- Volume 64 , Number 2
- Page: 166–8
Discoid lupus erythematosus and lepromatous leprosy
In an effort to increase the utility of the JOURNAL in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
Leprosy can, in our experience, be confused with lesions from a number of otherdiseases, prominent among which are gran-uloma annulare, granuloma multiforme,pseudolymphoma, Jessner's lymphocyticinfiltrate, eosinophilic granuloma, leish-maniasis, sarcoidosis, syphilis, morphca,tines, lupus vulgaris and necrobiosis lipoid-ica which is frequently anesthetic.1 Even sporotrichosis may be considered within thedifferential diagnosis.2 In addition, a patientmay, of course, have more than one disease.
Case report. A 30-year-old woman hadbeen diagnosed as having multibacillary(MB) leprosy by a medical assistant in October 1993 in Battambang, Cambodia. Slitskin smears were reported as being positiveat that time, and she was registered andtreated with multidrug therapy as recom-mended by the World Health Organization(WHO/MDT) for MB leprosy.3Findings atregistration had included several erythem-atous plagues, mostly on the body, but therewere no enlarged nerves or disabilities. During subsequent months a type 2 reaction wasdiagnosed on several occasions by the medical assistant who started treatment with upto 40 mg of prednisolone/day on each occasion. These type 2 reaction symptoms wereonly poorly described and were never confirmed by the supervisor.
In view of this history of recurrent type2 reactions, the patient was reviewed by JMPand DL in May of 1994. On the basis of thefacial lesions a diagnosis of discoid lupuserythematosus was made (Fig. 1). Althoughit was not feasible to carry out any confirmatory laboratory examinations, the diagnosis of discoid lupus erythematosus satisfactorily explained all skin lesions found, including the few seen on the rest of thebody, and it was assumed that the diagnosisof lepromatous leprosy made in October of 1993 was incorrect and that the slit-skinsmears had been misread. On the other hand,there remained a slight suspicion that theright superficial radial nerve was enlarged.Therefore, a split-nerve biopsy was takenunder local conditions.
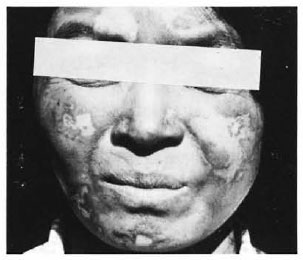
Fig. 1. Typical white atrophic lesions of discoidlupus erythematosus on the face of the patient.
The result of the histopathological examination by SL was as follows: the nervebiopsy showed a chronic, active, lepromatous leprosy neuritis with a bacterial index of 4.5 (fragmented). There was no influx of polymorphonuclear cells to support the diagnosis of intraneural erythema nodosum leprosum (Figs. 2 and 3).

Fig. 2. Longitudinal section of the right superficial radial nerve showing clusters of acid-fast bacilli (Fitc-Faraco stain).
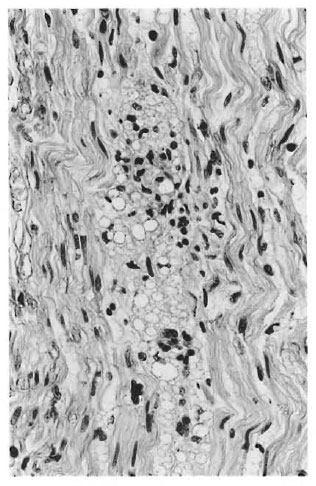
Fig. 3. Longitudinal section of the right superficial radial nerve showing neuritis (hematoxylin and cosin stain).
In June of 1994 the patient began treatment for discoid lupus erythematosus in addition to WHO/MDT for MB leprosy.
Discussion. The simultaneous occurrence of lupus erythematosus and leprosy has rarely been reported. In a case reported in 1967 lepromatous leprosy and systemic lupus erythematosus appear to have run a parallel course without clear indication which started first.4 Lepromatous leprosy was only diagnosed 13 years after the onset of symptoms of one or the other or both diseases. In a Japanese patient, systemic lupus erythematosus developed many years after lepromatous leprosy had been diagnosed.5 The patient received dapsonc and rifampin but the authors concluded that the patient did not suffer from a drug-induced lupus erythematosus. In a case reported in 1987, systemic lupus erythematosus was treated for 8 years with high dosages of prednisone before leprosy developed.6 The authors did not classify the type of leprosy, but from their description it would appear that the patient had borderline tuberculoid leprosy.3 Another case of systemic lupus erythematosus and lepromatous leprosy was presented at the 14th International Leprosy Congress.7 However, no details have been published so far.
We describe a patient for whom lepromatous leprosy and discoid lupus erythematosus appear to have developed at the same time. The diagnosis of lepromatous leprosy is based on a split-nerve biopsy (Figs. 2 and 3), the diagnosis of discoid lupus erythematosus on typical skin lesions as shown in Figure 1. We believe that one of these diseases can easily be overlooked in the presence of the other one. In particular, in the tropics where a patient may well have more than one skin disease, it can be misleading to try to explain all signs and symptoms with one diagnosis. A careful examination and an open mind, supported by access to biopsy pathology, remain the essential tools of a dermatologist supervising a leprosy control service.
- Jörg Martin Pönnighaus, Dr.Med.,
D.T.P.H. (London).
- Dirk Landwehr, Dr.Med.
Universitats-Hautklinik
66421 Homburg, Saar, Germany.
- Sebastian Lucas, F.R.C.P., F.R.C.Path.
Department of Histopathologv
UCL Medical School
London WC1E 6JJ, U.K.
1. Mann, R. J. and Harmann, R. R. Cutaneous anaesthesia in necrobiosis lipoidica. Br. J. Dermatol. 110(1984)323-325.
2. Mehta, S. D., Handa, U., Dawn, G., Handa, S. and Kaur, I. Borderline lepromatous leprosy masquerading as lymphocutaneous sporotrichosis. (Letter) Lepr. Rev. 66 (1995) 259-260.
3. Bryceson, A. and PfaltzgrafT, R. E. Leprosy. 3rd cdn. Edinburgh: Churchill Livingstone, 1990.
4. Bonomo, L., Dammacco, F., Tursi, A. and Barbieri, G. Lupoid features in a case of leprosy. Int. J. Lepr. 35(1967)65-71.
5. Ohkawa, S., Ozaki, M. and Izumi, S. Lepromatous leprosy complicated with systemic lupus erythematosus. Dermatológica 170(1985 80-83.
6. Posner, D. I. and Guill, M. A. Coexistent leprosy and lupus erythematosus. Cutis 39(1987)136-138.
7. Arunthati, S., Kumar, K. S. and Samuel, J. Systemic lupus erythematosus in a lepromatous leprosy patient: a diagnostic and therapeutic problem. (Abstract) Int. J. Lepr. 61(1993)28A.