- Volume 63 , Number 4
- Page: 529–34
Pupil cycle time in leprosy patients without clinically apparent ocular pathology
ABSTRACT
The pupil cycle time (PCT) was estimated in 384 leprosy patients whose eyes looked normal on clinical examination and in an equal number of healthy controls. A statistically significant increase in PCT (p < 0.05) was noticed in leprosy patients, and corroborates the view that the ocular autonomic system may be affected without any visible clinical pathology in the eye. The clinical value and application of this finding is uncertain since the difference is only a few milliseconds. Young females with leprosy showed a conspicuous lengthening of PCT for which no plausible explanation is offered. There was a general trend for the PCT to increase as the spectrum of disease moved toward the lepromatous pole and a significantly higher PCT (p < 0.01) was found among multibacillary patients compared to paucibacillary patients. Patients who had had erythema nodosum leprosum (ENL) reactions showed a higher PCT than did those who had not had ENL. Patients who had had reversal reactions showed a decrease in PCT, which may be a statistical oddity in this hospital-based study. Patients whose duration of the disease was over 10 years showed a higher PCT, while smear positivity of a patient did not alter the PCT significantly.RÉSUMÉ
Le temps du cycle pupillairc (TCP) a cié estimé chez 384 malades de la lèpre dont les yeux paraissaient normaux à l'examen clinique, et chez un nombre équivalent de témoins en bonne santé. Une augmentation statistiquement significative du TCP (p < 0.05) a été notée chez les malades de la lèpre, et corrobore l'idée que le système autonomique oculaire poutrait être affecté sans qu'il n'y ait de pathologie cliniquement visible de l'oeil. La valeur clinique et l'application de celte découverte est incertaine puisque la didërence n'est que de quelques millisecondes. Les jeunes femmes lépreuses montraient un ralentissement évident du TCP, pour lequel aucune explication évidente n'est offerte. If y avait une tendance générale à ce que le TCP augmente lorsque le spectre de la maladie allait vers le pôle lépromateux et un TCP signficativement plus élevé (p < 0.01) fut trouvé parmi les patients multibacillaires comparé aux patients paucibacillaires. Les patients qui avaient eu des réactions d'érythème noueux lépreux (ENL) montraient un TCP plus élevé que ceux qui n'avaient pas eu d'ENL. Les patients qui avaient eu des réactions reverses montraient une diminution du PCT, ce qui pourrait être une bizarrerie statistique dans cette étude hospitalière. Les malades dont la maladie avait duré plus de 10 ans ont montré un TCP plus élevé, alors que la positivité des frottis d'un patient ne modifiait pas significativement le TCP.RESUMEN
Se estimó el tiempo cíclico de la pupila (PCT) en 340 individuos sanos y en un número similar de pacientes con lepra cuyos ojos se miraban clínicamente normales. Se notó un incremento significativo del PCT en los pacientes con lepra (p < 0.05) y esto corroboróque el sistema autónomo ocular puede afectarse sin manifestar ninguna alteración clínica del ojo. El valor clínico y la aplicación de este hallazgo son inciertos ya que la diferencia fue de sólo unos millscgundos. Las mujeres jóvenes con lepra mostraron un alargamiento conspicuo de sus PCTs pero no se pudo ofrecer una explicación racional a este hallazgo. Se observó una tendencia general de incremento del PCT conforme el espectro de la enfermedad se acercó al extremo lepromatoso; los pacientes lepromatosos multibacilares tuvieron PCTs significativamente mayores (p < 0.01) que los pacientes paucibacilares. Los pacientes que habían tenido eritema nodoso leproso (ENL) mostraron PCTs mayores que los pacientes sin ENL. Los pacientes que habían presentado reacciones reversas mostraron cierta disminución en sus PCTs, aunque esto bien pudo representar sólo la probabilidad estadística. Los pacientes con una enfermedad mayor de 10 años mostraron los PCTs más altos, mientras que la positividad bacilar de los pacientes no afectó significativamente sus valores de PCT.An estimated 250,000 people in the world are blind due to leprosy (l2). This figure could swell to distressing proportions if those patients with gross visual handicap, but not falling within the conventional definition of blindness, are included in this category. For a disease in which blindness is generally preventable these figures are undesirable. More effective strategies to combat blindness and ocular morbidity are needed. These would, to a large extent, depend upon the detection of early ocular involvement and the exposition of clinically discernible risk factors that could reasonably forecast the occurrence of ocular inflammatory episodes which often are the cause of blindness in leprosy.
Beading of corneal nerves (13), low intraocular pressures (3), postural changes in intraocular pressures (6), denervation hypersensitivity of the pupil (17) and pupil cycle time (4) have all been studied by investigators as possible parameters that would enable early recognition of ocular involvement in leprosy.
Pupil cycle time (PCT) is the time in milliseconds that the pupil takes to constrict and dilate once, when stimulated with a slit beam of light. PCT has been studied in several diseases, including diabetes (9), HIV infection (7) and leprosy (4). The prolonged PCT observed in leprosy patients has been suggested to be a sign of early ocular involvement. Since the intake of patients in our leprosy study (4) was small and many demonstrated clinically observable ocular manifestations that, by themselves, could prolong PCT, we measured PCT in leprosy patients whose eyes looked normal on clinical examination and herein present our findings.
