- Volume 64 , Number 1
- Page: 51–7
Rapid village survey to determine the size of the leprosy problem in Khon Kaen province, Thailand
ABSTRACT
The rapid village survey (RVS) method has been developed as a simpler, less-expensive alternative to random sample surveys for determining the prevalence of leprosy and was compared with a total population survey (TVS). In the RVS, the cluster population receives clear information about the disease, and those with symptoms are invited to be examined by the survey team. A list of household contacts and suspects was made and those on the list were actively traced. The registered population was 20,815; 10 new patients were found among the 2034 people self-reporting in the RVS, 0 among the household contacts and suspects, and an additional 2 new patients in the TVS. There were 12 registered patients among the sample population. The prevalence rate found by the RVS was 1.06 per 1000 (95% CI = 0.49-1.63) and in the TVS 1.16 per 1000 (95% CI = 0.5-1.77). The man-days and costs of an RVS are considerably less than those for a TVS. It was concluded that the RVS is a valid replacement for the TVS as conducted in Khon Kaen Province, Thailand. The RVS can be applied under low-endemic conditions and could be carried out by the general hcalth staff.RÉSUMÉ
La méthode d'Enquête Rapide de Village (ERV) a été développée comme une méthode plus simple et moins chère, alternative à l'enquête par échantillonnage aléatoire, pour déterminer la prévalence de la lèpre, et a été comparée à l'enquête de population totale. Dans l'ERV, le groupe de population reçoit une information claire à propos de la maladie, et les personnes qui présentent des symptômes sont invitées à se faire examiner par l'équipe. Une liste des contacts domiciliaires et des suspects a été établie et les personnes notées sur la liste ont été activement recherchées. La population enregistrée était de 20,815 personnes; 10 nouveaux patients ont été découverts parmi les 2034 personnes venues d'elles-mêmes au cours de l'ERV, aucun parmi les contacts domiciliaries et les suspects, et deux nouveaux patients supplémentaires dans l'enquête de population totale. Il y avait 12 patients enregistrés parmi la population de l'échantillon. Le taux de prévalencc obtenu par l'ERV était de 1.06 pour 1000 (L.C. à 95%: 0.5-1.77). Le nombre de personnes-jours et les coûts de l'ERV étaient considérablement moins élevés que ceux d'une enquête de population totale. On en conclut que l'ERV est un bon substitut à l'enquête de population totale telle que conduite dans la Province de Khon Kaen en Thaïlande. L'ERV peut être appliquée dans des conditions de basse cndémicité et pourrait être réalisée par le personnel général de santé.RESUMEN
Se ha desarrollado un método de exploración rápida de pequeñas poblaciones (MERPP) como una alternativa más simple y menos cara de muestreo par a determinar la prcvalcncia de la lepra y su eficiencia se ha comparado con la del método estándar de muestreo de la población total (MPT). En el MERPP, la población estudiada recibe información clara sobre la enfermedad y aquellos con síntomas de la misma son invitados a ser examinados por el equipo de exploración. Los convivientes y aquellos sospechosos de tener la enfermedad son enlistados y mantenidos bajo vigilancia médica. En el estudio, la población registrada fue de 20,815; entre las 2034 personas que se autoreportaron en el MERPP se encontraron 10 casos nuevos, 0 casos entre los convivientes y sospechosos, y 2 nuevos pacientes adicionales en el MPT. Hubieron 12 pacientes registrados entre la población de muestra. La tasa de prevalencia encontrada por el MERPP fue de 1.06 por 1000 (95% Cl=0.49-1.63) en tanto que por el MPT fue de 1.16 por 1000 (95% Cl= 0.5-1.77). Los días-hombre involucrados y el costo del MERPP son considerablemente menores que aquellos del MPT. Se concluyó que, como se llevó a cabo en la provincia de Khon Kacn, Tailandia, el MERPP es un substituto válido del MPT. El MERPP puede ser aplicado en condiciones de baja endemia y puede ser ejecutado por las autoridades generales de salud.Reliable information on the prevalence of leprosy and its trend is of major importance for planning leprosy control activities, among others, in order to evaluate the effectiveness of case finding by the health services. The usual way to secure this information is to conduct a prevalence survey. Traditional prevalence surveys may provide valid information, but are costly and time-consuming (3). Simple and inexpensive methods that can give reasonable estimates of the true leprosy situation and that can be carried out by the general health staff are highly desirable. Several methods have been suggested in the literature, but their degrees of accuracy have not yet been established. Suggested methods for the rapid assessment of the leprosy situation include: rapid village surveys (RVS); extrapolation from registered cases; and school surveys (1,4).
