- Volume 64 , Number 3
- Page: 306–10
Silent Iritis in treated bacillary negative leprosy
ABSTRACT
Iridectomy specimens f rom 59 leprosy patients who had adequate medical records of whom 33 belong to the lepromatous (LL) leprosy variety and 16 normal controls were studied histopathologically. All patients were bacteriologically negative and had received dapsone followed by multidrug therapy (MDT), or MDT only, or only dapsone for varying periods. It was found that leprosy, particularly lepromatous disease, did not significantly decrease the age of formation of cataract. Of the 33 LL patients studied 60.6% had silent iritis. The duration of treatment had no obvious influence on the persistence of iritis. Treatment with only 2 years of MDT for LL patients did not significantly increase the prevalence of persistent silent iritis compared to those who received other types of antileprosy therapy for long periods. It is pointed out that chronic iritis is a serious complication that continues even after the patient is declared clinically and bacteriologically cured, especially in patients who had a history of chronic iritis clinically.RÉSUMÉ
On a étudié en histopathologic des échantillons d'iris de 59 malades de la lèpre qui avaient des dossiers appropriés, et dont 33 appartenaient à la variété de la lèpre lépromateuse, et également de 16 témoins normaux. Tous les patients étaient négatifs en bactériologie et avaient reçu de la dapsone suivie par une polychimiothérapie (PCT). ou une PCT seule, ou de la dapsone seule pour différentes durées. On a trouvé que la lèpre, particulièrement la maladie lépromateuse, n'a pas réduit de manière significative l'âge de formation de la cataracte. Parmi les 33 patients LL étudiés, 60.6 % avaient un iritis à bas bruit. La durée du traitement n'avait pas d'influence évidente sur la persistance de I'iritis. Le traitement avec seulement deux ans de PCT pour les patients LL n'a pas augmenté signilicativement la prévalence de I'iritis persistant à bas bruit, par comparaison à ceux qui ont reçu d'autres types de traitements anti-lèpre pour de longues périodes. Il est souligné que I'iritis chronique est une complication sérieuse qui continue même après que le patient ait été déclaré cliniquement et bactériologiquement guéri, particulièrement chez ceux qui avaient une histoire clinique d'iritis chronique.RESUMEN
Se hizo cl estudio histopatológico de los especímenes de tridectomía tomados de 59 pacientes con lepra que contaban con expedientes médicos adecuados de los cuales 33 correspondieron a pacientes lepromatosos (LL). Se incluyeron ademñs 16 especímenes de individuos normales. Todos los pacientes fueron bacteriológicamente negativos y habían recibido dapsona y después poliquimioterapia (PQT), o sólo la PQT. o sólo la dapsona, esta última administrada por periodos variables de tiempo. Se encontró que la lepra en general y la lepra lepromatosa en particular, no disminuyeron la edad de aparición de cataratas. De los 33 pacientes LL estudiados, en el 60.6% de los casos se detectó iritis silente. La duración del tratamiento no tuvo una influencia obvia sobre la persistencia de la iritis. El tratamiento pro sólo 2 años con PQT de los pacientes LL no aumentó significativamente la prevalencia de la iritis silente persistente ya que ésta fue similar a la observada en los pacientes sujetos a otros tratamientos antileprosos durante periodos mñs prologados de tiempo. Se hace notar que la iritis crónica es una complicación seria que continúa apareciendo en los pacientes aun después de que estos han sido declarados clínica-y bacteriológicamente curados.In lepromatous (LL) leprosy the iris and ciliary body are known to be common sites of infection with Mycobacterium leprae (3). Although they are infiltrated with lymphocytes, plasma cells and macrophages packed with acid-fast bacilli (AFB) (2), clinically there are no obvious signs of inflammation. During erythema nodosum leprosum (ENL), an acute iridocyclitis characterized by intense pain, edema, hyperemia of the eye, turbid aqueous, and keratotic precipitates can occur (1). There is also a silent phase of chronic asymptomatic iridocyclitis which persists with occasional attacks of ENL in some LL patients even 25 years after the patients' bacterial index (BI) had become negative (personal observations, CKJ). It has been suggested that the iris might be a site in which M. leprae would survive long after skin smears have become negative (5).
In this study we plan to evaluate the prevalence of silent iritis by examining iris specimens from resolved skin-smear-negative leprosy patients and to study their histopathologic appearance compared to that of normal individuals.