METHODS AND PATIENTS
Unselected, consecutive leprosy patients (384) attending the outpatient clinic of the Schieffelin Leprosy Research and Training Center, Karigiri, India, from January 1992 to December 1994, conforming to certain criteria and whose visual acuity was 6/12 or better, were included in the study. An equal number of age-and sex-matched nonleprosy individuals were enrolled in the study as controls. All patients and controls had clinically normal eyes except for a few older patients with early senile cataract changes whose visual acuity did not drop to < 6/12. Persons with afferent pupillary defects, gross corneal opacities, evidence of past or present iridocyclitis, recent intake of autonomic function-altering drugs and known diabetics were excluded from the study. Patients with external eye infections and those with leprosy reactions were also excluded. However, patients who had had leprosy reactions were included in the study. The control group had similar socioeconomic backgrounds as that of the patients and consisted of relatives and friends of patients attending the hospital. Suspects and close contacts were excluded from the control group. After informed consent was obtained, demographic and leprosy data were recorded.
Leprosy data included: a) current type of leprosy categorized according to the Ridley and Jopling classification using bacteriological, clinical and histopathological parameters; b) approximate duration of the disease; c) current treatment status of the patients; d) duration and doses of dapsone monotherapy and multidrug therapy; e) highest bacterial index (BI) recorded at any one time during the course of the disease and f) the occurrence of type 1 and type 2 reactions.
PCT was measured in both eyes of all patients and controls using the method described by Miller and Thompson (11) with minor modifications. Subjects were placed in a dimly lit room and asked to fixate at a distant point. A horizontal, 1-mm wide slit beam of moderate intensity was focused through a Haag Strict slit lamp on the lower part of the iris with the microscope unit of the slit lamp perpendicular to the front of the eye and the illumination unit at about 30º from the microscopic unit. The beam of light was slowly elevated until it impinged on the pupil and initiated a cycle of constriction and dilatation. These oscillatory cycles were timed in runs of 30, 30, and 40 with a stopwatch and the time in milliseconds (ms) was calculated for one cycle. All patients and controls had their PCT estimated by the same investigator.
We were unable to record PCT for 7 leprosy patients (5 borderline lepromatous and 2 borderline tuberculoid patients) since we could not induce the pupillary oscillations despite increasing both the light intensity and width of the slit beam. Ten controls also were excluded from the study since they chose not to cooperate during the recording of PCT.
Means, standard deviations and proportions were computed and compared using t , normal and F tests. The analysis was done using the computer software package SPSS PC+.
RESULTS
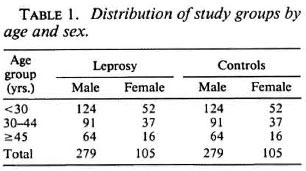
A total of 384 patients and an equal number of controls were studied. Their distribution in three broad age groups is given in Table 1. Ages of both patients and controls ranged from 8 to 75 years with an identical mean age of 33 years. The mean pupil cycle time (PCT) did not differ significantly between the right and the left eyes of patients or controls. The mean (S.D.) of PCT among leprosy patients was 735 (55) ms which was significantly (p < 0.05) higher than that of controls who had 726 (43) ms. The range of PCT in leprosy patients varied from 575 ms to 1004 ms; in the controls from 611 ms to 944 ms.
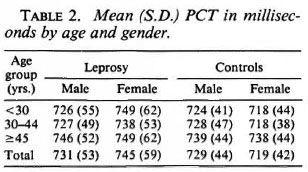
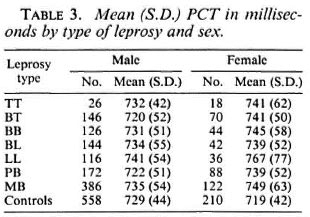
The mean (S.D.) of PCTs by age and gender is shown in Table 2. In the male and female control groups and in the male leprosy group there was a general trend for PCT to lengthen as age increased. However, a conspicuously higher PCT value was observed in females < 30 years in the leprosy group, which was significantly (p < 0.01) higher than other stratified groups of the same age. The mean (S.D.) of PCTs by type of leprosy and sex is given in Table 3. Except for the tuberculoid (TT) group of patients whose number was small, there is a general tendency for the PCT to increase as the type of leprosy moves toward the lepromatous pole. The mean (S.D.) PCTs of both males and females in the multibacillary (MB) group show a significantly (p < 0.01) higher value from that observed in the paucibacillary (PB) group.
