- Volume 65 , Number 4
- Page: 443–9
Histopathologic evidence to show that indeterminate leprosy may be a primary lesion of the disease
ABSTRACT
Five biopsies of patients with indeterminate leprosy and five with skin lesions of nonspecific chronic inflammation were chosen. Histopathologic changes in the presence of acid-fast bacilli (AFB) in an average number of 145 serial sections f rom the entire paraffin block f rom each were evaluated. In all five indeterminate lesions AFB were found in the dermis, but intraneural AFB were present in only two cases. Mainly, lymphocytic infiltrate was present in two and early, poorly formed granulomas were seen in three. It is suggested that nonspecific chronic inflammation of the skin could precede indeterminate disease and that AFB, before they entered the dermal nerves, may be found in other dermal tissues. In most if not all early lesions of indeterminate leprosy Mycobacterium leprae would be found if an adequate number of sections stained for AFB were examined. The histopathologic and immunologic features of indeterminate disease were in favor of it being a primary lesion in leprosy.RÉSUMÉ
Cinq biopsies de patients avec une lèpre indéterminée et cinq avec des lésions cutanées d'inflammation chronique non spécifique ont été choisies. Pour chacune, on a évalué les modifications histopathologiques en présence de bacilles aeido-résistants (BAR) dans un nombre moyen de 145 coupes en série faites à partir du bloc entier de paraffine. On a trouvé des BAR dans le derme de toutes les cinq lésions indéterminées, mais des BAR intraneuraux n'étaient présents que dans deux cas. Pour l'essentiel, un infiltrat lymphocytaire était présent dans deux cas, et des granulomes débutants et faiblement formés ont été vus dans trois cas. On suggère que l'inflammation chronique non spécifique de la peau pourrait précéder le stade indéterminé et que les BAR, avant qu'ils ne pénètrent dans les nerfs dermiques, pourraient être trouvés dans d'autres tissue du demie. Du Mycobacterium leprae serait trouvé dans la plupart, si pas dans toutes les lésions débutantes de lèpre indéterminée, si un nombre adéquat de coupes était coloré pour la receherche de BAR. Les caractéristiques histopathologiques et immunologiques de la maladie indéterminée étaient en faveur du fait qu'il s'agissait d'une lésion primaire de la lèpre.RESUMEN
Se escogieron 5 biopsias de lesiones de pacientes con lepra indeterminada y cinco biopsias de lesiones de inflamación crónica inespecilica. Se evaluaron los cambios histopatológicos y la presencia de bacilos ácido resistentes (BAAR) en un promedio de 145 secciones seriadas de cada una de las biopsias. En las 5 biopsias de las lesiones de lepra indeterminada se encontraron BAAR en la dermis, pero sólo se observaron BAAR intraneurales en dos de las biopsias. En dos casos se observaron infiltrados de linfocitos y pequeños granulomas incipientes en los tres restantes. Se sugiere que la inflamación crónica no específica de la piel puede preceder a la enfermedad indeterminada y que los BAAR pueden encontrarse en otros tejidos dérmicos antes de penetrar a los nervious de la piel. También se concluye que el Mycobacterium leprae puede encontrarse en la mayoría o en la totalidad de las lesiones dérmicas si se examina un número suficiente de cortes histológicos teñidos para BAAR. Las características histopatológicas e inmunológicas de la lepra inde te minada corresponden a las características de las lesiones primarias de la lepra.Indeterminate leprosy is widely accepted as the earliest manifestation of the disease (7,8,12,14). Clinically it presents as a single, hypopigmented or erythematous macule with minimal or no impairment of sensations. Very rarely more than one lesion is present. Histopathologically, a mild lympho-histiocytic infiltrate is present around skin adnexa. Superficial and deep dermal nerves are selectively involved, showing endoneural and perineurial inflammation. There may also be focal areas of epidermal erosion and spongiosis (1,4,8,9,16,17). Acidfast bacilli (AFB) are not always detected.
Even after several investigative studies, indeterminate leprosy has remained an enigma. The possibility of having minimal nonspecific changes in the skin (16) and the finding of AFB in sites other than nerves, such as the mononuclear phagocyte system, preceding the formation of nerve lesions (6) have been put forward. It has been said that if a sufficient number of sections stained for Mycobacterium leprae are carefully examined using an oil immersion lens, AFB will be found in most if not all cases of indeterminate leprosy (16). Opinion is also expressed that indeterminate lesions may gradually or abruptly evolve into cither tuberculoid or lepromatous leprosy (15).
