- Volume 64 , Number 4
- Page: 392–5
Short-term follow up of patients with multibacillary leprosy and HIV infection
ABSTRACT
During a period of 9 years, four male patients with HIV and Hansen's disease were detected in Tamil Nadu, South India. The sequence as to which infection came first is not known. All had high-risk sexual behavior with commercial sex workers and a past history of genital ulcer disease. Their spectrum of leprosy was multibacillary. Patient no. 1 had pure neural leprosy of the lepromatous type, which is rare. He also had a single episode of type 1 reaction which did not require steroid therapy. Despite having taken inadequate treatment, patient no. 2 remained clinically and bacteriologically quiescent after 4 years of follow up. He had a low CD4 count of 330 cells/mm3. The third patient completed a full course of multibacillary multidrug therapy, and a year later is clinically and bacteriologically inactive. The fourth patient died of AIDS within 2 months of the dual diagnosis.RÉSUMÉ
Au cours d'une période de neuf ans, on a détecté quatre patients de sexe masculin avec une infection à VIII et une maladie de Hansen au Tamil Nadu, dans le Sud de l'Inde. Nous ne savons pas dans quel ordre ces deux infections sont apparues. Tous avaient un comportement sexuel à haut risque avec des professionnels du sexe, et certains avaient une histoire d'ulcère génital. Le type de la maladie était multibacillaire. Le patient no. I avait une lèpre nerveuse pure de type lépromateux, ce qui est rare. Il avait aussi un épisode unique de réaction de type 1, qui n'a pas requis de traitement par steroïdes. En dépit d'un traitement inadéquat, le patient no. 2 est resté cliniquement et bactériologiquement inactif après 5 ans de suivi. Il avait un faible taux de CD4 de 330 cellules/mm'. Le troisème patient a terminé un traitement complet de polychimiothérapie pour multibacillaires, et un an plus tard est cliniquement et bactériologiquement inactif. Le quatrième patient est mort de SIDA dans les deux mois qui ont suivi le double diagnostic.RESUMEN
En un periodo de 9 años se detectaron cuatro pacientes masculinos con HIV y enfermedad de Hansen en Tamil Nadu, al sur de la India. No se sabe cual enfermedad apareció primero. Todos tuvieron comportamiento sexual de alto riesgo y algunos una historia de úlcera genital. Su tipo de lepra fue multibacilar. El paciente No. I tuvo lepra neural pura del tipo lepromatoso, la cual es rara. También tuvo un episodio único de reacción leprosa tipo 1 que no requirió terapia con esteroides. No obstante haber tomado tratamiento inadecuado, el paciente No. 2 permaneció clínica-y bacteriológicamente quiescente después de 5 años de sequimiento. Este paciente tuvo una cuenta baja de células CD4 (330 por mm3). El tercer paciente completó su tratamiento con poliquimioterapia y un año después aún permanece clínica- y bacteriológicamente negativo. El cuarto paciente murió de SIDA dos meses después de diagnosticarse las dos enfermedades.The most common opportunistic disease in human immunodeficiency virus (HIV)positive persons is tuberculosis, as seen in subSaharan Africa and India (5-7). Early controlled studies of leprosy patients in Africa found a prevalence of HIV seropositivity with a range varying widely from 1.3% to 33% (11,12). Prevalence studies in India prior to 1989 by Shiv Raj, et al. from Delhi showed that patients with leprosy and controls were negative for HIV infection, but this was during the early part of the epidemic in India (16). More recent studies have not found significant differences between leprosy patients and controls in countries where both diseases are endemic (8,14,15). However, Borgdorff, et al. found that HIV-1 is a risk factor for the development of multibacillary (MB) leprosy (2).
MATERIALS AND METHODS
Ever since the detection of HIV infection in our hospital in 1986, patients attending the sexually transmitted disease (STD) clinic are counselled and screened for HIV antibodies using an ELISA (Wellcozyme; Wellcome Diagnostics, Dartford, Kent, U.K. or Vironostika; Organon Teknika, Boxtel, The Netherlands) since they form a high-risk group. ELlSA-positive samples are confirmed by the Western blot test (WB; Du Pont Company, Wilmington, Delaware, U.S.A. or Technoply, Singapore). All patients who were detected as having both HIV infection and leprosy were included in the study.
