- Volume 65 , Number 4
- Page: 492–4
Alternaria keratomycosis in a lepromatous leprosy patient
In an effort to increase the utility of the JOURNAL in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
To the Editor:
Leprosy affects the eyes in several ways. Corneal ulcers occur in leprosy and together with other corneal pathology account for a substantial amount of ocular morbidity. The ulcers are likely to be more frequent in eyes that have impaired corneal sensation and lagophthalmos. Although most of the corneal ulcers are bacterial, being either due to pneumococcal or staphylococcal infections (personal observations), mycotic corneal ulcers do occur among leprosy patients. These are seen in patients who are agrarian in occupation and are usually related to an injury caused by vegetable matter. Recently we came across a corneal ulcer caused by a ubiquitous mycotic organism in a leprosy patient, and we report its features in this paper.
CASE REPORT
A 45-year-old man had sustained an injury to his left eye with a stick and developed watering, reduced vision and pain in the eye. He took treatment with topical antibiotic drops at a private clinic. Since his ocular condition continued to deteriorate even after 2 months of treatment, he presented at the eye clinic of the Schieffelin Leprosy Research and Training Centre (SLRTC), Karigiri, South India.
He gave a history of having developed a hypopigmented anesthetic patch on his left elbow 20 years ago. He had taken treatment with dapsone 100 mg daily for 2 years and then discontinued it for 2 years. Subsequently he developed erythematous patches and leg ulcers and took dapsone 100 mg for a year. He discontinued treatment when his leg ulcers healed. Five years later he developed erythematous patches on his face, was found to have anesthesia in all four limbs, was diagnosed as having borderline lepromatous leprosy and took MDT for 2 years. For the past 3 years he had not been on any antileprosy treatment. A skin biopsy taken from the left buttock showed moderatesized granulomas in the dermis composed of vacuolated foamy macrophages and a few scattered lymphocytes. Acid-fast staining showed scattered bacilli singly and in small clumps within the foamy macrophages, nerves and subepidermal zones. The bacilli were granular and beaded. The impression was that of resolving lepromatous leprosy.
An ocular examination showed a normal anterior segment and a visual acuity of 6/9 in the right eye. The corneal sensation in the right eye measured with the Cochet and Bonnet esthesiometer was 1.40 g/mm2. The left eye had a visual acuity of counting fingers at 10 cm. There was lid edema, circumcorneal congestion and purulent discharge. A corneal ulcer measuring about 4 mm was present at the center of the cornea. A small satellite lesion was present at the 9 o'clock position of the cornea, near the limbus (Fig. 1). There was a hypopyon 2 mm in height. Moderate amounts of flare and cells were found in the anterior chamber. The lens was cataractous. Corneal sensation was grossly impaired, being 17.68 g/mm2.
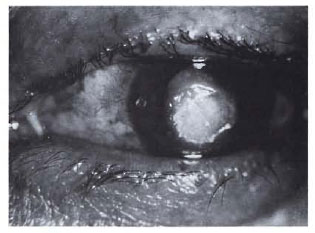
Fig. 1. Mycotic corneal ulcer with a satellite lesionat the 9 o'clock position.
Scrapings obtained from the corneal ulcer were stained using Gram's stain and also examined in a wet mount using 10% potassium hydroxide (KOH). Gram stain did not reveal any bacteria but contained numerous septate fungal hyphae, including bizarre morphological forms (Fig. 2). The KOH preparation also showed fungal elements similar to that seen with Gram's stain. The specimen was plated onto Sabouraud dextrose agar and blood agar and incubated at 28ºC and 37ºC, respectively. A rapidly growing, grayish-black myelial growth appeared on the plates. This dematiaceous fungus was identified to be Alternaría spp. based on its characteristic morphology of multicelled acropetal chains of obclavate to obpyriform conidia with short conical beaks.1,2

Fig. 2. Direct microscopy of corneal scrapingshowing septate fungal hyphae (Gram stain x320).