This study was undertaken to evaluate the above pronouncements and to find out whether the histopathological changes in an indeterminate lesion justify considering it a primary lesion of leprosy.
MATERIALS AND METHODS
St. Thomas Hospital and Leprosy Centre, Chettupattu, India, has a dermatology outpatient department to which patients suspected to have leprosy report for diagnosis and management. Skin biopsies are done whenever the clinical diagnosis of leprosy is in doubt. Diagnostic skin biopsies are, in most cases, 1.0-cm long and 0.5-cm wide and always include the subcutaneous tissue. Of these patients, five histopathologically diagnosed as indeterminate leprosy and five as nonspecific chronic inflammation (NCI) of the skin were chosen for study. Mild adnexal and selective perineural and intraneural inflammation of nerves were found in all five cases of indeterminate leprosy. There was no granuloma and AFB were absent in the five sections stained for AFB from each case. The clinical picture, such as the age and sex of the patient, site, duration and morphology of the lesions and involvement of cutaneous nerves and nerve trunks, was recorded.
The paraffin blocks of all 10 specimens were retrieved; serial sections were prepared from the entire block; all sections were carefully numbered, mounted, and stained with a modified Fite method for AFB (5) in which the cellular details of the lesion and the presence of AFB could be evaluated simultaneously. The number of sections from each biopsy varied from 41 to 233, with an average of 145. All sections were evaluated first for histopathological changes noting epidermal lesions and changes in skin adnexa, particularly the dermal nerves, and for the presence of granuloma. The sections then were searched for AFB under an oil immersion lens, in the epidermis, subepidermal connective tissues, nerves, endothelial cells, arrector pili muscles, sweat glands and macrophages, until bacilli were detected in at least three of the serial sections.
RESULTS
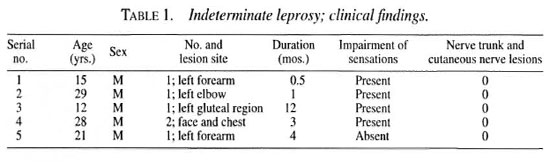
Clinical picture. Of the five patients diagnosed as indeterminate leprosy, all were males between the ages of 15 and 29 years, with an average of 21 years (Table 1). All five of them had hypopigmented macular lesions with vague borders. Some impairment of sensations was present in all but one. The duration of the patch ranged for 2 weeks to 12 months, with an average of 4.1 months. A single patch was present in four cases and of these three were in the upper extremities and the fourth was in the gluteal region. The fifth patient had two lesions, one each on the face and chest. Nerve trunks and cutaneous nerves did not show any thickening or tenderness in any of them, and there were no other lesions.
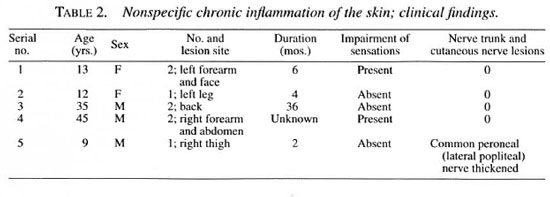
Of the 5 patients diagnosed to have NCI of the skin, 2 were females and 3 males between the ages of 9 and 45 years, with an average of 22.8 years (Table 2). All five had hypopigmented macules with vague borders. Minimal impairment of sensations was present in two. The duration of the patch in four patients varied from 2 months to 36 months and in one the duration was unknown. There were two patches in three of them and the other two had only one lesion. In the two patients with single lesions, the patches were found in the lower extremities and in one of them the right common peroneal (lateral popliteal) nerve showed mild thickening but there was no pain or tenderness. In the three patients with two lesions, one had lesions on the forearm and face, the second had them on the forearm and abdomen, and the third patient had both lesions on the back. No other lesions were detected.
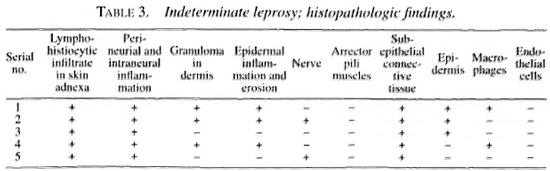
Histopathologic examination. An examination of all serial sections, averaging 145 in number, from the entire paraffin block from the five indeterminate lesions confirmed the presence of lympho-histiocytic infiltrate occupying <10% of the dermis, and selective perineurial and intraneural inflammation of the dermal nerves (Fig. 1 ). Early granuloma formation with a small number of epithelioid cells surrounded by collections of lymphocytes was detected in three patients. In two of them there were discrete microgranulomas with a poorly formed Langhans' giant cell in each (Fig. 2). In all three at least 13 serial sections were examined before granulomas were detected. Two microgranulomas each were found in two cases, and four in the third one. Two of the microgranulomas occupied three consecutive sections of 5µm thickness; the largest one occupied 11 serial sections. In all of these three cases granulomatous inflammation surrounding dermal nerves and destroying the entire perineurium and part of the endoneurium was present (Fig. 3). Epidermal infiltration by lymphocytes and erosion of the epithelium was also found in these three patients (Fig. 4). No granuloma was seen in the other two cases.

