- Volume 63 , Number 4
- Page: 559–66
Eliminating leprosy as a public health problem; why the optimism is justified
Editorial opinions expressed are those of the writers.
Following the widespread implementation, since 1982, of the World Health Organization (WHO)-recommended multidrug therapy (WHO-MDT) and the adoption by WHO in 1991 of the goal of elimination of leprosy as a public health problem, there have been considerable interest and debate on the progress being made toward leprosy elimination, and some questions have been raised on the optimism generated. It has therefore become necessary to explain the changes taking place in the leprosy scene in recent years and to address the issues raised on the goal of eliminating leprosy as a public health problem.
The experience with MDT over the last 10 to 15 years has shown that the treatment is highly effective in curing the disease, acceptable to a wide range of patients, and has only minimal side effects. Based on a review of several thousands of patients over 9 years of follow up, relapse rates following MDT have been found to be only around 0.1% per year, an extraordinarily good performance for chemotherapy against an infectious agent.1 It is possible to estimate that, by changing over from dapsone monotherapy to MDT, about half a million relapses have been prevented over the last 10-15 years. So far no cases have been reported of resistance to MDT. The benefits of MDT are very well appreciated by the patients, as shown by the high treatment compliance rates (over 90%) in most leprosy programs, and the fact that a very high proportion of multibacillary (MB) patients agree to take clofazimine (a constituent of MDT) in spite of discoloration of the skin, which is reversible once the treatment is stopped.
A great advantage of MDT, apart from its effectiveness, applicability and patient acceptance, is its robustness in that it is effective even under less than optimal conditions. As long as the drugs are taken in combination, MDT provides a degree of benefit even to the irregularly treated patients. It is relevant to mention here that leprosy treatment is largely confined to the public health services, and limiting the availability of MDT drugs to the public sector in most countries has prevented the haphazard use of the drugs either as monotherapy or through inappropriate combinations of drugs in the private sector and, thus, has prevented the emergence of multidrug resistance.
In terms of progress made in conquering leprosy over the past 10-15 years, MDT has played the central role and it continues to be the center of the strategy for the future.
Since 1985, globally, leprosy has been reduced from around an estimated 10-12 million cases to 1.8 million cases, a-reduction of over 80%. In terms of registered cases the reduction is over 75%, i.e., from 5.4 million to 1.3 million cases. The number of cases cured through MDT since 1985 is nearly 6.7 million with another 1 million patients currently undergoing treatment with MDT2. For details see Tables 1 and 2.
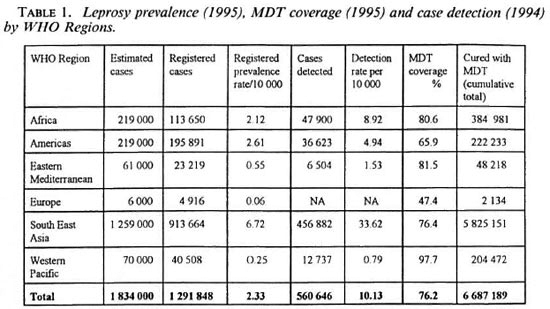
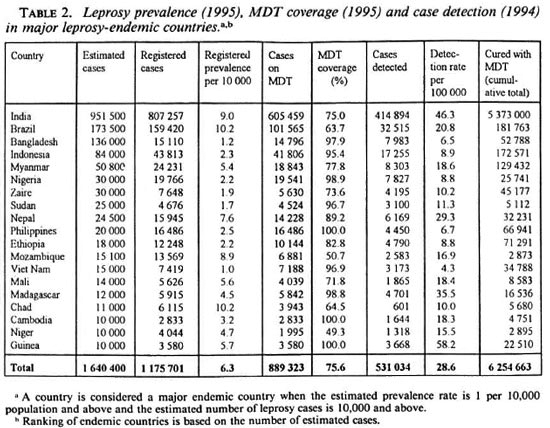
Table 1, which provides information by WHO Region, shows that currently the heaviest burden of leprosy is in the South- East Asian Region followed by the African and American Regions which have lower prevalences. The situation in the Eastern Mediterranean and Western Pacific Regions is even more favorable. As far as Europe is concerned, leprosy is a relatively uncommon disease with limited foci; however, information on leprosy in the Region is generally incomplete and outdated.