RESULTS
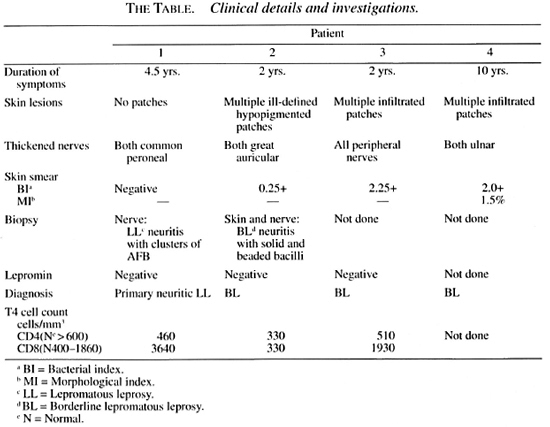
During the last 9 years, we detected four males with HIV infection and leprosy from the STD clinic. All were from Tamil Nadu in South India, and their ages ranged from 20 to 27 years. All had multiple heterosexual contacts with commercial sex workers (CSW) and a past history of genital ulcer disease. Their clinical details and investigations are shown in The Table. They were in the MB spectrum of the disease as evidenced by the presence of numerous acid-fast bacilli (AFB) in the nerve biopsy in case no. 1 and positive skin smears in the other three cases. Mitsuda tests done in three patients were negative, which is consistent with the MB spectrum of Hansen's disease (HD).
DISCUSSION
Although all four patients had HIV infection and HD, the sequence of infection as to which came first is not known. The first case report of HD and HIV infection was by Lamfers in 1987 in a 43-year-old homosexual with borderline tuberculoid (BT) HD (10). Subsequently, there were reports of both MB and paucibacillary (PB) HD associated with HIV infection by Bwire and Kawuma (3), Kennedy, et al. (9), and Vreeburg (17).
Incidence of type 1 reaction and neuritis was seen more among HIV-positive HD patients as reported by Bwire and Kawuma (4) in 9 out of 12 MB patients and by Vreeburg in 4 out of 8 PB patients (17). Among our patients, only one developed a type 1 reaction (at the time he was also detected to be HIV positive) and this rapidly recovered with nonsteroidal antiinflammatory drugs. Observation of the patient for 3 years did not show any further episodes of reaction. Bwire and Kawuma have reported that both HIV-positive and IHV-negative patients showed similar responses to steroid therapy for the management of acute neuritis (4). Patients with HIV infection and erythema nodosum leprosum (ENL) type of reactions also have been reported by Olivares, et al. (13) and Almeida, et al. (1). None of our patients developed ENL reaction.
Patient no. 1 has been on dapsone for 2 years and is now on World Health Organization (WHO)-recommended MB multidrug therapy (WHO/MB-MDT) for 1 ½ years. He developed a tuberculous pleural effusion 7 months ago and is doing well on antituberculosis treatment. He has been followed up for 3 ½ years after the initial diagnosis of HD and HIV infection.
Patient no. 2 had many atypicalities. His skin biopsy was consistent with borderline lepromatous (BL) leprosy but his bacterial index (BI) was only 0.25+. He defaulted after treatment for 3 months with rifampin and dapsone. A year later follow up showed no clinical or bacteriological evidence of HD. However, a cutaneous nerve biopsy done at that time showed BL HD with clusters of AFB, suggesting active leprosy. Although he had had inadequate treatment, follow up 5 years later showed no clinical or bacteriological evidence of HD, and this defies adequate explanation. Although his CD4 count was significantly low, he had no signs of clinical AIDS (The Table). Thus, there was no correlation between his immunosuppressed HIV status and the course of his HD.
Patient no. 3 completed 2 years of WHO/ MB-MDT and showed clinical and bacteriological remission. Follow up a year after stopping treatment showed no clinical or bacteriological activity of HD. His T lymphocyte cell count was normal (The Table).
Patient no. 4 developed fever, oropharyngeal candidiasis and tuberculous peritonitis 2 months after the diagnosis of HIV and HD. Since this patient died 2 months later, no comment can be made about the response to treatment or the course of HD. The patient did not have T-cell counts done.
Even though there are many reports of patients who have dual infection with HIV and HD, the largest number are reported from Uganda (8). However, these studies have neither observed the clinical progress of HD nor the response to treatment over a period of follow up. While the preponderance of data suggest that the interaction of these two diseases is virtually nil, Borgdorff, et al. (2) found that HIV-1 is a risk factor for the development of MB leprosy (odds ratio 4.6; CI = 1.3-13.2).
Patients nos. 1, 2, and 3 have been followed up for 3.5, 5, and 3 years, respectively, after the diagnosis of dual infection. During this period, they had neither worsening of their leprosy nor progression to clinical AIDS. A longer period of follow up is needed to see whether they will develop any reactivation or relapse of HD.
Thus, on the whole, HIV infection does not appear to influence an infection with Mycobacterium leprae.
Acknowledgment. We thank Dr. Sushil M. Chandi for reading the histology of the biopsy slides and Dr. George P. Babu for doing the ELISAs, Western blots, and T4 cell counts.
REFERENCES
1. ALMEIDA, A. M., ROSELINO, A. M. F. and Foss, N. T. Leprosy and HIV infection. Int. J. Lepr. 62(1994)133-134.
2. BORGDORFF, M. W., VAN DEN BROEK, J., CHUM, H. J., KLOKKE, A. H., GRAF, P., BARONGO, L. R. and NEWELL, J. N. HIV-1 infection as a risk factor for leprosy; a case-control study in Tanzania. Int. J. Lepr. 61(1993)556-562.