Fig. 1 Indeterminate leprosy; skin showing lymphohistiocytic infiltrate occupying <10% of the dermis. A longitudinal section of nerve bundle (←) showing intraneural and perineurial inflammation by lymphocytes lhematoxylin and eosin (1I&E) x50l.

Fig. 2. "Indeterminate" lesion becoming "deter-mined"; granulomatous inflammation in the superficialdermis composed of collections of epithelioid cells and lymphocytes. A poorly formed giant cell is seen in the granuloma (H&E x480).
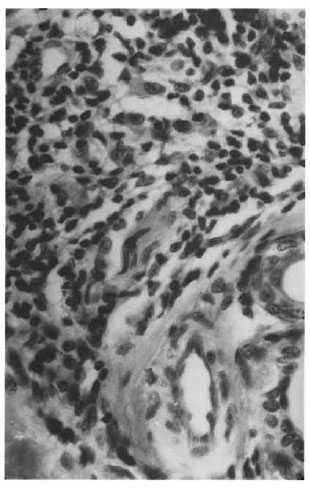
Fig. 3. "Indeterminate- lesion becoming "deter-miner; granulomatous inflammation of a dermal nerve showing complete destruction of the perineurium. Aportion of the nerve parenchyma is identified in the granuloma (H&E x480).
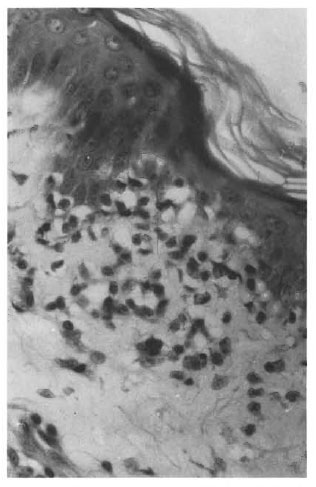
Fig. 4. Indeterminate leprosy; skin with epidermisshowing erosion and infiltration with lymphocytes (H&E x480).
AFB were present in subepidermal connective tissue in all 5 cases (Fig. 5), intraneurally in 2, inside macrophages in 2 (Fig. 6), in the basal layer of the epidermis in 3, and in the granular layer in 1. The arrector pili muscles, sweat glands and endothelial cells did not show any bacilli. The first evidence of AFB was found in all five patients by the time the 15th serial section was examined, and AFB were found a third time by the time the 67th section was studied.
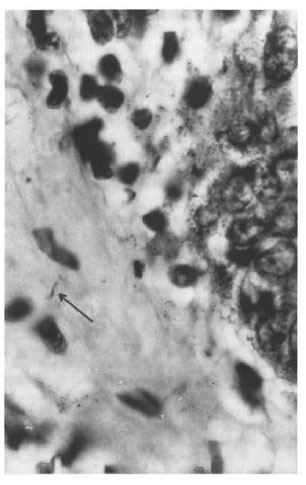
Fig. 5. Indeterminate leprosy; AFB (←) in the subepithelial connective tissue (H&E x1200).
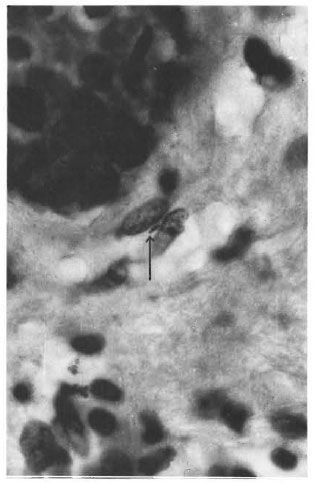
Fig. 6. Indeterminate leprosy; AFB (←) inside amacrophage in the dermis (H&E x 1200).