The uneven distribution of the disease among countries is a marked feature of leprosy as shown in Table 2. Only 19 countries contribute 89% of the estimated global leprosy prevalence of which just five countries contribute 76%. India alone accounts for 52% of the global burden. This pattern is even more markedly shown in the distribution of registered cases and new cases detected. In terms of MDT implementation, the current coverage of registered cases with MDT is 76%, with variation among regions. Of the 6.7 million patients cured through MDT so far, about 5.8 million or 87% belong to the South-East Asian Region.
Global progress over the last 10 years indicates that the estimated and registered prevalences have declined by about 84% and 76% respectively, although there has been no appreciable change in case detection. The projections for the year 2000 call for prevalence reduction by a further 83% and case detection by about 50%. These reductions, if attained, would result in the cumulative figure for patients cured through MDT to exceed 10 million by the year 2000.
Even though these figures are highly impressive, all of this would not have been possible without the impetus provided by MDT in reinvigorating leprosy programs and in reinforcing political and professional commitment everywhere. The introduction of MDT has resulted in improved performance of leprosy control programs by way of organized review of leprosy case registers and excluding cases not needing treatment, increased casefinding and mobilization of community support. The encouraging results seen also have increased everywhere the motivation and enthusiasm of health workers dealing with leprosy. Even the donor agencies, particularly donor nongovernmental organizations (NGOs) whose focus was more on the care of the individual patient, found the public health approach through MDT to be a very attractive social goal. This resulted in their increased support to disease control activities and support to national ministries of health.
Elimination of leprosy as a public health problem. The phenomenal results obtained in the first 5 to 10 years of implementing MDT and the prospects for making further major gains through concerted action led the 1991 World Health Assembly to adopt the goal of elimination of leprosy as a public health problem by the year 2000 through its resolution WHA44.9. This defined elimination as attaining a level of prevalence below one case per 10,000 population. The resolution declared WHO's commitment to global elimination and urged countries to increase their political commitment to this goal. By establishing a target for the year 2000, the World Health Assembly drew attention to the effectiveness of MDT, the need for leprosy-endemic countries and donor agencies to stop regarding leprosy as a permanent problem and to grasp the opportunity to conquer the disease. The commitment to eliminate leprosy was indeed a giant step in dealing with this centuries-old scourge.
The elimination goal received the enthusiastic endorsement from national ministries of health of leprosy-endemic countries as well as of the WHO Regional Committees which led to increased political commitment. The commitment to the elimination goal was further reiterated in the first International Conference on the Elimination of Leprosy held in Hanoi on 1-4 July 1994.3 The Conference also approved the global strategy and global plan of action for elimination. The countries and the WHO Regions themselves also had developed their own strategies and plans of action, in concert with the global strategy and plan, and have been able to set their own intermediate targets and mechanisms for monitoring. That the World Health Assembly resolution had a major impact can be seen from the fact that leprosy has been reduced by about 60% since 1991, when the resolution was adopted, and that practically most major leprosy-endemic countries have increased their priority for leprosy. An important resource constraint being faced by the countries for procurement of MDT drugs was resolved at the Hanoi Conference through a commitment of a major donor agency (Sasakawa Foundation) which pledged US$ 10 million per year to WHO until the year 2000 for free supplies of MDT drugs to the countries in need.
Questions on elimination of leprosy. The WHO-inspired goal of eliminating leprosy as a public health problem, in spite of attracting an overwhelmingly positive response from most people concerned with the plight of leprosy patients, also has generated questions among some as to its necessity, feasibility and long-term sustainability apart from some difficulties in understanding what is elimination. Although many of these have been answered earlier;4 they call for further clarification.