MATERIALS AND METHODS
Cataract operations are regularly performed in leprosy and nonleprosy patients in the Purulia Leprosy Home and Hospital, West Bengal, India. During surgery an iridectomy is invariably done. Specimens of iris removed during iridectomy of clinically inactive and skin-smear-negative leprosy patients were obtained. Similarly available iridectomy specimens from normal people served as controls. The iris tissues soon after removal were fixed in 10% buffered neutral formalin, processed for paraffin sections, cut into 5- µ m sections, stained with hematoxylin and eosin (H&E) and a modified Fite's stain (4), and examined with a light-microscope. The H&E sections were examined for evidence of inflammation and other histopathologic changes. The sections stained with the modified Fite's stain were examined for AFB under an oil immersion lens.
Patients were clinically classified according to the Ridley-Jopling classification. The age, sex, duration of disease, and history of antileprosy therapy were recorded. Skin smears were checked to confirm that they were negative for AFB.
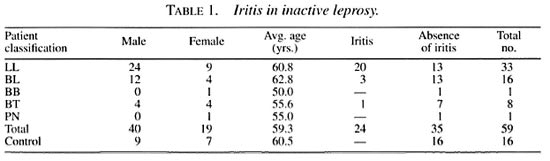
Iris biopsies from 59 patients with adequate clinical and laboratory records and 16 controls were available for study (Table 1). There were 40 males and 19 females among the patients and 9 males and 7 females among the controls. The ages of the patients were between 45 and 82 years (mean 59.3 years) and the controls were between 50 and 80 years (mean 60.5 years). Of the 59 patients, 33 were classified as polar lepromatous (LL) leprosy, 16 as borderline lepromatous (BL), 1 as midborderline (BB), 8 as borderline tuberculoid (BT) and 1 as pure neural (PN) leprosy.
RESULTS
On histopathological examination of the 16 control iris specimens, there were very few scattered lymphocytes, and there was no evidence of inflammation in any of them. However, almost all of them showed evidence of atrophy and several small blood vessels had thick hyalinized walls. Of the 33 LL patients, 20 showed varying degrees of inflammatory reaction in addition to signs of atrophy. The inflammatory infiltrate consisted of lymphocytes, plasma cells, mast cells and macrophages. Many of the macrophages were packed with melanin pigment (Fig. 1). In one patient there was a dense focal collection of lymphocytes (Fig. 2). Although in some specimens there were occasional eosinophils and neutrophils, they were far too few to be considered as evidence of acute inflammation. Small blood vessels with thick hyalinized walls, as seen in the controls, were present in some (Fig. 3). Specimens from the other 13 LL patients showed evidence of atrophy but no inflammation. Of the 16 BL patients 3 showed similar inflammatory changes as described above and 13 were free from inflammation. The specimens from all 8 BT patients except 1, the one BB patient, and the 1 PN patient showed only evidence of atrophy but no significant inflammatory changes.
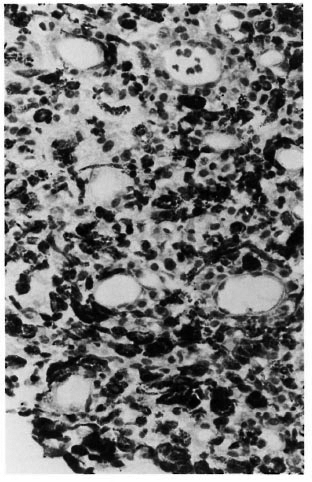
Fig 1. Photomicrograph of iris showing markedinfiltration with lymphocytes, plasma cells, mast cellsand melanophages (H&xE400).

Fig. 2. Photomicrograph showing dense collection of lymphocytes in the iris (H&E x400).

Fig . 3. Photomicrograph of iris showing presenceof several small blood vessels with thick hyalinifedwalls (H&E x400).
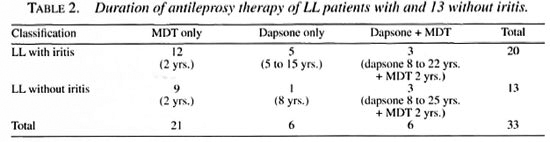
Since the overwhelming majority of iritis was found in LL patients further analysis was done only on LL patients. The average duration of the disease of 20 LL patients who had iritis was 31.5 years; that of the 13 who did not have iritis was 29.7 years. The duration and type of therapy given to the 20 LL patients who had iritis was: 5 (25%) had only dapsone for periods varying from 5 to 15 years with an average of 6.8 years; 12 (60%) had only multidrug therapy (MDT) as recommended by the World Health Organization (WHO) for multibacillary (MB) patients (6) for 2 years and 3 (15%) had dapsone for periods varying from 8 to 22 years (mean 17.3 years) followed by MDT lor 2 years (Table 2). The duration and type of therapy given to the 13 LL patients who had no iritis was: 1 (7.7%) had only dapsone for 8 years; 9 (69.2%) had only MDT for 2 years; and 3 (23.1%) had dapsone for periods varying from 8 to 25 years (mean 12.7 years) followed by MDT for 2 years (Table 2).
