visible deformity of both hands and feet, and severe bilateral impairment. The EHF score was calculated at diagnosis and for annual follow-up examinations which the patient had attended. To assess whether the patient had improved, stayed the same, or deteriorated, the difference in EHF scores between diagnosis and annual follow ups was calculated. A positive difference score was called "improvement," a score of zero was "stable," and a negative score was "deterioration."
We decided to use the data after 2 years as the main outcome measure because the proportion of patients lost to follow up increased dramatically beyond this. At 2 years, a sample of 706 remained (64.3%). The association between a three-category (deteriorated, stable, improved) outcome at 2 years and the explanatory variables was examined using 3 x N tables. Logistic regression was used to look at the joint effect of the explanatory variables on the outcome (3). For this purpose, the outcome was divided into only two categories, "deteriorated" and "stable or improved." The odds ratios (OR) obtained show the increase in risk of becoming more impaired when a patient belongs to a certain category, compared with those in the baseline category. The 95% confidence intervals (95% CI) for the OR are given. If these do not include 1, then the association is significant at the 5% level.
RESULTS
The mean age of the study subjects at diagnosis was 38.7 years. Seven-hundred-forty-one patients were males (68.5%). Table 1 shows the distribution of the study patients into two groups, according to whether they had a 2-year follow-up record or not. The two groups were not significantly different, except for a larger proportion of females among those who did not have a follow up. Even after 1 year, the median impairment status (EHF score) of both groups was not significantly different. Of the 1082 patients, 478 (44.2%) had no impairment (a score of 0) at diagnosis. This left 55.8% of the patients scoring 1 or more.
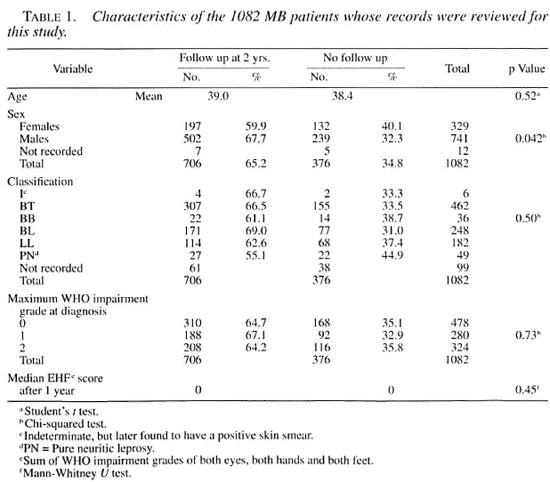
Seven-hundred-six patients had an impairment grade recorded at the 2-year follow-up examination. Among these patients, 310 (43.9%) had no impairment at diagnosis. Two years after the start of leprosy treatment, the number without impairment had increased to 396/706 (56.1%). Therefore, it appeared that about 12% of the patients had improved during this period. However, although this was the net result, the real situation was more complicated. Of 310/706 patients without initial impairment, 31 (10%) had developed some impairment after 2 years (Fig. 1). Of the 396 who had impairment at diagnosis, 195 (49.2%) improved, 120 (30.3%) remained stable, and 81 (20.5%) deteriorated (Fig. 2).
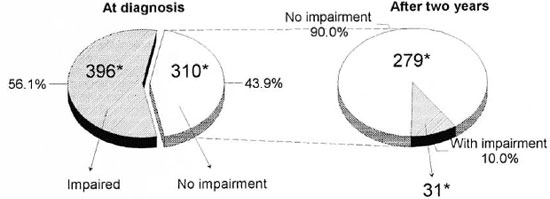
Fig. 1. Changes in impairment status during a 2-year period in MB patients without initial impairment (N = 310) in the Western Region of Nepal. * = number or patients in each category.
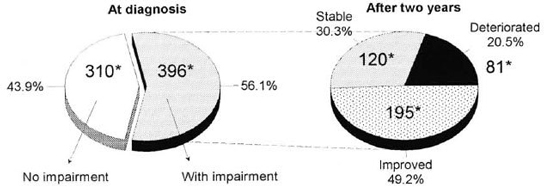
Fig. 2. Changes in impairment status during a 2-year period in MB patients with impairment at diagnosis (N = 396) in the Western Region of Nepal. * = number of patients in each category.