Firstly, there is the question of why leprosy should be chosen for elimination as a public health problem in the context of a large number of health problems facing the developing countries. The answer to this relates to the tremendous physical and social burden caused by leprosy which cannot be fully expressed just in terms of statistics on prevalence or incidence. The disease, even if it does not kill, is capable of causing permanent and progressive physical disability and consequent psychological damage. Apart from this, in light of the severe social stigma attached to leprosy in many societies, when an individual gets leprosy it causes tremendous social problems, not only to the individual but also to the family, and sometimes even to the community.
The second and more important reason why we need to eliminate leprosy is the unique opportunity we now have to achieve this goal. This window of opportunity is the result of a confluence of four highly favorable factors involving: a) an epidemiological opportunity, i.e., that in many parts of the world leprosy is already on the retreat in terms of its secular trend; b) a technological opportunity, i.e., that MDT is highly effective in curing the disease; c) a political opportunity, i.e., that there is good national commitment in all major leprosy-endemic countries and d) a resource opportunity, i.e., that a number of donor agencies and NGOs are currently keen to support efforts toward MDT implementation and leprosy elimination. Such a favorable situation may not last long-be it in terms of the epidemiological trend, continued effectiveness of MDT, political commitment or the interest of the donor agencies.
Thirdly, the very purpose of putting together a concerted time-bound effort is to ensure that the heavy investment during a limited period would result in sustained long-term gains. The intensive activities and resource investment of the 1990s involving MDT is expected to reduce the disease burden to such low levels that after the year 2000 a considerable part of the resources employed for leprosy until that year can then be released for other purposes.
In addition, leprosy as a disease offers other unique epidemiological opportunities. The very uneven distribution of the disease among and within countries makes it possible to identify and target priority areas and, thus, focus resources and activities more effectively. Further, the current prevalence burden in leprosy is a result of incident cases accumulating over several years and even decades, with the current new cases contributing to only a small proportion of the prevalence pool. This means that through MDT a very high proportion of the disease burden can be reduced even if the new cases continue to occur in small numbers. In this connection it should be recognized that the very long incubation period in leprosy makes incidence reduction in the short term very difficult since a high proportion of new cases currently occurring are probably those who had acquired their infection several years earlier and before MDT had been introduced. Thus MDT implementation today, although capable of interrupting transmission, may not result in a dramatic reduction in incidence for many years to come due to its very long incubation period. Yet another advantage with leprosy is that it has no other significant reservoir of infection other than the human case, with rifampin capable of rendering cases practically noninfectious even with a single dose, the total infective pool can be drastically reduced even in the face of some patients not taking their treatment regularly.
Lastly, the phrase "elimination of leprosy as a public health problem" is sometimes confused with the term "eradication." Eradication envisages total and complete interruption of transmission resulting in zero disease and also the total disappearance of the organism involved. Elimination as a public health problem is a somewhat less ambitious goal, in which the disease prevalence is reduced to very low levels even if complete interruption of transmission is not possible. In leprosy the elimination goal is clearly defined as attaining a level of prevalence below one case per 10,000 population. To some extent this cut-off point is arbitrary, although there are indications that when such very low levels are attained the potential for transmission will be extremely low and thus the possibility of the disease dying out slowly are quite high. Again, the reference to the public health problem is mainly to address the reservoir of infection in terms of the pool of active cases and its potential for transmission. Therefore when we mention the disease burden in the public health context we are referring to only active cases, and it should not be confused with the accumulated burden of cured individuals even if they are left with residual disability. With regard to the deadline of the year 2000 to achieve the goal, the end of the millennium is a convenient and visible goalpost and, although somewhat arbitrary, it is also considered reasonably feasible. Further, it should be emphasized that although the World Health Assembly refers to global elimination, the intention is that the goal should also be attained at the national level and for larger countries also at the first subnational level.
A question often raised is why the elimination goal is set in terms of prevalence and not incidence, which is likely to be a much more sensitive indicator. The main difficulty is that incidence in leprosy is not easy to measure through routine reporting systems which generate information only on case detection. Leprosy case detection has a very low correlation with incidence in view of the prolonged delay between onset of the disease and detection. Recent information indicates that the delay in detection is more than 3 years in a large majority of instances. Secondly, due to the long incubation period, current incidence reflects transmission that had occurred several years earlier and, therefore, does not indicate the effectiveness of current antileprosy activity.
