- Volume 63 , Number 4
- Page: 535–8
Prevalence rates of leprosy in Cambodia; results of a sample survey
ABSTRACT
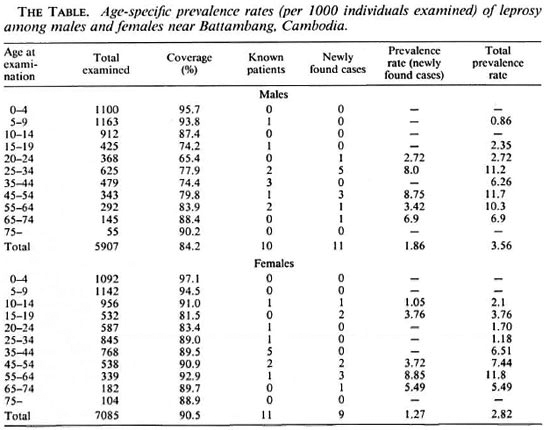
A total population survey was carried out in early 1994 in 13 villages around Battambang (northwest Cambodia). Coverage was 87.5% (12,992 out of 14,842). Among the 12,922 household members examined 21 known patients and 20 new patients were found. Five of the 21 known and none of the newly found patients had disabilities. Among males total prevalence rates (known and newly found patients combined) appear to rise up to the age of 25 to 34, after which rates remain roughly stable until they start to decline in the 65 to 74-year age group. Among females prevalence rates reach a plateau in the 35 to 44-year age group.RÉSUMÉ
Une enquête sur une population totale a été réalisée au début de 1994 dans 13 villages aux alentours de Battambang (Nord-Ouest du Cambodge). Parmi les 12 922 habitants examinés, on a trouvé 21 patients connus et 20 nouveaux patients. Cinq des 21 malades connus et aucun des malades nouvellement découverts avaient des incapacités. Parmi les hommes, les taux de prévalence totaux (combinant les malades connus et ceux nouvellement détectés) semblent augmenter jusqu'à l'âge de 25 à 34 ans, après quoi les taux restent grossièrement stables jusqu'à ce qu'ils commencent à descendre dans le groupe d'âge de 65 à 74 ans. Parmi les femmes, les taux de prevalence atteignent un plateau dans le groupe d'âge de 35 à 44 ans.RESUMEN
A principios de 1994 se hizo un estudio sobre la prevalencia de la lepra en 13 comunidades alrededor de Battambang, al noroeste de Cambodia. La cobertura fue del 87.5% (12, 992 de 14, 842 habitantes). Entre los 12, 992 convivientes examinados, se encontraron 21 pacientes conocidos y 20 casos nuevos. Cinco de los 21 casos conocidos y ninguno de los 20 casos nuevos tuvieron algún tipo de lesión incapacitante. Entre los hombres, la tasa de prevalencia total (casos conocidos y casos nuevos combinados) pareció aumentar hasta la edad de 25-34 años, después permaneció estable hasta que empezaré a decaer en el grupo de 65-74 años. Entre las mujeres, la tasa de prevalencia alcanzó una meseta en el grupo de 35-44 años de edad.A sample survey was carried out in 13 villages in two different districts in Battambang Province in northwestern Cambodia in order to assess the extent of the leprosy problem. Leprosy control services were established in the area in the late 1980s. Insofar as all casefinding was through self reporting, there was little knowledge about the true prevalence of leprosy. Prevalence surveys carried out in other countries have shown various ratios of known to newly found leprosy patients. In a survey in Tanzania of 15,029 people about 55% of the 116 patients found were not known to the health services (9). A mass screening in eastern Turkey, during which 15,848 people were examined, resulted in the detection of 18 new patients in addition to the 35 already known patients (7). When 1323 people were examined for leprosy in western Ethiopia, 7 new patients were discovered in addition to the 16 known ones (3).
An additional reason for carrying out the work was to investigate the feasibility of doing surveys in a country with an almost totally destroyed infrastructure due to civil wars (1). The survey was also meant to serve as a basis for future incidence studies.
METHODOLOGY
Because of the ongoing civil war and the widespread use of personnel mines in Battambang Province, it was not feasible to examine the population of a random sample of villages drawn from all villages in the province. Therefore, 13 villages were selected on the basis of being typical rural Cambodian communities and because they were, at the time of the survey, not touched by the war. Seven villages were situated along the Sangker River some 15 km to 20 km away from Battambang, and a large proportion of the inhabitants were fishermen. The other six villages were scattered along the main road to Phnom Penh (about 15 km southeast of Battambang). Most of these inhabitants were subsistence farmers growing rice. Examinations were carried out in February and March of 1994 after the rice harvest. The purpose of the survey was explained to the population in an effort to gain knowledge about the prevalence of common skin diseases in rural areas. Because of widespread somatization of leprosy patients in Cambodia, the word leprosy was studiously avoided during the study.