The MURLEP* project (Khon Kaen Province, Thailand, 1989-1994) is a multidisciplinary health systems research project aimed at the development of tools for leprosy and tuberculosis control program managers to estimate prevalence, to monitor performance, and to identify appropriate interventions. The first MURLEP study, carried out in 1990 and 1991, developed and tested the RVS method for the estimation of the extent of the leprosy and tuberculosis problem. The RVS method was then compared to a total population survey, the total village survey (TVS). The present paper reports on the results for leprosy; those for tuberculosis will be reported separately.
METHODS
Definition of RVS. An RVS is a leprosy prevalence survey to determine the size of the leprosy problem in which selected groups of people are examined: those persons selfreporting, contacts of registered leprosy patients, and those persons identified by village leaders as possibly suffering from leprosy. The RVS is different from a total population survey or as called in this study, a total village survey (TVS) in which the whole village (cluster) population is examined by TVS.
Population and sampling. The study area was Khon Kaen Province in the northeastern part of Thailand with a population of about 1.6 million. A list of all villages in Khon Kaen Province was made. The probability of villages to be sampled was proportionate to population size. Urban areas and market villages were excluded because of the composition of those populations (high percentage of immigrants). The estimated prevalence rate was 3 per 1000, and 40 villages (with an average population of 500) were selected and would be surveyed in the first year. Depending on the degree of agreement (or lack of it) between the RVS and TVS, another 40 villages would be examined in the second year. In addition to those 80 villages, another sample of eight villages for pretesting the survey methods was drawn.
Census. A reasonably accurate estimation of the village population is sufficient for an RVS. For a TVS, however, a detailed census is necessary. A village population list obtained from the district office was updated during the RVS with the assistance of the village leaders. During the afternoon of the TVS team's arrival, supervisors went to each household to make up-to-date lists. The sample population included all persons registered during the village census as living in the village for more than 2 weeks and excluded persons who were absent and were not expected to return within 1 month of the TVS.
RVS versus TVS. Each village was surveyed by two methods: first by the newly developed RVS and 1 week later by a TVS. The same team (although extra stall' members were added to the TVS team) conducted both surveys. The population was prepared for the RVS and only at the end of the RVS was the village community informed that the following week a TVS would take place. During the TVS the whole village population was examined for signs and symptoms of leprosy, and the number of cases found served as the "gold standard" against which the number of cases found by the RVS was measured. All cases found in the RVS were automatically included in the TVS.
Definition of a leprosy case. The operational definition of a leprosy case was: a person having clinical signs of leprosy, with or without bacteriological confirmation of the diagnosis, and requiring chemotherapy (5). The diagnosis was confirmed when at least one of the three cardinal signs (loss of sensation in a typical skin lesion, enlarged nerve, positive skin smear) were present. Therefore, a decision on classification was made on clinical and bacteriological grounds only; no biopsies were taken. An indeterminate skin-smear-negative person was not counted as a case.
Standardization. In a presurvey workshop, the researchers and leprosy supervisors standardized the method of physical examination, examination for signs of leprosy, and all other procedures. The information for the village headmen, the announcement by the headmen, and the announcement by the survey team to the village population were standardized as well.
The RVS and TVS methods were pretested in eight villages in February 1990 and, based on that experience, adjustments were made. During the survey, regular quality control checks (e.g., examination procedures, census procedures, information to the villagers) were made by the teamleader and the researchers.
Planning the time of survey implementation. During 1 week the RVS would be executed in (on average) four villages, 1 day per village (from the afternoon until the end of the next morning). The TVS was done in the same villages the week after. Therefore, on average, eight villages could be surveyed by the two methods in a 1-month period. The period October 1990-February 1991 was selected for the first round of surveys. The months of October to February, being dry and cool and the harvest season, were considered to be the most convenient time to obtain maximum participation.
