- Volume 64 , Number 3
- Page: 320–3
Antiphospholipid antibodies thrombotic syndrome misdiagnosed as Lucio's phenomenon
In an effort to increase the utility of the Journal in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
The antiphospholipid syndrome (APS) is characterized by the presence of anticardiolipin antibodies (ACA) or lupus anticoagulant (LA), or both, associated with recurrent venous and arterial thromboembolic phenomena, livedo reticularis, thrombocytopenia, and recurrent fetal loss.1,2 APS is associated with systemic lupus erythematosus (SLE)3 or may exist alone in non-SLE patients with clinical features attributable to ACA (the "primary" antiphospholipid syndrome; PAPS). Antiphospholipid antibodies have been reported in leprosy patients in 50% to 80% of multibacillary individuals,4-7 also being used for diagnostic purposes.8 No association was noted between the presence of ACA with the occurrence of Lucio's phenomenon or erythema nodosum leprosum (ENL) in one study,7 and ACA-positive patients did not show the presence of any pathological feature associated with the APS in another.4
In this communication we report a patient with treated lepromatous leprosy presenting with features of the APS with recurrent arterial and venous thrombosis, livedo reticularis, and positive anticardiolipin antibodies. We were not able to find any similar case in the literature. The differential diagnosis of APS with Lucio's phenomenon is of great importance, especially regarding the prognosis.
CASE REPORT
A 30-year-old, Caucasian, Brazilian female was referred with a history of recurrent necrotic lesions on the skin, mostly on the extremities, of 6 months' duration. She was in her 18th month of multidrug therapy (MDT) for lepromatous leprosy, and showed no signs of active disease. She had been treated in her city with oral steroids for Lucio's phenomenon during the former episodes.
A cutaneous examination revealed ciliary and superciliary madarosis. The face was mildly infiltrated. On both cheeks, thighs, and lower abdomen bluish reticulated patches of livedo reticularis were observed.
On both legs, feet and forearms irregular necrotic ulcers of different shapes and sizes were seen, more intense on the lower limbs (Fig. 1). Several of these were covered by black eschar. Gangrene of the toes and forefoot was very prominent (Fig. 2).

Fig. 1. Irregularly shaped extensive necrotic ulcerations partially covered by eschar on lower limb.

Fig. 2. Gangrene of left four toes and forefoot.
Ecchymotic necrosis of the fingertips was present (Fig. 3). The tip of the 5th finger of the left hand underwent spontaneous amputation during a previous episode of the lesions.
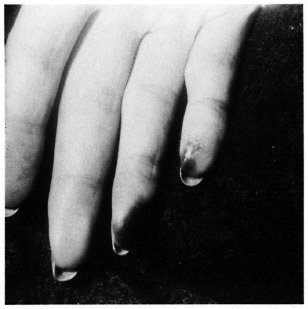
Fig. 3. Ecchymotic necrotic plaques on fingertips.
A routine laboratory examination of blood showed microcytic anemia and lymphopenia. Prothrombin time was slightly raised and fibrinogen was increased. The antinuclear factor was positive 1/640, showing a peripheral pattern. ANA antibodies, cryoglobulins and the Coombs test were all negative. C3 and C4 values were within normal ranges. The VDRL test was reactive 1:4 with a negative FTA-ABS test. The IgM class of ACA was positive; other classes of immunoglobulins were not available. Proteins C and S for coagulation had normal levels.
Skin biopsies showed ischemic infarction with epidermal and dermal necrosis. Dermal and hypodermal blood vessels showed massive thrombosis sometimes with partial recanalization (Fig. 4) and slight inflammatory infiltrate around the vessels, probably due to thrombosis. Stains for acid-fast bacilli (AFB) were negative.