In the five cases diagnosed as NCI, the epidermis showed minimal hyperkeratosis in one, and no significant change in any of the others. In the dermis there was mainly perivascular inflammation mostly confined to the superficial and midportion. Neurovascular-bundle inflammation was present in the superficial dermis in one case and in another, a nerve bundle in the mid-dermis showed Schwann cell hyperplasia. The inflammatory cells were composed of lymphocytes and histiocytes. There was only minimal involvement of other skin adnexa. No intraneural or perineurial inflammation and no AFB were detected in any of them.
DISCUSSION
All 10 of the patients included in the study had a similar clinical picture, having one or two hypopigmented macules mostly on the extremities with minimal or no impairment of sensations. In the five cases with NCI of the skin, the serial sections examined showed mild infiltration with lymphocytes mainly around the dermal blood vessels. Skin adnexal involvement was minimal and was not significant. Even after examining an average of 145 serial section no selective intraneural or perineuria! inflammation, no granulomas and no AFB were found. The inflammation of the neurovascular bundle in the superficial dermis present in one case is not uncommon in cases of superficial dermatitides. The assessment of Schwann cell hyperplasia found in another could be subjective and might be "due to repair of Wallerian degeneration following minor trauma or other causes" (16). However, the possibility of NCI preceding lesions of indeterminate leprosy should not be ruled out.
M. leprae were found in the granular layer of the epidermis in 1 patient, in the basal layer in 3, and in the subepithelial connective tissue in all 5 patients diagnosed as indeterminate leprosy. The macrophages in the superficial dermis also had M. leprae in two cases. In two patients there were AFB in dermal nerves. Further, dermal nerves also showed destruction of the entire perineurium with much of the endoneurium preserved. In a case of early leprosy with a single skin lesion, proliferation of a perineuria! cell with AFB in one of them and no significant endoneural changes has been reported (10). Considering all of this evidence, M. leprae entering the site through the epidermis involving much of the dermal structures, including dermal nerves, causing a localized primary lesion in the skin is a distinct possibility (15).
On examination of the serial sections from the five indeterminate patients, AFB were found in all before the 15th serial section was examined. Therefore, this study confirms Ridley's contention that in all biopsies of patients with early leprosy, AFB could be detected if fairly large numbers of serial sections stained properly for M. leprae were carefully examined under an oil immersion lens and searched for in the appropriate sites (16).
In 2 of the 5 cases of indeterminate leprosy, after examining all the serial sections from the block, no granulomas were detected in either of them. AFB in large numbers inside macrophages or other sites were not seen. Their immune system at that point in time had been neither sensitized to produce a tuberculoid granuloma nor made tolerant to have a lepromatous response. It should be noted that the evolution into either tuberculoid or lepromatous disease will also depend on HLA-linked genetic factors (3,18). These two patients were in a phase in which the lesion was "not determined." Is it possible to have an indeterminate lesion at a metastatic site or during re-infection? If M. leprae had entered the body in these patients through the nasal mucosa (2) or by some other route, a primary focus would have been established at that site and any metastatic lesion should be a "determined lesion."
In this study of indeterminate disease two phases were seen. An early phase in which there was only a minimal lymphocyte response demonstrating insufficient immunity and a subsequent phase in which there was adequate immunity to produce a poorly formed epithelioid cell granuloma. In an immunologic study of 14 indeterminate patients, two phases were recognized in their responses to the lymphocyte transformation tests: an initial insignificant or negative response, followed at a later date by a positive lymphocyte response (11). It appears that the immune system, subject to genetic influence, was being primed during indeterminate disease. These two phases of inflammatory reactions and immune responses would not have been seen if there had been another primary site at which the priming of the immune system had already taken place. Therefore, it is reasonable to conclude that the indeterminate skin lesion may be a primary site of the infection in these patients, i.e., the site of initial entry of M. leprae. This does not exclude primary lesions in the nasopharyngeal region or the nose or other sites, depending on other routes of entry of M. leprae.
Acknowledgment. We acknowledge with gratitude the financial support from American Leprosy Missions International, Greenville, South Carolina, U.S.A., which made this study possible. Thanks also go to Mr. K. Rajanna for technical work and to MissK. Jayanthi for secretarial assistance.
REFERENCES
1. BlNFORD, C.H. The histologic recognition of early lesions of leprosy. Int. J. Lepr. 39 (1971) 225-230.
2. CHACKO, C. J. G., MOHAN, M., JESUDASAN, K., JOB, C. K. and FRITSCHI, E. P. Primary leprosy involvement of nasal mucosa in apparently healthy household contacts of leprosy patients. Proceedings XI International Leprosy Congress, Mexico City, 1978. Amsterdam: Excerpta Medica, 1980, p. 264.