Composition of rvs team. The RVS team consisted of one medical doctor, who was also the teamleader, one male and one female supervisor (all women were examined by female supervisors), one laboratory technician, one drug supplier and two drivers. All supervisors (including the laboratory technician and drug supplier) were senior and experienced staff from the Leprosy Control Centre, Zone 6, Khon Kaen.
Permission from authorities and information to villagers. Permission was sought from responsible authorities. The village headmen of the target villages were called for a meeting to inform them about the RVS 1 month before the start of the survey. One week before the date of the RVS the teamleader would visit the target villages and remind the village headman to inform the villagers about the RVS. After the arrival of the survey team at the village, a car with a loud-speaker broadcast a standardized message asking all people with skin problems, leprosy, and deformities to come for examination.
Making a list of cases, their contacts and suspects. Prior to the RVS, the health services were contacted to provide a list of registered leprosy patients (and their household contacts) in the target villages. After the arrival of the survey team, one of the supervisors had a group discussion with the village leaders (including village health volunteers) to collect the names of villagers identified as possibly suffering from leprosy. At the end of the afternoon on the day of arrival, the supervisor visited those persons on the list who had not yet presented themselves voluntarily at the examination station. The next morning one more attempt was made to trace those who had not yet been seen.
Examination of villagers. After arrival, the team set up the examination area (usually within the Buddhist temple compound) and examined villagers who reported themselves. The team stayed overnight in the village and was available for consultation until late at night and from early morning.
New patients found. The new leprosy patients were registered, given health education, supplied with 1 month of multidrug therapy (MDT) and referred to the general health service (appointment date given). Their household contacts were examined as well. The list of names and copies of the patients' records were given to the health staff responsible for leprosy control in the area.
TVS method. The TVS consisted of the following additional steps. After finishing the RVS, the village leaders were informed of the fact that a TVS would be conducted in 1 week's time. The population list was updated during the TVS. The census visit to the household was used to inform the people and to ask for cooperation (housenumber cards were supplied); the villagers were requested to report to the examination place. The completed examination sheets were collected by the dispenser at the last table before the individuals left the secluded examination area to make sure that nobody left the area without having been examined. In the following month, two supervisors traced and examined persons belonging to the census population who had been absent during the TVS. Several tracing visits (with a maximum of three visits) were made to the respective villages.
Cost estimates. Only the direct costs to the project for the organization of the surveys were calculated. Included were the supplies, car rent and fuel, and staff per diem. Not included in the cost estimates were salaries. However, the number of man-days worked (cluster information, standardization, survey test run, census, actual survey and tracing) is provided. The time spent on planning for the survey, the prcsurvey organization and on analyzing the survey results and reporting has not been calculated.
RESULTS
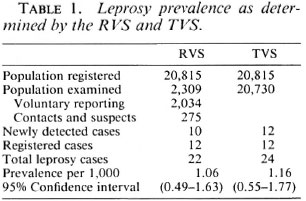
In the first round of surveys it was found that there was a high agreement between the two (RVS and TVS) methods. A second round was, therefore, not considered necessary. The sample population of the 40 villages available for analysis was 20,815. The attendance at the TVS was good initially (93.5%), and with tracing visits 99.6% were examined. The number of people reporting for examination during the RVS was on average 11% of the total village population (Table 1). The prevalence rates estimated by both the RVS and TVS were 1.06 and 1.16 per 1000, respectively (Table 1). These results are not significantly different, and the observed difference was considered to be of no practical importance.
The sensitivity of the RVS in detecting new cases (not yet registered) was 83% compared to the TVS: in total 10 new patients were found in the RVS and an additional two new patients (both paucibacillary patients with early leprosy) in the TVS. The reasons that the two patients were not found during the RVS were: one patient had not heard about the RVS. She went to the fields early in the morning and worked until late at night. Two years ago she had noticed a patch, but she never went for treatment. The other patient was away with her family for a few days during the RVS but came back 2 days before the TVS. Three months ago she had found a small patch, but never went for treatment. Of the 12 new cases found 11 were classified as PB (7 tuberculoid cases and 4 borderline tuberculoid cases) and only 1 as multibacillary borderline lepromatous leprosy. Most of the new PB cases found had only minor signs and symptoms. None of the new patients had any deformity.