She was treated with oral prednisone (1 mg/kg/day) and warfarin anticoagulation, an international normalized ratio (INR) of 1.5, with excellent recovery of most necrotic skin lesions. However, amputation of the right foot, of toes of the left foot, and the distal phalanges of two fingers was necessary due to the mummified, dry. irreversible gangrene of these anatomical areas. Multidrug therapy (MDT) for her leprosy was maintained normally.
DISCUSSION
ACA are immunoglobulins of the IgG or IgM class that react with negatively charged phospholipids.9 A serum cofactor (beta-2glycoprotcin I, or apolipoprotein H) dependence has been pointed out for this binding.6The interaction of cardiolipin and beta-2-GPI leads to a conformational change in cardiolipin with exposure of the immunogenic epitope and induction of ACA.10
ACA are associated with autoimmune diseases, such as systemic lupus erythematosus (SLE),3or may exist alone in non-SLE patients presenting clinical features attributable to ACA (the so-called PAPS).11,12
Among others, ACA may also appear in viral (infectious mononucleosis, HIV infection) or bacterial (Q fever, syphilis and leprosy) disorders4,5,7,13 Clinical and laboratory features of both APS and PAPS can be variable.12 The exact reason why some ACA produce thrombosis or other clinical manifestations while others do not is still unknown. Testing for ACA is essential for identifying patients with unexplained vascular occlusive disease.14
In the classical picture of Lucio's phenomenon, or erythema necroticans, painful and tender red patches appear on the skin, particularly on the extremities. These triangular or irregular patches become purpuric, their center becomes necrotic and ulcerated, producing a black eschar which falls off after a few days to leave a superficial atrophic scar15-17. Furthermore, Lucio's phenomenon is primarily a necrotizing vasculitis, with necrosis in the walls of superficial vessels, and focal endothelial proliferation of mid-dermal vessels, with epidermal necrosis. AFB are found in large numbers in endothelial cells.18 Gangrene of the extremities or deep tissue necrosis are not part of the clinical picture of Lucio's phenomenon because to produce them an occlusion of larger and deeper blood vessels is required, as encountered in this patient.
Gangrene, livedo reticularis, deep-vessel thrombosis and positive ACA were the most important features in our patient. The presence of livedo reticularis, although not infrequently encountered in lepromatous leprosy, together with gangrene was helpful in suggesting APS since it is one of the characteristics of the syndrome in patients without leprosy. Since our patient did not fulfill the minimum of four diagnostic criteria for SLE suggested by the American College of Rheumatologists,19 we considered the presence of APS associated with ACA in leprosy as a diagnostic possibility in her case. Furthermore, in histology, thrombosis of deep blood vessels without necrotizing vasculitis and negative stains for AFB in endothelial cells make the diagnosis of Lucio's phenomenon quite unlikely.
Although former studies did not correlate ACA to any clinical alteration in leprosy, an association to the antiphospholipid thrombotic syndrome, apparently a rare clinical finding in leprosy, should be kept in mind when evaluating a Iepromatous patient with severe necrotic lesions. In APS these lesions could be very mutilating, producing a severe physical handicap in the affected patient, even though treated with anticoagulation. In Lucio's phenomenon the prognosis is relatively better since, normally, the necrotic lesions leave superficial atrophic scars after resolving.
- Lucio Bakos, M.D Ph.D.
Cecilia C. Correa, M.D.
Larissa Bergmann, M.D.
Renan R. Bonamigo, M.D.
Luiz F. Bopp Muller, M.D.
Service of Dermatology
Department of Internal Medicine
Hospital de Clinicas de Porto Alegre
Federal University of Rio Grande do Sul
Rua Ramiro Barcelos 2350
90035-003 Porto Alegre, Brazil
1. Asherson, R. A. A "primary" anti-phospholipid syndrome. J. Rheumatol. 15(1988)1742-1746.
2. Lockshin, M. D. Anti-cardiolipin antibody. (Editorial) Arthritis Rheum. 30(1987)471-477.
3. Alarcon-Segovia, D Deleze, M Oria, C. V Sanchez-Guerrero, J Gomez-Pacheco, L Cabiedes, J.. Fernandez, L. and Ponce de Leon, S. Antiphospholipid antibodies and the antiphospholipid syndrome in systemic lupus erythematosus. A prospective analysis of 500 consecutive patients. Medicine (Baltimore) 68(1989)353-365.