3. DE VRIES, R. R. P., MEHRA, N. K., VAIDYA, M. C, GUPTE, M. D., KHAN, P. M. and VAN ROOD, J. J. HLA-linked control of susceptibility to tuberculoid leprosy: confirmation of the DR2 marker. J. Infect. Dis. 141 (1980) 693-701.
4. FINE., P. E. M., JOB, C. K., LUCAS, S. B.; MEYERS, W. M., PONNIGHAUS, J. M. and STERNE, A. C. J. Extent, origin and implications of observer variation in the histopathological diagnosis of suspected leprosy. Int. J. Lepr. 61 (1993) 270-281.
5. JOB, C. K. and CHACKO, C. J. G. A modification of Fite's stain for demonstration of M. leprae in tissue sections. Indian J. Lepr. 58(1986)17-18.
6. JOB, C. K., DRAIN, V., TRUMAN, R. W.; SANCHEZ, R. M. and HASTINGS, R. C. Early infection with M. leprae and antibodies to phenolic glycolipid -I in the nine-banded armadillos. Indian J. Lepr. 62 (1990) 193-201.
7. LIU, T. E., YEN, L. Z., YE, G. Y. and DUNG, G. J. Histology of indeterminate leprosy. Int. J. Lepr. 50 (1982) 172-176.
8. LUCAS, S. and KIRKIIAM, M. Infective and noninfective granulomas. In: Biopsy Pathology of the Skin. Kirkham, N. London: Chapman and Hall Medical, 1991, pp. 304-327.
9. LUCAS, S. and RIDLEY, D. S. The use of histopathology in leprosy diagnosis and research. (Editorial) Lepr. Rev. 60 (1989) 257-262.
10. MURRAY, K. A., MCLKU.AND, B. A. and JOB, C. K. Early perineural proliferation. Arch. Dermatol. 120(1984) 360-361.
11. MYRVANG, B., GODAL, T, F'I.I.K. C. M., RIDLEY, D. S. and SAMUEL, D. R. Immune response to Mycobacterium leprae in indeterminate leprosy patients. Acta Pathol. Microbiol. Scand. [B] 81 (1973)615-620.
12. NAYAR, A., NARAYANAN, J. S. and Jon, C. K. Histopathological study of early skin lesions in leprosy. Arch. Pathol. 94 (1972) 199-204.
13. RIDLEY, D. S. Pathology and bacteriology of early lesions in leprosy. Int. J. Lepr. 39 (1971) 216-224.
14. RIDLEY, D. S. Pathogenesis of the early lesions in leprosy. J. Pathol. 3 (1972) 191-206.
15. RlDLEY.D.S. The early skin lesion of leprosy. In: Pathogenesis of Leprosy and Related Diseases. London: Wright, Butterworth & Co. Ltd., 1988, pp. 61-70.
16. RIDLEY, D. S. Histological diagnosis. In: Pathogenesis of Leprosy and Related Diseases. London: Wright, Butterworth & Co. Ltd., 1988, pp. 146-151.
17. TAKAHASHI, M. D., ANDRADE, H. F., JR., WAKA-MATSU, A., SIQUEIRA, S. and Di: BRITO, T. Indeterminate leprosy: histopathologic and histochemical predictive parameters involved in its possible change to paucibacillary or multibacillary leprosy. Int. J. Lepr. 59 (1991) 12-19.
18. VAN EDEN, W., GONZALES, N. V., DE VRIHS, R. R. P., CONVIT, J. and VAN ROOD, J. J. HLA-linked control of predisposition to Iepromatous leprosy. J. Infect. Dis. 151 (1985)9-14.
1. M.D., F.R.C.Path.; St. Thomas Hospital and Leprosy Centre, Chcttupattu 606 801, T.S. District, Tamil Nadu, India.
2. M.B.B.S., D.C.P.; St. Thomas Hospital and Leprosy Centre, Chcttupattu 606 801, T.S. District, Tamil Nadu, India.
3. M.B.B.S., D.T.M.&H.; St. Thomas Hospital and Leprosy Centre, Chcttupattu 606 801, T.S. District, Tamil Nadu, India.
4. M.D., St. Thomas Hospital and Leprosy Centre, Chcttupattu 606 801, T.S. District, Tamil Nadu, India.
Received for publication on 16 April 1997.
Accepted for publication in revised form on 7 September 1997.