DISCUSSION
The average age of the normal controls with cataract in this study was 60.5 years, that of all leprosy patients was 59.3 years, and that of only LL patients was 60.8 years. It is apparent that the age incidence of cataract in leprosy patients, and especially in lepromatous patients, is not significantly different from that of controls. Therefore, it is reasonable to suggest that leprosy, particularly lepromatous disease, may not contribute significantly to the development of cataract. However, it must be noted here that all of the leprosy patients in this study had "mature" cataracts and therefore might have had the cataracts for a long time.
Of the 59 iris specimens examined, 24 (40.7%) had signs of asymptomatic chronic or silent iritis. Of these 24, 20 were from the 33 LL patients (60.6%), 3 from the 16 BL patients (18.8%), and 1 from the 8 BT patients (12.5%). It is obvious that a significant number (46.9%) of MB patients, especially those belonging to the LL group (60.6%), had chronic iritis. There was evidence of persistent inflammation after they were clinically and bacteriologically declared disease arrested. It is interesting that no stainable organisms were detected in the iris specimens. The persisting inflammation might be due to lingering bacterial antigens, possibly including some solid-staining bacilli which were far too few to be detected in a light-microscopic study. It would be interesting to look for M. leprae and its antigens using immunologic and polymerase chain reaction (PCR) techniques. Since there were no stainable organisms in the light-microscopic study, it is highly unlikely that there would be enough viable M. leprae in the iris to initiate a relapse. However, the antigens persisting in a significant amount were adequate to maintain a chronic inflammation. It must be mentioned here that of the 20 LL patients with pathologic evidence of chronic iritis only one had chronic iritis clinically which was controlled by treatment but he continued to have flare tips post-opcratively. Therefore, lepromatous patients, although they may be pronounced cured or disease arrested after 2 years of MDT, should be monitored for eye complications especially if at any time previously they had had iritis clinically.
The presence of chronic inflammation in one BT patient is difficult to explain. From the records we find that he was treated with dapsone for 20 years followed by MDT for 2 years and, therefore, it is possible that there might be a clerical error in the entry. The other possibility is that this patient was one among the "occult multibacillary patients" in whom although the skin smears were negative antigens of M. leprae might persist in the skin, peripheral nerves and even in the iris.
The numbers studied are too small to derive definite conclusions on the presence of iritis in relation to the duration and type of drugs the patients received. However, it appears that iritis was more common among those who received only dapsone. Further, the duration of treatment seems to have no significant effect on the persistence or disappearance of iritis. MDT given only for 2 years was found to have the same effect in controlling iritis as prolonged administration of antileprosy drugs such as dapsone or dapsone followed by MDT.
Acknowledgment. We are grateful to the American Leprosy Mission International, Greenville, South Carolina, U.S.A., for continued financial support for the histopathologic studies and to Miss K. Jayanthi and Mrs. Shikha Mandai for secretarial help.
REFERENCES
1. Brand, M. E. and Ffytche, T. J. Eye complications of leprosy. In: Leprosy. 1st edn. Hastings, R. C ed. Edinburgh: Churchill Livingstone. 1985, pp. 223-242.
2. Desikan, K. V. and Jon. C. K. Report on the study of eye lesions in three autopsied cases of leprosy. Lepr. India 42(1970)1-3.
3. Holmes, W. J. Leprosy of the eye. Lepr. Rev. 28(1957)108-123.
4. Job, C. K. and Chacko, C. J. G. A modified Fite's stain for demonstration of M. leprae in tissue sections. Indian J. Lepr. 58(1986)17-18.
5. Joffrion, V. C. Ocular leprosy. In: Leprosy. 2nd edn. Hastings, R. C., ed. Edinburgh: Churchill Livingston. 1994. pp. 353-364.
6. Who Study Group. Chemotherapy of Leprosy for Control Programmes. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
1. F.R.C.S., Purulia Leprosy Home and Hospital, Purulia 723 101, West Bengal, India.
2. M.D., F.R.C.Path., Consultant Pathologist, St. Thomas Hospital and Leprosy Center, Chettupattu 606 801, T.S. District, Tamil Nadu, India.
Reprint requests to Dr. Job.
Received for publication on 23 February 1996.
Accepted for publication in revised form on 13 May 1996.