From the foregoing discussion it is clear that eliminating leprosy as a public health problem has clear definitions, and its limitations vis-a-vis eradication should be fully recognized. Currently we have no tools to completely interrupt transmission, neither do we have dependable tools to measure transmission of infection. Therefore, the dependence on measuring disease burden is through prevalence figures. It is ironic that today one is able to foresee the end of leprosy even before the epidemiology of the disease is fully understood.
Challenges and prospects for the future. The attainment of the goal of elimination of leprosy means reaching a prevalence level of under 300,000 cases globally by the year 2000 from the current figure of 1.8 million estimated cases, and the cumulative figure for cases cured through MDT to exceed 10 million by the year 2000 from the current figure of 6.7 million. The progress so far has been very good because it was possible for the well-organized programs and well-developed health services to reach the relatively easy areas and to implement MDT effectively. However, in the future we will be facing the problem of the more difficult areas, populations and services, and this calls for even more intensive efforts and innovative approaches keeping in view the timebound nature of the goal. It is important to maintain and further intensify the political and professional commitment and not slacken our efforts in light of the good progress achieved so far.
The difficult-to-access areas and populations will be an important part of the remaining problem, and routine approaches are unlikely to deal with them effectively. In these instances, cost per case treated will be quite high since special input not usually needed elsewhere will be needed here. The WHO Leprosy Programme has recently developed a special mechanism that would enable short-term special projects to be set up in countries to reach patients difficult to reach, even if it means utilizing nonconventional channels for treatment. A geographical information system (GIS) is also being set up to identify highly endemic pockets of leprosy that will need special attention.
Even in reasonably well-organized programs it is clear that delayed detection of new cases is an important factor in the accumulation of cases, resulting not only in damage to the individual patient but also in maintaining the infection pool in the community longer than necessary. Special initiatives are being employed through support from the WHO Leprosy Programme to flush out the undetected and, therefore, untreated cases from the community so that the disease burden can be reduced more rapidly. The special initiatives include shortterm campaign approaches reinforcing the existing approaches. While the short-term costs of campaigns are high, in the longer term they may turn out to be cost-effective.
In the context of the decreasing disease burden, the relevance of specialized vertical leprosy programs as well as the relevance of leprosy-specialized elements within the general health services will increasingly be questioned, particularly in terms of their cost-effectiveness. While vertical programs should be discouraged, the continuation of specialized leprosy elements in support of general health services should be looked at carefully so that in the process of integration the general health services have at least some support for supervision and referral. This is particularly important if the existing disease burden is still high in spite of significant decrease over the years. One way to address this problem would be to shift the leprosyspecialized elements to a higher level in order to cover a larger area and thus be costeffective. Alternatively, if the general health services at all levels are sufficiently strong it may be possible to train supervisory personnel supporting the general health services to undertake the specialized activities for leprosy. In any case, it is important to remember that the elimination goal should not be compromised in any way and that support elements in some form should continue until the goal is attained.
The occurrence of disability is the raison d' être for the concern about leprosy, and the need to deal with the disabled should not be underestimated. However, it is clear that the best way to address the problem is to prevent the occurrence of disabilities, and the best way to prevent disabilities is through early diagnosis and prompt treatment with MDT. This has already happened through widespread implementation of MDT and it is estimated that over the last 10-15 years MDT, through its direct and indirect contributions, has prevented over 1 million disabilities from occurring. Although early diagnosis and treatment can prevent disabilities, still a proportion of patients at the time of detection will be at risk of disability as a result of damage to the peripheral nerves and such patients will need special attention. MDT programs should incorporate simple, targeted activities to prevent disability among such "at risk" patients. In spite of this, some patients will have disabilities at the time of diagnosis and will need care to limit the disabilities, and those who become handicapped will need attention and care within their families and communities. The solution to the individual with residual disability after cure has to be found within the context of community-based rehabilitation (CBR). In this context it is also important to take maximum advantage of the existing internal coping mechanisms within the family and community. However, these rehabilitation issues should not be confused with the tasks relating to the elimination goal.
