- Volume 60 , Number 4
- Page: 641–3
Erythema nodosum leprosum: a possible cause of oral destruction in leprosy
ABSTRACT
Apart f rom vague statements and speculative remarks, the role of ENL in the oral cavity has not been considered in the recent English language literature. A case of oral ENL is reported, and we postulate that ENL plays a prominent role in the intra-oral destruction noted in leprosy. Information gathered f rom the literature and f rom our own experience with a series of 37 leprosy patients with oral lesions support this postulation.In an effort to increase the utility of the Journal in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
This short paper reports a case of destructive ulceration of the hard and soft palate coinciding with a peak of severity of erythema nodosum leprosum (ENL) in a patient who was observed over a period of more than a decade. It is suggested that this kind of immunologically mediated destructive ulceration may be the cause of the frequently reported deformities of the palate and uvula in leprosy.
Oral lesions in lepromatous leprosy have been reported much more frequently1-7 than oral lesions in reactional tuberculoid and borderline leprosy.8, 9
In a review of the English language literature since 1950, no reports of oral ENL came to light, although Reichart,10 did report both "ulcerating painful leproma" and various degrees of destruction of the soft palate and uvula in patients who had ENL or a history thereof, but he only hinted at a possible relationship.
CASE REPORT
A 46-year-old black male presented at Westfort Hospital in 1976 with a hoarse voice and extensive ulceration of the extremities. On the basis of the clinical features and the extensive lepromatous infiltration of the skin, especially of the face, ears and legs, he was classified as true lepromatous leprosy. Acid-fast bacterial indexes from skin smears were done over a period of 11 years (The Table).
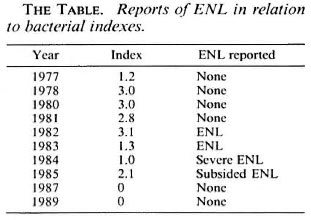
The patient started developing episodes of ENL in 1982, and was treated with hydrocortisone followed by tapering doses of prednisolone. In 1983 he had multiple skin lesions of ENL as well as a polyarthritis, which was treated symptomatically with ibuprofen and crepe bandages. The severity of the ENL peaked during 1984, and then gradually subsided under treatment.
During the 1984 phase of severe ENL, the patient was examined at the dental clinic. He had skin lesions of ENL all over his body (Fig. 1). The oral aperture was constricted with whitish angular cheilitis, and with diffuse white patches on the tongue, buccal mucosa and palate, diagnosed as a candidal infection. He was partially edentulous, the few remaining teeth being in extremely poor condition. On the mid-posterior hard palate there was an ulcer 1.5 × 1.5 cm in size, with a smaller ulcer at the right of soft and hard palate (Fig. 2). The main ulcer was about 3-4-mm deep with an intense red central area surrounded by a yellowish necrotic halo. The soft palate was deformed by scarring and the uvula was destroyed (Fig. 3).

Fig 1. ENL lesions on the arm.
Fig 2. ENL lesions of the palate.
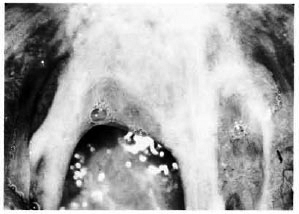
Fig 3. Destructive changes of the soft palate and uvula
DISCUSSION
Since the skin lesions are so characteristic, the term ENL is often used synonymously with the term "type 2 lepra reaction," which is an example of a type 3 Gell and Coombs hypersensitivity reaction. In addition to the ENL skin lesions, type 2 lepra reaction includes fever, malaise, tissue pain (e.g., muscle, nerve and periosteum), and polyarthritis."