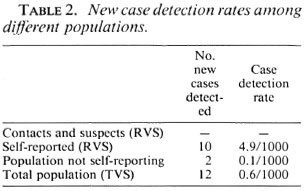
The detection rate among the self-reported group (RVS) was eight times higher than the rate among the TVS and almost 50 times higher compared with the population who did not report for examination (Table 2). None of the suspects which were notified during the group discussion with the village leaders were found to have leprosy.
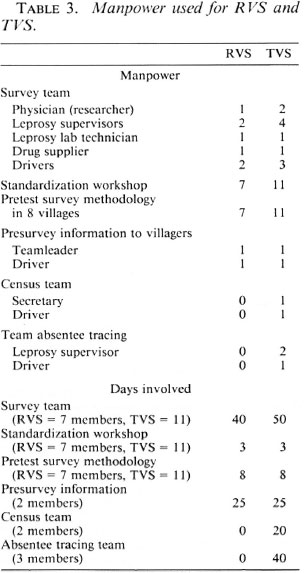
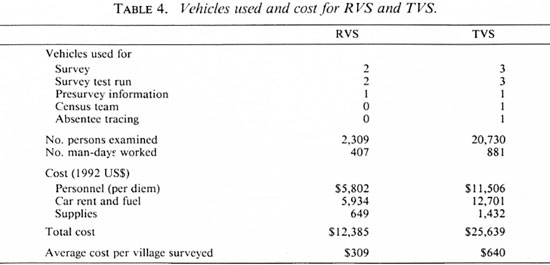
Altogether (Tables 3 and 4) the RVS mandays and costs were less than half of the TVS. The RVS man-days involved were 407; the TVS man-days 881. The average cost per cluster village (with an average population of 500 inhabitants) was US$309 for the RVS and US$640 for the TVS. The cost (and also the man-days) of the survey is higher than mentioned (Table 4) because the cost (man-days) of the preparation, analysis, salaries and consultants arc not included.
A detailed report on the study and all raw data can be obtained on request to the corresponding author.
DISCUSSION
In the first round of the survey it was found that there was a high agreement between the RVS and the TVS. It was decided that a second survey round would not add much precision to the outcome of the comparison between the two methods and was therefore, considered not necessary. The development of a simpler, less-expensive alternative to random sample surveys for determining the leprosy problem was the objective of this study. An RVS is less time consuming, easier to implement and the total costs are much less than those of a TVS (Table 4). The preparations are less strenuous (no need for a detailed census); only a fraction of the population has to be examined; the survey team can be much smaller and there is no need for tracing procedures (Table 3). For an RVS no detailed census is required: the estimated number of inhabitants residing in the village would be sufficient information which would, in most cases, be available from the village headman.
The quality of any survey depends upon clear definitions (e.g., a case of leprosy, village resident), well-trained personnel, rigorously maintained standards for procedures (including quality control), and a near 100% coverage of the population. The paramedical staffused in the survey were all staff of the regional leprosy control center with long experience in leprosy control. In case of doubt and to confirm the diagnosis, the medical officer and the consultant leprologist were consulted. The population coverage was already high during the TVS (93.5%) and was increased to 99.6% by absentee tracing within the month afterward. It may be concluded that the TVS was carried out well and that the number of patients found is probably very near the real prevalence of the sample.
No second TVS was carried out by an independent team to validate the result of the first TVS. It was considered not feasible to request examination of the same population three times. Nevertheless, within this study the TVS was considered to be the "gold standard" against which the validity of the RVS was tested. From the findings (Table 1), it was concluded that there was a high agreement between the two methods and that the RVS as implemented is a valid method to replace the TVS for the estimation of the extent of the leprosy problem. The RVS method depends on the willingness of the people to come forward and present their symptoms. Two additional new cases were found during the TVS. The crucial factor in their detection may have been a longer presence of the survey team in the village rather than examining people who did not report themselves.
The detection rate (Table 2) among the self-reporting group (RVS) was eight times higher than the rate among the TVS population. Additional factors for success of the RVS are clear information to the sample population and the optimal availability of the survey team by staying overnight in the village. Solutions for different (possibly less favorable) circumstances than in Khon Kaen should be explored and tested.
Whether the RVS will produce similar good results in other parts of the world needs some reflection (2). The RVS can be applied under low-endemic conditions. In case of an estimated prevalence rate of < 5 per 10,000, however, the sample size requirement will become too large even for an RVS, and the time and cost involved would be prohibitive. This also applies for the use of the RVS as a case-finding tool in low-endemic conditions.