The mycotic corneal ulcer was treated with topical ketaconazole drops instilled every waking hour alternated with ciprofloxin eye drops. Atropine 1% was also instilled four times a day. The ulcer and the patient's symptoms did not show any improvement although the hypopyon kept disappearing and re-appearing. The treatment was continued and after 3 weeks a faint hypopyon persisted but there was no fluorescein staining of the corneal ulcer. At this point a 1 in 10 dilution of betnesol eye drops was started every waking hour. In a week's time the hypopyon disappeared, the eye was quiet and the betnesol eye drops were stopped and the patient discharged from hospital.
The patient returned with a similar-looking ulcer in the same eye in 3 weeks' time. Corneal scrapings sent for culture did not grow any organism. VDRL and ELISA for HIV were negative. Treatment, as before, was given. The ulcer alternatively healed and broke down several times with the hypopyon appearing and disappearing until after 3 weeks the eye was quiet with a corneal opacity that was vascularized with several blood vessels traveling from the limbus. The patient has had no recurrence of the ulcer in the last 2 years, and the vision in the left eye remained at 6/18.
DISCUSSION
A sizable proportion of leprosy patients become blind or visually incapacitated due to corneal pathology. Although corneal ulcers are not uncommon among leprosy patients, they have not been studied extensively in leprosy. While dealing with corneal ulcers that occur in leprosy patients, etiologies other than a bacterial infection should be kept in mind.
The clinical appearance of the corneal ulcer which developed in this patient suggested a mycotic etiology since there was a history of trauma with vegetable matter, marked congestion, hypopyon and a satellite lesion. The grossly impaired corneal sensation in the affected eye of this patient could be one reason for the frequent breakdown of the ulcer through indiscriminate rubbing of the eyes due to insensitivity.3 This could not be corroborated by questioning the patient.
Infection of the cornea by the fungus Alternaría spp. is quite rare.4 It is an ubiquitous saprophytic fungus whose natural habitat is the soil. Once thought to be an uncommon pathogen, Alternaría spp. are increasingly recognized as pathogenic organisms. It has been known to cause sinonasal infections, cutaneous ulcers, pneumonitis and ocular keratomycosis in humans. The cause of the corneal infection is convincingly established in this case as the fungus Alternaría by demonstrating it by direct microscopy and also by growing it in culture. Alternaría spp. are known to demonstrate fungal elements which may appear globose or show short chains of oblong cells, both of which were seen in this case. We have presented this case report because corneal ulcers infected by Alternaría spp. are rare, and one occurring in a leprosy patient has not been reported. Patients with corneal ulcers that had developed due to vegetable injuries, as is common in patients doing agricultural work, should be suspected of having a fungal etiology and should be treated with broad spectrum antifungal eye drops.
- Ebenezer Daniel, M.B.B.S., M.S., D.O.
Head, Branch of Ophthalmology
Schieffelin Leprosy Research and Training Centre
Karigiri, North Arcot District
Tamil Nadu 632 106, India
- Mary S. Mathews, M.B.B.S., M.D.
Professor
Department of Microbiology
Christian Medical College and Hospital
Vellore, Tamil Nadu 632 004, India
- Shirley Chacko, M.B.B.S., M.D.
Ophthalmologist
Branch of Ophthalmology
Schieffelin Leprosy Research and Training Centre
Karigiri, North Arcot District
Tamil Nadu 632 106, India
1. Morrison, V. A. and Wiesdorf, D. J. Alternaria: an emerging fungal pathogen in normal and immunocompromised hosts. In: Clinic Guide to Fungal Infections. Vol. 5, Issue 3. New York: Lawrence Dellacortc Publications, 1995, pp. 1-6.
2. Schell, W. A., Pasarell, L., Salkin, I. F and McGinnis, M. R. Bipolaris, Exophiala, Scedosporium and other dematiaceous fungi. In: Manual of Clinical Microbiology. 6th edn. Washington, D.C.: American Society for Microbiology, 1995, pp. 825-846.
3. Daniel, E. and Brand, M. An unusual presentation of recurrent corneal abrasion in a lepromatous patient with impaired corneal sensation. Int. J. Lepr. 63 (1995) 450-452.
4. Kwon-Chung, K. J. and Bennett, J. E. Phaeohyphomycosis. In: Medical Mycology. Kwon-Chung, K. J., ed. Philadelphia: Lea & Febiger, 1992, pp. 620-677.