- Volume 63 , Number 4
- Page: 567–9
An unusual presentation of facial palsy in leprosy; a case report
In an effort to increase the utility of the JOURNAL in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial points. Letters to the Editor pointing out other viewpoints are welcome.
In leprosy the most commonly involved nerve in the face is the zygomatic branch of the seventh cranial nerve causing paralysis of the orbicularis oculi muscle. There is difficulty in bringing the eyelids close together, resulting in lagophthalmos. Symmetrical involvement of these nerves on both sides is also seen rarely. Occasionally, the whole facial nerve on one side may be affected in the bony canal causing Bell's palsy. However, it is very uncommon to find paralysis confined to only the forehead muscles and upper eyelid on one side. It is even more uncommon to meet with a patient presenting with paralysis of forehead muscles and upper eyelid on one side and the lower facial muscles on the opposite side. One such patient is presented here.
A 65-year-old male patient presented to our eye clinic in December 1994 with poor visual acuity in both eyes of gradual onset, and epiphora in the right eye of approximately 1-year duration. The duration of the patient's leprosy was uncertain but he had received 5 to 6 years of dapsone monotherapy, and was then lost to follow up. He was re-traced in 1992, 2 years prior to this presentation. He had lagophthalmos of the right eye and his skin smears were negative. He was diagnosed then as borderline tuberculoid (BT) leprosy with lagophthalmos of the right eye and was again given dapsone monotherapy.
On examination, there were three ill-defined, hypopigmented and partially anesthetic skin patches, one on the forehead above the right eye and one each on both upper arms. There was another small, welldefined patch on the left upper arm.
His ulnar nerves and lateral popliteal (common peroneal) nerves on both sides and the left posterior tibial nerve were thickened. Glove-and-stocking type anesthesia was present on all four limbs. There was a trophic ulcer on the right sole and shortening of the left hallux associated with the scar of a healed ulcer. Skin smears taken from routine sites, including the skin patch on the right upper arm revealed a bacterial index (BI) of 1.75+.
An ophthalmic examination of his right eye revealed a visual acuity of counting fingers not improved with a pin hole. There was loss of normal forehead skin creases and lagophthalmos due to upper lid laxity. The latter was accentuated by forced lid closure, when the upper lid margin tended to buckle as the discrepancy in the upper and lower lid activity became more marked. There was 3- to 4-mm of lagophthalmos on gentle closure, not reduced by forced closure due to the loss of apposition to the globe of the upper lid (Figs. 1 and 2). Bell's phenomenon was absent and his cornea showed fine punctate staining with fluorescein over the inferior one third, but was otherwise clear with normal sensation. The anterior chamber, iris and pupil were normal and there was a dense cataract. Intraocular pressure was 13 mm of mercury. The lower nasolacrimal punctum was well-positioned but stenosed. Other facial muscles on his right side functioned normally.
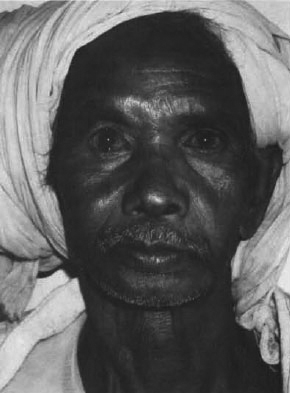
Fig. 1. Patient with both eyes open. Note the lossof normal forehead creases on right side, flattening ofnasolabial fold, and drooping of the angle of the mouthon left side.
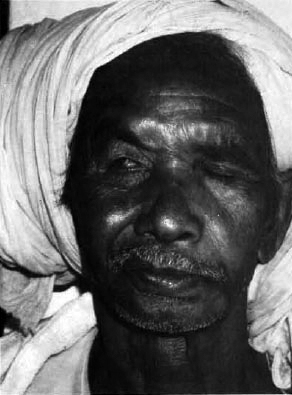
Fig. 2. Patient attempting to close both eyes. Notelagophthalmos due to upper lid laxity on right side,flattening of nasolabial fold, and drooping of the mouthon left side.