4. Escobar-Gutierrez, A Amezcua-Chavarria, M. E Castro, E Flores, O. and Rodriguez, O. Anti-cardiolipin antibodies in Mexican lepromatous leprosy patients. (Letter) Int. J. Lepr. 58(1990)723-724.
5. Furukawa, F, Kashihara, M Imamura, S Oshiho, G. and Hamashima, Y. Evaluation of anticardiolipin antibody and its cross-reactivity in sera of patients with lepromatous leprosy. Arch. Dermatol. Res. 278(1986)317-319.
6. Ordi, J Selva, A Monegal, F, Porcel, J. M Martinez-Costa, X. and Vilardell, M. Anticardiolipin antibodies and dependence of a serum cofactor; a mechanism of thrombosis. J. Rheumatol. 20(1993)1321-1324.
7. Quismorio, F. P Jr. and Rea, T. 11. Serum antiphospholipids in leprosy. (Abstract) Int. J. Lepr. 56(1988)682.
8. Fiallo, P Cardo, P. P. and Nunzi, E. Higher specificity in the serodiagnosis of leprosy by combined titration of antiphenolic glycolipid-I and antiphospholipid antibodies. Int. J. Lepr. 61(1993)464-466.
9. Harris, E. N. Annotation. Br. J. Haematol. 73(1989)139-142.
10. Canoso, R. T. Antiphospholipid antibodies; basic mechanisms, clinical features, and animal models. Stroke 24(1993)1124-1125.
11. Asherson, R. A Khamastha. M. A Ordi-Ros, J Derksen. R. H Machin, S. J Garquinero. J., Outt, H. H Harris, E. N Vilardell-Torres, M. and Hughes, G. R. The "primary" antiphospholipid syndrome: major clinical and serological features. Medicine (Baltimore) 68(1989)366-374.
12. Vianna, J. L., Khamashta, M. A., Ordi-Ros, J Font. J., Cervera, R Lopez-Soto, A Tolosa. C. Franz J Selva, A Ingelmo, M et al. Comparison of the primary and secondary antiphospholipid syndrome: a European Multiccnter Study of 114 patients. Am. J.Med. 96(1994)3-9.
13. Vaarala, O Palosuo, T. Kleemola, M. and Ako, K. Anticardiolipin response in acute infections. Clin. Immunol. Immunopathol. 41(1986)8-15.
14. Bacharach, J. M., Lie, J. T. and Homburger. H. A. The prevalence of vascular occlusive disease associated with antipospholipid syndromes. Int. Angiol. 11(1992)51-56.
15. Jopling. W. H. and McDougall, A. C. Handbook of Leprosy. 4th edn. London: Heinemann Professional Publishing, 1988, pp. 90-91.
16. Pfaltzgraff, R. E. and Bryceson, A. Clinical leprosy. In: Leprosy. 1st edn. Hastings, R. C, ed. Edinburgh: Churchill Livingstone. 1985, pp. 171-172.
17. Rea, T. H. and Levan, N. E. Lucio's phenomenon and diffuse non-nodular lepromatous leprosy. Arch. Dermatol. 114(1978) 1023-1028.
18. Rea.T. II. and Ridley. D. S. Lucio's phenomenon: a comparative histological study. Int. J. Lepr. 47(1979)161-166.
19. Tan, E. M, Cohen, A. S Fries, J. F Masi, A. T, McShane, I). S Rothfield, N. F Schaller, J. G., Talal, N. and Winchester, R, J. The 1982 revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum. 25(1982)1271-1277.