- Volume 64 , Number 4
- Page: 455–7
Dormancy, drug resistance or dependency; some thoughts to ponder
To the Editor:
This study, using the mouse foot pad method, was aimed at investigating Mycobacterium leprae persistors in the skin and nerves of leprosy patients and their sensitivity to drugs after a fixed duration of the World Health Organization-recommended multidrug treatment (WHO/MDT). Certain observations were intriguing and persuasive.
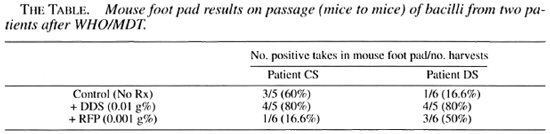
Secondary resistance to dapsone (DDS) (0.01 g%) and rifampin (0.001 g%) were recorded in two of the multibacillary cases treated and released from WHO/MDT. It was noted, however, that in both patients the percentages of takes (in second passage, mice to mice) were higher in the presence of DDS. Both were 80% as compared to untreated mice of 60% and 16.6%, respectively (The Table), and the average fold increases/foot pad of M. leprae were 10 times more in DDS-treated mice, suggesting that these organisms grew better in the presence of 0.01 g% DDS given by oral feeding.
A reconfirmation of the results was sought in these two patients. A second skin biopsy was obtained from each patient 3 years after release from treatment (RFT). The bacterial index (BI) of these biopsies were: Patient CS had a BI of 5+ and a morphological index (MI) of 1%; patient DS had a BI of 4.5+ and a MI of 1%.
Inocula were appropriately diluted to give 1 x 104/0.03 ml and injected into the foot pads of normal Swiss white mice, and a direct test for sensitivity to the same concentration of DDS (0.01 g%) and a higher concentration of rifampin (0.03 g%) was carried out.
Contrary to our expectations, both inocula showed no recordable count in the foot pads of mice at 6, 7, 8 and 12 months. However, significant counts were obtained at 16 months in both of the control groups of mice. The percentage take in patient CS was 80% (4/5); in patient DS, 67% (4/6). Only inocula from patient CS showed growth in the foot pads of drug-treated mice (percentage take with DDS 0.01 g% = 25% (1/4); with rifampin 0.03 g% = 33% (2/6), thus confirming resistance to both DDS and rifampin using highest concentrations.
Since there were no mice left, further harvests and confirmation of growth could not be carried out. Nevertheless, these cumulative data have raised several questions.
Results from the first part of the study indicate that there was a subpopulation of M. leprae that were not only refractory to DDS but grew better in the presence of DDS (? DDS dependence) and a doubtful rifampin resistance considering the concentration of rifampin used in this test was only 0.001 g%.
Three years after RFT, the second biopsies obtained from the same patients, in spite of showing a good BI and 1% MI, failed to show a normal growth pattern. Since the harvests were carried out at regular intervals beginning from month 6, the chances of missing any growth did not arise. We were, hence, inclined to assume that these "dormant persistor" bacteria either continued to remain dormant in the foot pads of mice for a prolonged period or they had an unusually long generation time, thus showing a delay in growth?
Another argument would be that if a significant subpopulation of M. leprae were DDS dependent, 3 long years of starvation would have further reduced their metabolic activity or viability. This argument derives some support from the results obtained in the second part of the study, i.e., growth in the foot pads was at a lower level in patient DS who had shown a higher degree of DDS dependency in the first inocula.
It should be mentioned that DDS dependency was also indicated in yet another inoculum tested in our laboratory that was derived from an untreated lepromatous case (to be published). Another independent in vitro study records unperturbed and abetter growth in the presence of rifampin of a M. tuberculosis strain that was derived from a tuberculosis patient showing clinical resistance (Mistry, N.F., personal communication).
There is documented evidence of the increased growth rate of atypical mycobacteria and of M. malmoense (S-253/86) in the presence of isoniazid in Lowenstein-Jensen media (2,3). The concept of physiological or adoptive resistance development to DDS was proposed by Chatterjee (1). Observations made in the present study indicate the possibility of an interplay between dormancy, drug resistance and dependency. It also suggests an alternative approach to tackling the problem rather than justifying a case for prolongation of MDT An up-to-date clinical history of these patients given below does not contradict the above thoughts.
Case 1. Patient DS was registered as a LL case in 1979. The patient remained absent from 1980 until June 1988, and was put on WHO/MDT from July 1988-June 1990. Histopathology studies of skin and nerve in April 1990 showed regressing lepromatous leprosy. The patient underwent repeated episodes of erythema nodosum leprosum reaction which were managed with steroids. Because the patient developed steroid dependency, the reaction was controlled with thalidomide. A mean BI when treatment was withdrawn was 4.3 and negativity was attained during a 5-year surveillance period. Skin and nerve biopsies 2 months after stopping treatment revealed growth in the mouse foot pad.
Case 2. Patient CS was diagnosed as LL with pulmonary tuberculosis (mean BI = 5.2) in January 1980 and incompletely treated with antituberculosis treatment (isoniazid + PAS 4- streptomycin and prothionamide) because the patient absented himself for 8 years from treatment after registry. When reported in 1988, the mean BI was 4.0 and the patient was put on WHO/MDT for 2 years from March 1988 to March 1990, when his mean BI was reported to be 3+. Histopathology of skin and nerve at this stage showed regressing borderline lepromatous leprosy. The BI was found to be negative in 1994. Periodical clinical examination of the patient did not show any evidence of clinical activity or any signs that indicated any need for chemotherapy.
- V.P. Shetty, Ph.D.
Senior Research Officer
- N.F. Mistry, Ph.D.
Senior Research Officer
- M.W. Uplekar, M.D.
Medical Officer
- N.H. Antia, F.R.C.S., F.A.C.S (Hon.)
Director and Trustee
The Foundation for Medical Research
84-A R.G. Thanani Marg
Worli, Bombay 400 018 India
- V.V. Pai, M.B.B.S., D.D.V.
Medical Officer
- R. Ganapati, M.B.B.S., D.D.V.
Director
Bombay Leprosy Project
Vidnyan Bhavan
11 V.N. Purav Marg
Sion-Chanabhatti
Bombay 400 002, India
REFERENCES
1. CHATERJEE, B. R. Drug resistance and multi-drug therapy in leprosy. Lepr. India 54(1983)402-411.
2. HAFFNER, S. E. and JHELM U. Increased growth ofMycobacterium malmoense in vitro in the presence of isoniazid. Eur. J. Clin. Microhiol. Infect. Dis. 10(1991)787-788.
3. MIORNER, H. and OLSSON, B. Improved isolationof mycobacteria other than M. tuberculosis on ison-azid containing Lowenstein-Jensen medium. Eur. J.Clin. Microhiol. Infect. Dis. 7(1988)47-49.
Reprint requests to Dr. Shetty.