As we progress toward the elimination goal and look into the future it is possible to anticipate several changes, mostly for the better. MDT itself might undergo modifications with yet another set of new drugs more powerful and more easily applicable, which could make treatment simpler, shorter and fully supervisable. Further, it is possible to envisage operational refinement of the classification of leprosy which might take into account the very early minimal disease having a high tendency for spontaneous healing. This may have consequences for future treatment regimens. With increasing demonstration of the curability of leprosy, social attitudes toward leprosy patients may change for the better and social stigma against leprosy may slowly diminish. Leprosy is likely to be fully accepted within the mainstream of medicine and public health and become a part of the general health services. With specialized unipurpose leprosy expertise becoming less and less common, leprosy expertise is likely to be increasingly "owned" by other specialists such as dermatologists. Leprosy-specific NGOs and donor organizations are likely to broaden their base and maintain support for leprosy work in the broad context of support for general health care and slowly diversify. Leprosy research itself, particularly basic research, is likely to merge within the overall general mycobacterial research. Beyond the year 2000, the burden of those disabled due to leprosy will diminish further and they will probably be dealt with in ways similar to other disabled. All of these will be welcome developments in general except for those full-time leprosy workers who have spent their lifetime in leprosy and thus miss seeing leprosy as a special cause, an exclusive effort and an exceptional rallying point in support of the most neglected.
Post-elimination issues. Even as we are promoting integration of leprosy such efforts should not be misconstrued as forgetting leprosy completely after the year 2000. As indicated earlier, small numbers of cases will continue to occur for several years beyond the year 2000, resulting from infections acquired in the pre-MDT period. Even small numbers of leprosy-endemic pockets might survive since these are the places to which leprosy would like to retreat in the face of the MDT onslaught. All these call for constant vigilance and surveillance to monitor and to deal with any resurgence of the disease. However, the historic experiences with leprosy in the past and the epidemiology of disease, as we understand it now, does not suggest that leprosy in terms of its possible resurgence will behave in ways similar to other diseases, such as malaria. All the same, the elimination of leprosy through specific interventions like MDT, particularly in poverty-stricken situations, should be monitored carefully and special monitoring mechanisms should be developed for this purpose. It is conceivable that current research into the immune response to Mycobacterium leprae may yield simple tools by the early 2000s with which to monitor the infection in the community in a more sensitive manner. Lastly, it is hoped that the tremendous knowledge gained in the last three to four decades on M. leprae and other aspects of leprosy will be expanded further, including through the currently ongoing construction of the genome of M. leprae , so that any unforeseen problem faced with leprosy in the 21st century could be addressed effectively.
Conclusions. Eliminating leprosy as a public health problem is certainly a highly desirable goal, it is attainable notwithstanding some challenging tasks ahead. When such a goal is reached and sustained it will be another major triumph for organized human effort in a world struggling to achieve health for all. WHO has enabled the development and dissemination of the technical means to achieve this and has provided the leadership toward concerted action to achieve the goal. However, it is the leprosyendemic countries and their health workers, together with those who supported them with the necessary means, that should take full credit for what has been achieved so far and what is expected to be achieved in the next 5 years. There is no doubt that the optimism that exists now is justified; however, the momentum gained so far needs to be maintained and further accelerated. This tunity to sec the end of leprosy. is not the time to relax or become complacent. We cannot afford to miss this opportunity to see the end of leprosy.
- S. K. Noordeen.
Director.
Action Programme for the Elimination of Leprosy
World Health Organization
1211 Geneva 27, Switzerland
1. Risk of relapse in leprosy. Geneva, World Health Organization, 1994 (unpublished document WHO/ CTD/LEP/94.1).
2. WHO. Weekly Epidemiological Record, No. 25, 1995, pp. 177-182; No. 26, 1995, pp. 185-188.
3. WHO. Report of the International Conference on the Elimination of Leprosy, 1994 (unpublished document WHO/CTD/LEP/94.5).
4. Elimination of leprosy-questions and answers, WHO, 1993 (unpublished document WHO/CTD/LEP/ 93.7).