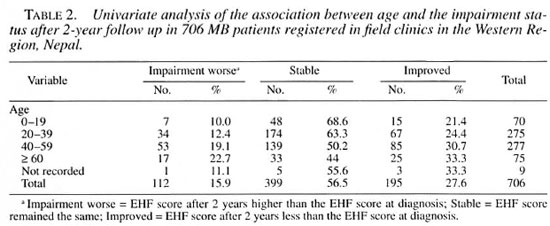
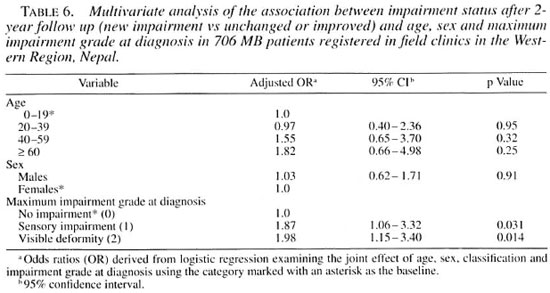
Impairment after 2 years and age. Table 2 shows that both the proportions of patients who deteriorated and who improved increased with age. This trend was (with our study size) not statistically significant for "deterioration" when the joint effects of age, sex, classification and initial impairment status were examined (Table 6). For "improvement," the trend completely changed in the multivariate model, with older age groups being less likely to improve than those in the under-20 group (data not shown).
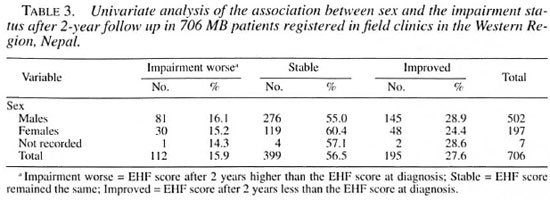
Impairment after 2 years and sex. Table 3 shows that there was little difference between males and females in the progress of impairment after 2 years.
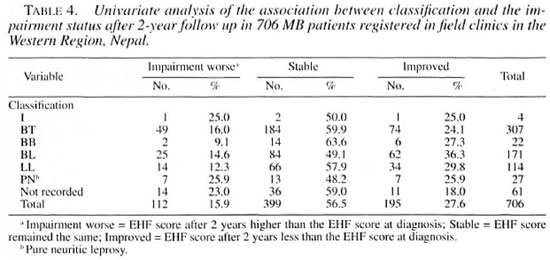
Impairment after 2 years and classification. There were no significant differences in improvement or deterioration among the three patient groups (BT, BL, LL) which had sufficient numbers to make comparisons (Table 4).
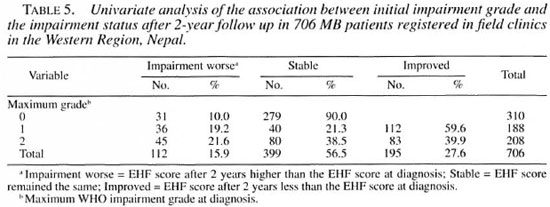
Impairment after 2 years and initial impairment grade. Table 5 shows that the risk of developing new impairment was double for those who already had some impairment at diagnosis (grades l and 2 combined) compared with those who had no impairment (20.5% vs 10%, OR 2.05, 95% CI 1.4-3.0, p = 0.0002). An important observation was that the increased risk was about equal for those who only had sensory impairment at diagnosis and for those who already had some visible deformity (adjusted OR 1.87 and 1.98, respectively; Table 6).