Examination of his left eye revealed a visual acuity of 6/60 not improved with a pin hole. Lid closure was normal, with normal orbicularis oculi function. An anterior segment examination was unremarkable, and there was lens opacity to a slightly lesser degree than in the right eye. Intra-ocular pressure was low, 5.3 mm of mercury, despite no other clinical evidence of intra-ocular involvement by Mycobacterium leprae . Corneal sensation was normal.
There was flattening of the nasolabial fold and drooping of the angle of the mouth on the left side (Figs. 1 and 2). Facial sensation was normal except in the region of the patch described above.
The patient was clinically and bacteriologically classified as borderline lepromatous (BL) leprosy with weakness of selective fibers of the zygomatic branch of the right seventh cranial nerve of at least 2 years' duration and the buccal and mandibular branches of the left seventh cranial nerve of unknown duration.
DISCUSSION
The zygomatic branch to the facial nerve as it passes superficial to the zygoma provides a favorable milieu for M. leprae which is known to proliferate in Schwann cells and to have a preference for cool sites closer to the skin. The pattern of muscle weakness observed in this patient demonstrates the selective destruction of nerve bundles within a peripheral nerve especially in BT-BL leprosy. The branching and rearranging of nerve bundles into varying numbers of fascicles along its course can also result in sparing of the motor function in the presence damage to up to one third of a nerve trunk. Thus selective fibers of the muscle supplied may show weakness or paralysis while other fibers function normally. The nerve lesion may remain stationary or progress until eventually all the nerve fascicles are destroyed.1
Progressive nerve damage has been known to occur in the absence of active disease in treated patients. Job, et al . examined an ulnar nerve biopsy from such a patient and postulated that the proliferation of fibrous tissue observed may be a reactive phenomenon to the continued presence of fragments of the bacilli and their products. An increase of intraneural collagen causing ischemia could result in Schwann cell atrophy and subsequent demyelination and necrosis.2
Owing to the irregularity of this patient's attendance for treatment and follow up, it had been difficult to chart the clinical course of his disease accurately. However, the above mechanism of nerve damage would be consistent with the clinical findings, occuring after 5 to 6 years of dapsone therapy.
Further, this patient (after his second visit) progressed from BT leprosy to BL leprosy in a period of 2 years while undergoing dapsone monotherapy. Either the patient failed to take the drug regularly or the organisms in his lesions were resistant to dapsone. This, again, emphasizes the importance of administering multidrug therapy (MDT), if feasible, to all paucibacillary patients who have completed a course of monotherapy and have been discharged as cured. This patient came from a remote tribal area in eastern Bihar and MDT was introduced in that region only recently. In such remote areas staff motivation to stay well informed and keep good records is found to be very difficult, and staff turnover tends to be very high, compounding the problem. An all out effort to establish MDT treatment programs in these remote field areas, although demanding, is imperative. Therefore, it is true to state that "despite the strongly declining prevalence of leprosy, leprosy-related disabilities will, for decades to come, continue to exist as an important problem. Effective leprosy services will continue to be needed into the 21st century".3
- Dr. Kirsteen Thompson, F.R.C.S.
Ophthalmologist
The Leprosy Mission India
Purulia Leprosy Home and Hospital
P.O. Box 9
Purulia 723101, West Bengal, India
1. Job, C. K. Nerve damage in leprosy. Int. J. Lepr. 57(1989)532-539.
2. Job, C. K., Victor, D. B. I. and Chacko, C. J. G. Progressive nerve lesion in a disease-arrested leprosy patient-an electron microscopic study. Int. J. Lepr. 45(1977)255-260.
3. Feenstra, P. Will there be a need for leprosy control services in the 21st century? (Editorial) Lepr. Rev. 65(1994)297-299.