3. BWIRE, R. and KAWUMA, H. J. S. Leprosy, Kaposi's sarcoma and the acquired immune deficiency syndrome in two African patients. Trans. R. Soc. Trop. Med. Hyg. 87(1993)559.
4. BWIRE, R. and KAWUMA, H. J. S. Type I reactions in leprosy, neuritis and steroid therapy: the impact of human immunodeficiency virus. Trans. R. Soc. Trop. Med. Hyg. 88(1994)315-316.
5. CHACKO, S., JOHN, T. J., BABU, P. G., JACOB, M., KAUR, A. and MATHAI, D. Clinical profile of AIDS in India: a review of 61 cases. J. Assoc. Physicians India 43(1995)535-538.
6. DECOCK, K. M., SORO, B., COULIBALY, I. M. and LUCAS, S. B. Tuberculosis and HIV infection inn sub-Saharan Africa. JAMA 268(1992)1581-1587.
7. KAUR, A., BABU, P. G., JACOB, M., NARASIMMHAN, C., GANESH, A., SARASWATHI, N. K., MATHAI, D., PULIMOOD, B. M. and JOHN, T.J. Clinical and laboratory profile of AIDS in India. J. Acquir. Immune Delic. Syndr. 5(1992)883-889.
8. KAWUMA, H. J. S., BWIRE, R. and ADATU-ENGWAU, F. Leprosy and infection with human immunodeficiency virus in Uganda; a case-control study. Int. J. Lepr. 62(1994)521-526.
9. KENNEDY, C, CHIN A LIEN, R. A. M., STOLZ, E., VAN JOOST, T. and NAAFS, B. Leprosy and human immunodeficiency virus infection; a closer look at the lesions. Int. J. Dermatol. 20(1990)139-140.
10. LAMFERS, R. J. R, BASTIANS, A. H., MRAVUNAC, M. and RAMPAN, F. H. J. Leprosy in the acquired immunodeficiency syndrome. Ann. Intern. Med. 107(1987)111-112.
11. LEONARD, G., SANGARE, A., VERDIER, M., SASSOUGUESSEAU, E., PETIT, G., MILAN, J., M'BOUP, S., RAY, J.-L., DUMAS, J.-L., HUGON, J., N'GAPORO, I. and DENIS, F. Prevalence of HIV infection among patients with HD in African countries and Yemen. J. Acquir. Immune Delic. Syndr. 3(1990)1109-1113.
12. MEERAN, K. Prevalence of HIV infection among patients with leprosy and tuberculosis in rural Zambia. Br. Med. J. 298(1989)364-365.
13. OLIVARES, L. M., PIZZARIELLO, G. E. A., BENETUCCI, J. and FARINA. M.H. Lepromatous leprosy with HIV infection. Int. J. Lepr. 62(1994)295-296.
14. PONNIGHAUS, J. M., MWANJASI, L. J., FINE, P. E. M., SHAW, M., TURNER, A. C, OXBORROW, S. M., LUCAS, S.B., JENKINS, P.A., STERNE, J.A.C. and BLISS, L. Is HIV infection a risk factor for leprosy? Int. J. Lepr. 59(1991)221-227.
15. SEKAR, B., JAYASHEELA, M., CHATTOPADHYA, D., ANANDAN, D., RATHINAVEL, L., VASANTHI, B., SUBRAMANIAN, M. and RAO, P. S. Prevalence of HIV infection and high risk characteristics among leprosy patients of South India-a case control study. Int. J. Lepr. 62(1994)527-531.
16. SHIV RAJ, L., PATIL., S. A., GIRDHAR, A., SENGUPTA, U., DESIKAN, K. V. and SRINIVASAN, H. Antibodies to HIV-1 in sera of patients with mycobacterial infections. Int. J. Lepr. 56(1988)546-551.
17. VREEBURG, A. E. M. Clinical observations on leprosy patients with HIV-1 infection in Zambia. Lepr. Rev. 63(1992)134-140.
1. M. Jacob, M.N.A.M.S., Professor and Head, Department of Dermatology, Christian Medical College and Hospital, Vellore 632 004, Tamil Nadu, South India.
2. S. George, M.D., Dip.NB., Department of Dermatology, Christian Medical College and Hospital, Vellore 632 004, Tamil Nadu, South India.
3. S. Pulimood, MIX, Department of Dermatology, Christian Medical College and Hospital, Vellore 632 004, Tamil Nadu, South India.
4. N. Nathan, M.A., Department of Dermatology, Christian Medical College and Hospital, Vellore 632 004, Tamil Nadu, South India.
Received for publication on 12 March 1996.
Accepted for publication in revised form on 28 May 1996.