DISCUSSION
Few investigators have reported on the incidence of impairment (9, 12, 14) or changes in impairment status over time (13, 16). In the current study we examined the changes in impairment status that occurred during 2 years of MDT (a few patients were initially treated with dapsone) in a cohort of MB patients. The study was retrospective and was not free from the weaknesses inherent to such a design. Because all MB cases RFT during the afore-mentioned years were included, the results should at least be representative for MB patients at the given clinics. The main problem concerns loss to follow up. At 2 years, 35.7% of the patients had been lost as far as recording of impairment status was concerned. However, a detailed comparison of those with and those without a recording at 2 years revealed no differences between the two groups, except that fewer women had a follow-up examination (Table 1). This difference was, although significant at the 5% level, not large (40 .1% of women vs 32.3% of men not having a follow-up exam). It is unlikely that the higher dropout rate among women was directly associated with their impairment status; rather, it reflects the greater difficulty experienced by women in Nepal to attend the health services, particularly for prolonged periods. We concluded that, despite the loss to follow up, the remaining sample could still be considered representative of the whole study group.
Prevalence. Among our study patients 56% had some impairment at diagnosis. During a recent survey among newly detected cases in East Nepal, this proportion was 64 .1% (15) . In Ethiopia, the proportion of new MB patients with impairment was very similar-56.4% (4). In a cohort of MB patients in Malawi, only 34.1% had "disability at diagnosis" (l 3) . The lower prevalence in Malawi seems to be at least partly due to a much lower reported prevalence of grade 1 (sensory impairment); 12.1%, compared with 26.9% in East Nepal, 32.3% in Ethiopia and 25.9% in the current study.
Incidence and risk factors. Smith, et al . (17) state that the realistic component of "disability" in their patient study population reversible by surgery and health education would be 8.3%. In contrast to this, our results show that 49.2% of our patients who were impaired at diagnosis actually improved (Fig. 2). Possible explanations for this observation are the effect of corticosteroid treatment, spontaneous recovery, the effect of surgery and ulcer care during hospital referral and, finally, the possibility of error. It is noted that this study was retrospective and that the data collection was, therefore, less controlled than in a prospective study. Prospective studies on the incidence and evolution of impairment during and after MDT are overdue.
The cumulative incidence of new impairment among patients without impairment at diagnosis was 10% over a 2-year period in the current study. For patients with initial impairment this figure was 20.5%. Data for comparison are few. Smith reported a 16.5% incidence of new nerve damage "during MDT" (16). We found a cumulative incidence of motor and/or sensory nerve impairment of 23.3% among 335 hospital outpatients over an average follow-up period of 21 months (21). More than half of these patients improved after steroid treatment, so the proportion of patients left with new impairments at the end of 2 years was comparable to the above figure of 10%. Among 118 patients with impairment followed over a 4-year period in India, 16.1% improved and 23.7% deteriorated (16). Ponnighaus and Boerrigter prospectively followed a group of MB patients, randomized into taking either one of two fixed-duration MDT regimens, for an average of about 3 years (13). In the initially impairment-free group, 28/201 (13.9%) developed new impairment during the study period, while 52/104 (50%) with a pre-existing impairment deteriorated. This gives a risk ratio among these patients of 3.6 (95% CI 2.42-5.32), suggesting a 3.5-times increased risk of developing impairment among those already impaired at diagnosis. Among our study patients, the presence or absence of impairment at diagnosis also proved to be the major risk factor for developing new impairment. When the effects of age, sex, classification and impairment grade at diagnosis were examined in a joint model, only the effect of the latter remained as an independent risk factor (Table 6; OR 1.98, 95% CI 1.15-3.4).
It is important to note that the neartwofold increase in risk was almost equal in patients who "only" had sensory impairment at diagnosis to those who already had visible deformity. This emphasizes the importance of detecting sensory impairment and taking appropriate measures to prevent secondary tissue damage. It also highlights the importance of reporting patients with sensory impairment in routine statistics used for monitoring, evaluation and planning. The only impairment-related indicator commonly used in routine statistics is the "proportion of patients with WHO grade 2 among new cases." While this may be a useful indicator of delay in case finding, it completely overlooks a very substantial group of patients at risk. We would strongly recommend that influential bodies such as WHO and ILEP would require reporting of the proportion of patients with grade 1 and the proportion with grade 2 at diagnosis and at RFT.
