- Volume 60 , Number 4
- Page: 657–8
Chromoblastomycosis masquerading as tuberculoid leprosy
To the Editor:
It is not uncommon for the skin lesions of leprosy to be mistaken for other skin diseases but only rarely does the reverse occur. There are occasional reports of diseases such as histiocytic lymphoma, pachydermoperiostosis, Melkersson-Rosenthal syndrome, amniotic band syndrome, and lymphocytic infiltration of the skin being misdiagnosed as leprosy (1-5).
A 21 -year-old male developed an asymptomatic, well-circumscribed, slightly erythematous, dry, flat, hypoesthetic, hypoalgesic, oval plaque of 3 × 4 cm on the lumbar region (Fig. 1). There was no thickening of the cutaneous or peripheral nerves. The routine laboratory tests on blood and urine were normal. Blood VDRL and Mantoux tests were negative. Slit-skin smears from the earlobes and from the plaque did not show any acid-fast bacilli. Histopathological study of the biopsy specimen taken from the edge of the plaque revealed mild atrophy of the epidermis and a granulomatous infiltration in the dermis consisting of many "tubercles," some eroding the basal-cell layer of the epidermis. There were also a few Langhans'-type giant cells (Fig. 2). A clinico-histopathological diagnosis of tuberculoid leprosy was made, and he was treated with dapsone 100 mg daily and rifampin 600 mg once a month for 6 months. Since there was no therapeutic response even at the end of 6 months and there was peripheral extension of the lesion, a skin biopsy was repeated. Histopathology this time revealed tuberculoid granuloma in the dermis and numerous dark brown, thick-walled, rounded spores (sclerotic bodies) inside the Langhans' giant cells (Fig. 3), suggesting a diagnosis of chromoblastomycosis. There was no associated epidermal hyperplasia or neutrophilic abscesses in the epidermis or dermis. Culture of the biopsy specimen in Sabouraud's agar yielded growth which was identified to be Cladosporiion carrioni. He was later treated by surgical excision of the lesion followed by skin grafting.
Fig. 1. Well-defined, dry, flat plaque of 4 × 3 cm on the lumbar area.
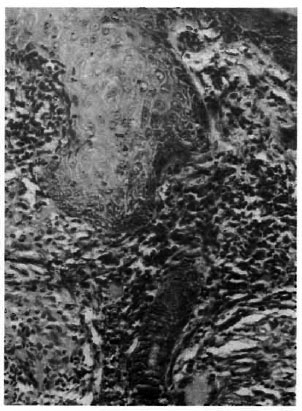
Fig. 2. Histology (H&E × 100) revealed tuberculoid granuloma in the dermis. The granuloma eroded the basal-cell layer of the epidermis.
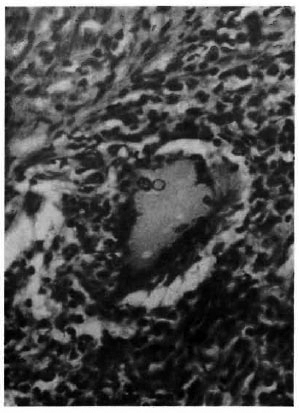
Fig. 3. Note two "sclerotic cells" within a Langhans' giant cell (H&E × 400).
Cutaneous chromoblastomycosis, being a verrucous lesion, usually docs not come under the differential diagnoses of leprosy. The well-defined, dry, hypoesthetic plaque in our patient simulated a tuberculoid leprosy lesion. However, the lack of therapeutic response to antileprosy drugs prompted us to repeat the biopsy and histopathological study which revealed "sclerotic cells," suggesting that the previous leprosy diagnosis was wrong.
This report emphasizes the need for considering chromoblastomycosis also in the differential diagnoses of tuberculoid leprosy and for a thorough search for "sclerotic cells" in all sections of biopsy specimens from skin lesions suspected to be tuberculoid leprosy, especially in areas where chromoblastomycosis is endemic. A tuberculoid granuloma in the dermis is only a tissue reaction to different ctiologic agents that include bacteria, viruses, fungi, parasites, and foreign bodies.
- K. Pavithran, M.D., D.V.D.
Associate Professor
Department of Skin and VD
Medical College Hospital
Kotlayam 686008, India
REFERENCES
1. BALACHANDRAN, C., SRINIVAS, C. R., SlNG, K. K. and VENUGOPAL, N. Histiocytic lymphoma simulating lepromatous leprosy-a case report. Indian J. Lepr. 59(1987)332-333.
2. JOPLING, W. H. Pachydermoperiostosis and leprosy. Lepr. Rev. 61(1990)402-404.
3. PAVITHRAN, K. Amniotic bank syndrome. Indian J. Lepr. 58(1986)291-294.
4. PAVITHRAN, K. Melkersson-Rosenthal syndrome masquerading as tuberculoid leprosy. Indian J. Lepr. 59(1987)27-29.
5. SING, K., DAWAR, R. and RAMLSH, V. Lymphocytic infiltration of skin of Jessner-Kanof masquerading as borderline leprosy. Indian J. Lepr. 57( 1985)804-806.