Lists of people were obtained from the village leaders. The village leaders also were responsible for informing people about the purpose of the survey and the examination schedule. Examination points were schools, temples, and other central places. Male and female individuals were examined in screened-off cabins by male and female paramedical staff, respectively. Examinations were complete with the exception of the pelvis. All individuals with any skin lesion were referred to a medical officer (DL).
Leprosy was diagnosed on the basis of clinical signs (typical skin lesion with definite anesthesia and/or definitely enlarged nerves). In addition skin smears and skin biopsies were taken from most suspects. Biopsies (6mm punch specimens) were examined in Homburg (JMP). If there was no evidence of leprosy histopathologically the diagnosis leprosy was discarded.
Provincial and district records of known patients were screened for residency in the sample survey area, and these patients were subsequently identified during the field work even if there were no residual signs of leprosy.
Age was taken from the village registers and confirmed at the time of examination. If no one from a household listed by the village headman came for examination, inquiries were made via the neighbors. Households who had left more than 3 months ago were assumed to have left the area permanently, even if neighbors thought they might come back.
Data were entered and analyzed using the EPI-INFO computer program.
RESULTS
A total of 2903 households were found in the 13 villages; 12,992 members could be examined, 1850 were absent. The overall coverage reached 84.2% among males and 90.5% among females. Among the 20-24 year-old males only two thirds could be examined. Of the present heads of households 685 out of 2410 (28%) were females; among absent heads of households 56 out of 493 (11.4%) were females.
The age and sex distribution of people examined is shown in The Table. Females (7085) outnumber males (5907), this being only partly explained by the larger number of males not examined. Noteworthy is the sharp drop in numbers per 5-year age group above the age of 14.
The average age of known patients was 37 years, the average age of newly found patients was 41.9 years. Of the known patients 11 were females; of the newly found patients 9 were females. Five of the 21 known patients had disabilities (grade 2) (10); none of the newly found ones had any disability. For 15 of the 20 newly found patients biopsy results were available (confirming the clinical diagnosis leprosy). In five patients biopsies could not be taken because of: lesions on the face (2), age (1), refusal (2). All newly found patients were members of different households; only one was found in a household with a known patient. The 21 known patients were found in 18 different households. Only one of the newly found patients had multibacillary (MB) leprosy, borderline lepromatous/lepromatous (J3L/LL) with the highest bacterial index (BI) of 5. The classification of the known patients proved difficult due to the lack of reliable original records.
Age-specific prevalence rates are also shown in The Table. Among males, total prevalence rates (known and newly found patients combined) appear to rise up to the ages of 25-34 after which rates remain roughly stable until they start to decline in the 65-74-year age group. There was no leprosy below the age of 5. Among females, prevalence rates appear to reach a plateau in the 35-44-year age group. No leprosy patient below the age of 10 was found.
DISCUSSION
There might be some doubt concerning the diagnosis of leprosy among known patients without disabilities. However, this is bound to be the case in any prevalence survey. Among 3631 registered patients in Norway (who were never hospitalized) Irgens calculated a predictive value of the diagnosis leprosy of 94.3% (4). A similar rate among the 21 known patients in the sample survey would mean that 1 or 2 did not have leprosy. The effect on the overall prevalence rate would be small. Among new patients strict diagnostic criteria were applied, and we consider it unlikely that a false-positive diagnosis was made. On the other hand, it is possible that an early case was overlooked among those examined. Again, the effect on prevalence rates would be small.
There is a remarkable drop in the number of people above the age of 14 living in the 13 villages included in our sample survey. The most likely reason would seem to be that during the reign of the Khmer Rouge (1975 until 1978) older individuals fell victim to war, mass killings, starvation and epidemics (1). Correspondingly, a surplus of females is particularly noticeable among older age groups.
The coverage achieved (84.2% among males and 90.5% among females) compares favorably with that of other surveys. During a survey in Trinidad only 73.5% of the people could be examined completely (8). In a leprosy-endemic area in Turkey coverage was between 68.5 and 76.2% (7). In Greater Bombay 81.2% of 39,345 enumerated people could be examined during surveys in slums (6).