Radhakrishna and Nair reported data that yielded an incidence rate of deformity of approximately 71.5/1000 patients per year among borderline, indeterminate and lepromatous patients (14). This would give a cumulative incidence of 14% over 2 years. These data did not include sensory impairment as "deformity." However, the overall incidence is in the same order of magnitude as in the above-mentioned studies. Using a stratified analysis, Radhakrishna and Nair showed an association between the incidence of deformity and age, sex, type of leprosy and treatment (dapsone) regularity. Patients who were more regular in attending for treatment were more likely to develop deformity. Several other authors have also reported this apparent association (6, 19). Others have pointed out that this association may be due to confounding (5, 8). Patients with (more severe) impairment or who develop impairment are likely to be more motivated to attend for treatment than those with minor or no impairment.
A much lower incidence of only 0.6% "disability" was reported by Keeler and Ryan among 335 patients without impairment at diagnosis during a 2- to 6-year follow-up period. The reason for this low incidence is not clear. Ponnighaus, et al. report an equally low incidence rate of "disabilities" of 2.9/1000 person years at risk during MDT among 1229 patients in Malawi. However, most of these patients were PB (tuberculoid), who have a much lower incidence of impairment (14). The incidence of impairment among MB patients from the same area, described by Ponnighaus and Boerrigter, was comparable to ours (see above).
Conclusions. 1. In a cohort of 1082 MB patients in the Western Region of Nepal, the majority had some impairment at diagnosis (55.8%). 2. After 2 years, the proportion impaired had decreased to 43.9%, a net improvement of 12%. 3. Among patients without impairment at diagnosis, 10% had developed some after 2 years. The risk of developing impairment was almost double for those with sensory impairment and those with visible deformity at diagnosis. 4. For purposes of monitoring, evaluation and planning, both the proportion of patients with sensory impairment (WHO grade 1) and the proportion with visible deformity (WHO grade 2) should be reported at diagnosis and at RFT
Acknowledgment. We are grateful to the staff of the INF mobile clinic in the Western Region of Nepal who enabled us to do this study and to I IMG/Nepal for their cooperation in the field work. Dr. Alison M. Anderson gave constructive comments during the drafting of this paper. The work of the INF Leprosy Project is dedicated to God.
REFERENCES
1. BECHELU, L. M. and DOMINGUEZ, V. M . Disability INDEX lor leprosy patients. Bull. WHO 44(1971)709-713.
2. BRANDSMA, J. W., HEERKENS, Y. F., LAKERVELD-HEYL, K. and MISCHNER-VAN RAVENSBERG, C. D. The international classification of impairments, disabilities and handicaps in leprosy control projects. Lepr. Rev. 63(1992)3.37-344.
3. CLAYTON, D. and HILLS, M. Statistical Models in Epidemiology. Oxford: Oxford University Press, 1993.
4. DE RUK, A. J., GABRE, S., BYASS, P. and BERHANU, T. Field evaluation of WHO-MDT of fixed duration, at ALERT, Ethiopia: the AMFES project-I. MDT course completion, case holding and another score for disability grading. Lepr. Rev. 65(1994)305-319.
5. GIRDHAR, K., ARORA, S. K., HOHAN, L. and MURIUM, R. D. Pattern of leprosy disabilities in Gorakhpur (Uttar Pradesh). Indian J. Lepr. 61(1989)503-513.
6. GUPTE, M. D. Dapsone treatment and deformities: a retrospective study. Lepr. India 51(1979)218-233.
7. HASAN, S. A survey of leprosy deformities among the patients of Hyderabad city. Lepr. India 49(1977)393-399.
8. KAUR, P. and SINGH, G . Deformities in leprosy patients attending urban leprosy clinic at Varanasi. Indian J. Lepr. 57(1985)178-182.
9. KELLER, R. F. and RYAN, M . A. The incidence of disabilities in Hansen's disease after the commencement of chemotherapy. Lepr. Rev. 51(1980)149-154.