ENL ulceration rather than primary lepromatous ulceration may be the major cause of the destruction, perforation4, 12 and deformation of the palate and uvula. There are several arguments in favor of this postulation. ENL is characterized by an acute vasculitis in which tissue destruction is common. Reichart's cases10,13 with palatal scarring and/or ulceration had active ENL or a history thereof, and in a scries of 37 leprosy patients, 3 of the 4 with destruction of the uvula and soft palate had active ENL; the fourth had a history of ENL.14
The bone destruction seen in the premaxilla (facies leprosa) may also be aggravated by an ENL reaction,15 and in support of this contention, Moller-Christensen16 observed increased destruction of other bones coinciding with severe ENL reactions.
If ENL does indeed play an important role in the destruction of oral tissues, then more elfective management of this condition17 may reduce these unfortunate sequelae.
- Anton Scheepers, B.Ch.D.
Registrar
Department of MaxillofaciaI and Oral Surgery
- Johan Lemmer, B.D.S., H.Dip.Dent.
Professor & Head
Department of Oral Medicine and Periodontology
University of Witwatersrand
Johannesburg, Republic of South Africa
1. Bucci, F., Mesa, M., Schwartz, R. A., McNeil G. and Lambert. C. Oral lesions in lepromatous leprosy. J. Oral Pathol. Med. 42(1987)4-6.
2. Epker, B. N. and Via, W. F. Oral and perioral manifestations of leprosv. Oral Surg. Oral Med. Oral Pathol. 28(1969)342-347.
3. Fitch, H. B. and Ailing. C. C. Leprosy, oral manifestations. J. Periodont. 33(1962)40-44.
4. Girdhar, B. K. and Desikan, K. V. A clinical study of the mouth in untreated lepromatous patients. Lepr. Rev. 50(1979)25-35.
5. Lighterman, I., Watanabe, Y. and Hidaka, T. Leprosy of the oral cavity and adnexa. Oral Surg. Oral Med. Oral Pathol. 15(1962)1178-1194.
6. Mukherjce, A., Girdhar, B. K. and Desikan, K. V. Histopathology of tongue lesions in leprosy. Lepr. Rev. 50(1979)37-43.
7. Reichart, P. and Mai, C. Pathological changes of the soft palate in lepromatous leprosy; an evaluation of 10 patients. Oral Surg. Oral Med. Oral Pathol. 38(1974)889-904.
8. Alfieri, N., Fleury, R. N., Opromolla, D. V. A, Ura, S. and de Campos, I. Oral lesions in borderline and reactional tuberculoid leprosy. Oral Surg. Oral Med. Oral Pathol. 55(1983)52-57.
9. Mishra, B., Girdhar, A., Husain, S., Malaviya, G. N. and Girdhar. B. K. A borderline lesion of the palate: a case report. Lepr. Rev. 59(1988)71-74.
10. Reichart, P. Facial and oral manifestations in leprosy. Oral Surg. Oral Med. Oral Pathol. 41(1976)385-399.
11. Jopling, W. H. Handbook o f Leprosy. 3rd edn. London: Heinemann, 1986, pp. 70-74.
12. Prejean, B. M. Oral aspects of leprosy. J. Am. Dent. Assoc. 17(1930)1030-1038.
13. Reichart. P., Ananatasan. T. and Re/nik, G. Gingiva and periodontium in lepromatous leprosy. J. Periodontol. 47(1976)455-460.
14. Scheepers, A. Oral manifestations of leprosy; clinico-pathological study. Dissertation, Johannesburg, University of Witwatersrand, 1992.
15. Rendall, J. R. and McDougall, A. C. Reddening of the upper central incisor associated with periapical granuloma in lepromatous leprosy. Br. J. Oral Surg. 13(1976)271-277.
16. Moller-Christensen. V. Bone Changes in Leprosy. Copenhagen: Munksgaard, 1961, pp. 14-15.
17. Shannon, E. J., Ejigu, M., Haile-Mariam, H. S., Berhan, T. Y. and Tadesse. G. Thalidomide's effectiveness in erythema nodosum leprosum is associated with a decrease in CD4 + cells in the peripheral blood. Lepr. Rev. 63(1992)5-10.
Reprint requests to Dr. Anton Scheepers, P.O. Box 140, 2050 WITS, Republic of South Africa.