It would be worthwhile to explore cheaper methods for conducting an RVS. One suggestion is to involve general health staff of the nearby health service in the survey. A disadvantage would be that this staff may be less experienced and may need extra training and guidance. However, if this staffwould be involved in the ongoing leprosy control activities, it would be a good in-vestment to train them. Therefore, such anapproach would be profitable only in highly endemic areas.
In combined leprosy and tuberculosis control programs with staff experienced in both diseases combined, an RVS obviously has advantages for the health service. In general, it seems to be cost effective to survey for more than one disease at the same time, especially if other, more or less similar groups of diseases with relatively low prevalence are added.
CONCLUSIONS
The RVS is a valid replacement of the TVS as conducted in Khon Kaen Province, Thailand. The RVS can be applied in lowendemic conditions and could (partly) be carried out by the general health staff. Another advantage of the RVS is that the population is disturbed less: no detailed census has to be made, only a minority of the population will have to be examined, and absentees do not have to be traced. When applying the RVS in another area, adaptations for different local circumstances need to be explored.
Acknowledgment. The MURLEP Project received financial support from the Netherlands Leprosy Relief Association (NSL), the Ministry of Education of The Netherlands and the European Union. We are grateful to the Ministry of Public Health and the University of Khon Kacn, Thailand; the Royal Tropical Institute, Amsterdam; and the NSL for their kind cooperation and support. We recognize the important contributions made by the staff of the Leprosy and Tuberculosis Zonal Control Centres, Khon Kacn; Dr. P. Fecnstra, Mr. I. Bijleveld, Dr. M. Elink Schuurman, Dr. K. Vaetecwootacharn and Dr. M. Borgdorff.
REFERENCES
1. BECHELLI, L. M., GARBAJOSE, P. G., GYI, M. M., UEMURA, K., SUNDARESAN, T., TAMONDONG, C,MARTÍNEZ-DOMÍNGUEZ, V., SANSARRICQ, H. and WALTER, J. Proposed method for estimating leprosy prevalence based on rates in children. Bull. WHO 48(1973)502-503.
2. CASABIANCA, M. N., KERKETTA, W. and ROY, P. K. A comparative study of the effectiveness of different methods of case detection in north India. (Abstract) Int. J. Lepr. 61(1993)38A.
3. SUNDARESAN, T. Issues involved in the rapid assessment of the leprosy problem. Lepr. Rev. 63 Suppl. (1992) lls-20s.
4. WORL D HEALTH ORGANIZATION. A guide to leprosy control. 2nd edn. Geneva: World Health Organization, 1988.
5. WORL D HEALTH ORGANIZATION. Report of a meeting on methods for the rapid assessment of the leprosy situation. Geneva: World Health Organization, 1988. WHO/CDS/LEP88.2.
1. M.D., Khon Kaen University; The MURLEP Project, P.O. Box 8, Khon Kaen University, Khon Kaen 40002, Thailand.
2. M.Sc, Khon Kaen University; The MURLEP Project, P.O. Box 8, Khon Kaen University, Khon Kaen 40002, Thailand.
3. M.D.; Khon Kaen University; The MURLEP Project, P.O. Box 8, Khon Kaen University, Khon Kaen 40002, Thailand.
4. Ph.D., Khon Kaen University; The MURLEP Project, P.O. Box 8, Khon Kaen University, Khon Kaen 40002, Thailand.
5. M.D.; NSL Khon Kaen Project; The MURLEP Project, P.O. Box 8, Khon Kaen University, Khon Kaen 40002, Thailand.
6. M.P.H., NSL Khon Kaen Project; The MURLEP Project, P.O. Box 8, Khon Kaen University, Khon Kaen 40002, Thailand.
Received for publication on 28 March 1995;
Accepted for publication in revised form on 14 November 1995.
*In the MURLEP project four groups worked together: the Khon Kaen University (Faculties of Medicine and Public Health); the Thai Ministry of Public Health (Provincial Health Office, Khon Kaen and the Communicable Disease Control Office, Leprosy and TB Zonal Centers, Zone 6, Khon Kaen); the Royal Tropical Institute (KIT), Amsterdam; and the Netherlands Leprosy Relief Assocation (NSL).