10. KUSHWAH, S. S., GOVILA. A. K. and KUSHWAH, J. An epidemiological study of disabilities among leprosy patients attending leprosy clinic in Gwalior. Lepr. India 53( 1981 )240-247.
11. MISHRA, B., RAMU, G., CHAUHAN, V. S., KUSHWAH, S. S. and DWIVEDI, M. P. Leprosy deformities. II. As parameters to monitor the effectivity of leprosy control programme. Indian J. Lepr. 60(1988)260-266.
12. PONNIGHAUS, I. M., BOERRIGTER, G., FINE, P. E. M., PONNIGHAUS, J. M. and RUSSELL, J. Disabilities in leprosy patients ascertained in a total population survey in Karonga district, northern Malawi. Lepr. Rev. 61(1990)366-374.
13. PONNIGHAUS. J. M. and BOERRIGTER, G. Are 18 doses of WHO/MDT sufficient for multibacillary leprosy; results of a trial in Malawi. Int. J. Lepr. 63(1995)1-7.
14. RADHAKRISHNA, S. and NAIR, G. K. Association between regularity in dapsone (DDS) treatment and development of deformity. Int. J. Lepr. 55(1987)425-434.
15. SCHIPPER, A., LUBBERS, W. J., HOGLWEG, M. and DE SOLDENHOFF, R. Disabilities of hands, feet and eyes in newly diagnosed leprosy patients in eastern Nepal. Lepr. Rev. 65(1994)239-247.
16. SMITH, W. C. S. The epidemiology of disability in leprosy including risk factors. Lepr. Rev. 63 Suppl.(1992)23s-30s.
17. SMITH, W. C. S. and PARKHE, S. M. Disability assessment as a measure of progress in leprosy control. Lepr. Rev. 57(1986)251-259.
18. SMITH, W. C. S., ANTIN, U. S. and PATOLE, A. R. Disability in leprosy: a relevant measurement of progress in leprosy. Lepr. Rev. 51(1980)155-166.
19. SRINIVASAN, H. and NOORDEEN, S. K. Epidemiology of disability in leprosy. 2. Factors associated with low disability. Int. J. Lepr. 34(1965)170-174.
20. VAN BRAKEL, W. H., DE SOLDENHOEE, R. and MCDOUGALL, A. C. The allocation of leprosy patients into paucibacillary and multibacillary groups for multidrug therapy, taking into account the number of body areas affected by skin, or skin and nerve lesions. Lepr. Rev. 63(1992)231-245.
21. VAN BRAKEL, W. H. and KHAWAS, I. B . Nerve damage in leprosy: an epidemiological study of 396 patients in West Nepal-part 1: definitions, methods and frequencies. Lepr. Rev. 65(1994)204-221.
22. VAN GIJN, J. Measurement of outcome in stroke prevention trials. Cerebrovasc. Dis. 2 Suppl. 1(1992)23-34.
23. WHO EXPERT COMMITTEE ON LEPROSY. Fourth report. Geneva: World Health Organization, 1970. WHO Tech. Rep. Ser. 459.
24. WHO EXPERT COMMITTEE ON LEPROSY. Sixth report. Geneva: World Health Organization, 1988. WHO Tech. Rep. Ser. 768.
25. WORLD HEALTH ORGANIZATION. International classification of impairments, disabilities and handicaps. Geneva: World Health Organization, 1980.
1. B. Appl. Sc. (Physiotherapy), Physiotherapist, Green Pastures Hospital, Pokhara, Nepal.
2. Ph.D., Project Director, INF Leprosy Project, P. O. Box 5, Pokhara, Nepal.
3. B.Appl.Sc. (Physiotherapy), Physiotherapist, Western Regional Hospital, Pokhara, Nepal.
Reprint requests to Dr. van Brakel at the above address or FAX 977-61-20430.
Received for publication on 27 February 1996.
Accepted for publication in revised form on 16 April 1997.