The average age of newly found patients (41.9 years) was higher than that of known patients (37 years). This finding is in contrast with findings in Tanzania, where newly found patients were younger than known ones (9). We presume that around Battambang younger patients found it easier to report to the leprosy services in the town of Battambang than did older people.
Overall prevalence rates are slightly higher for males than for females. We do not think that this excess is due to an ascertainment bias because examinations of females were as complete as examinations of males (carried out by examiners of the same gender). On the other hand, the difference is small and may be due to chance. Total prevalence rates in this survey can be compared to rates called "cumulative rates" found during a total population survey in Karonga District, northern Malawi (5). Rates rise to around 10 per 1000 individuals examined in the older age groups, which is considerably lower than in Karonga District/northern Malawi where cumulative rates rose to around 40 per 1000 individuals examined in the 45-59-year age group (5). In slum areas in Greater Bombay the overall prevalence rate was 11.9 per 1000 (6). Even ignoring likely differences in the age structures of the populations this is, again, considerably higher than the overall rates for males and females found around Battambang (3.56 and 2.82, respectively). In Tanzania the overall prevalence rate was 7.7 per 1000 (9).
An interesting feature of the prevalence rates around Battambang is that peaks are reached in older age groups than is usual (2). This may be chance (due to the small numbers included in the survey). However, an alternative explanation could well be that we are faced with the end of an epidemic in this part of the world. Low rates among children also were found during school surveys in Battambang town where 5 new cases could be found among 4449 school children examined (DL, unpublished observations).
Obviously, the survey around Battambang cannot be called representative for the whole of Cambodia. In some provinces prevalence rates will be higher; in others, lower. Nevertheless our results suggest that there are only twice the number of patients in Cambodia than the number on treatment-not 4½ times the number as suggested in a recent WHO publication (11).
Two of the villages included in the sample survey were burnt down by Khmer Rouge platoons shortly after the survey. So it seems unlikely that the area will be suitable for incidence studies in the foreseeable future.
Acknowledgment. Financial assistance for the sample survey was received from the Western Pacific Regional Office of WHO. JMP was given a travel grant from The Cochrane Fund to visit the Maltescr Hilfs dienst Leprosy Control Project in Cambodia. OA Dr.med. H. P. Baum helped in examining the biopsies. We thank the Ministry of Health of the Kingdom of Cambodia for their permission to publish this paper.
REFERENCES
1. Chandler, D. P. The Tragedy of Cambodian History . New Haven and London: Yale University Press, 1991.
2. Fine, P. E. M. Leprosy: the epidemiology of a slow bacterium. Epidemiol Rev. 4(1982)161-188.
3. Gundersen, S. G. Leprosy and tuberculosis in the Blue Nile Valley of western Ethiopia. Lepr. Rev. 58(1987)129-140.
4. Irgens, L. M. Leprosy in Norway. Lepr. Rev. 51s(1980)1-130.
5. Ponnighaus, J. M., Fine, P. E. M., Maine, N., Bliss, L. Kalambo, M. and Ponnighaus I. The Lepra Evaluation Project (LEP), an epidemiological study of leprosy in northern Malawi. II: Prevalence rates. Lepr. Rev. 59(1988)97-112.
6. Revankar, C. R., Dudhalkar, B., Raju, G. D. and Ganapati, R. Leprosy surveys in urban slums possibilities for epidemiological investigations. Lepr. Rev. 53(1982)99-104.
7. Saylan T and Aytekin AH. Mass screening in leprosy-endemic areas of Turkey: preliminary report. Lepr. Rev. 57(1986)243-249.
8. Suite, M., Edinborough, N. B. Lewis M. and Tollefson J. A survey to determine the prevalence of leprosy in a community in east Trinidad. Lepr. Rev. 65(1994)122-129.
9. Van Praag, E. and Mwankemwa, S. A. A prevalence survey on leprosy and the possible role of village 10-cell leaders in control in Muheza District, Tanzania. Lepr. Rev. 53(1982)27-34.
10. WHO Expert Committee on Leprosy. Sixth report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
11. World Health Organization. Progress towards eliminating leprosy as a public health problem. Wkly. Epidemiol. Rec. 69(1994)145-151.
1. Dr.med., Malteser Hilsdicnst, Leprosy Control Project, Battambang, Cambodia.
2. Dr.med, D.T.M.&FL, D.T.P.H., Universitäts-Hautklinik, 66421 Homburg, Saar, Germany.
Reprint requests to Dr. Ponnighaus.
Received for publication on 7 July 1995;
Accepted for publication on 5 September 1995.