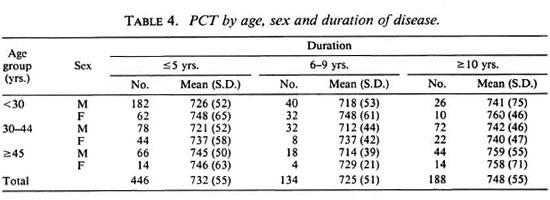
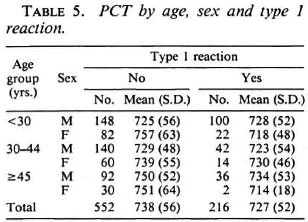
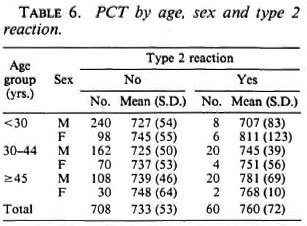
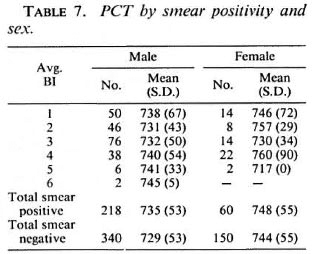
The mean (S.D.) PCTs by age, sex and duration of disease is given in Table 4. Higher values of PCTs are seen when the duration of disease exceeded 10 years. PCTs by age, sex and type 1 reaction given in Table 5 show the mean PCTs of patients who had had type 1 reaction to be significantly (p < 0.01) lower than those of patients who did not have the reaction duringtheir disease. Conversely, as seen from Table 6, the PCTs in patients who had had type 2 reactions shows significantly (p < 0.01) higher values from those patients whodid not. PCT by smear positivity and sex (Table 7) did not reveal any consistent pat-tern, and there was no significant differencebetween the mean PCTs of patients whowere positive for bacilli and those who werenegative for bacilli.
DISCUSSION
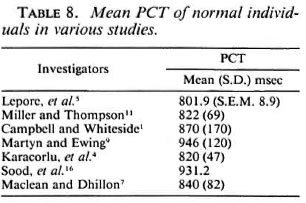
A noticeable feature in our study is that the mean PCT observed among our control subjects is one of the lowest recorded among those investigating PCT in recent times (Table 8). There is a wide range in the mean PCTs observed by various investigators with a low value of 801.9 ms and a high value of 946 ms. The methodology adopted by us varied to some extent from that of Miller and Thompson (11). We used a slit beam that had a width of 1 mm instead of ½ mm and had moderate intensity instead of low intensity because we found that this beam produced pupillary cycles of greater amplitude that were better observed. We also focused the beam from an angle since many of the patients found a coaxial beam disagreeable. Whether these minor modifications could have altered the PCT is uncertain since previous investigators (9, 11) have pointed out that both the intensity as well as the width of the slit beam does not alter the PCT significantly. Ethnic differences altering PCT seemed a possibility, but Sood and his coworkers (16), who had investigated PCT in 56 normal people of Indianorigin, reported an average PCT of 931.2ms. The number of their study subjects was not large and in the methodology used by them only 50 cycles were timed in each eye and no standard deviations were reportedfor any of the mean PCTs observed. We areunable to comment on the huge difference in values. Manor and coworkers (8), investigating PCT in normal subjects, reported mean (S.D.) PCTs of 739 (74) ms in a group aged 10-49 years and 872 (83) ms in an age group of 50-79 years. Since more than 340 of our controls (89%) were younger than 50 years, our mean (S.D.) value of 726 (43) ms is closer to the values obtained by them. However, the wide range of normal values of PCT obtained by various investigators highlights the importance of having a matched control group of normal individuals while investigating PCT in any particular disease in a group of patients.
The statistically significant difference observed between the mean PCTs of leprosy patients and healthy controls suggests that there could be some amount of impairment in the functioning of the ocular autonomic system in leprosy patients even though their eyes may not exhibit any noticeable clinical pathology. The finding that more leprosy patients have longer PCT than controls adds credence to this. This could be rated as a sign of early ocular involvement although its importance in a clinical context js uncertain. Whether a few milliseconds of difference in PCT would help differentiate a group of patients whose PCTs would indicate early ocular involvement is a moot point. Even if one were to differentiate such a group of patients there is nothing in the presently available literature to indicate that these patients would have more ocular complications compared to patients with shorter PCTs Carefully formulated studies involving long-term follow up of patients with and without prolonged PCTs are essential before extrapolating that prolongation of PCT be considered as an indicator of forthcoming ocular complications.
The young leprosy women in our study had a significantly higher PCT value than did the other groups. We investigated several variables that may have contributed to the elevated PCTs in this group. Socioeconomic status, type of leprosy, duration of the disease, smear positivity, and the leprosy reactions were looked into but did not show any significant correlation with PCT in this group. Previous studies in PCT have indicated that sex did not alter PCT (9, 11). The reason for the altered PCTs in young leprosy females in our study needs further investigation.
There is a general trend for PCT to increase as the spectrum of disease moves toward the lepromatous pole. A significant difference is noticed in the PCT of MB patients compared to PB patients. If affectation of the ocular autonomic system can be inferred from the prolonged PCTs observed in MB patients, it appears to be proportionate to the severity of the disease. Slowing of motor conduction velocity of peripheral nerves has been demonstrated among different types of leprosy in a number of studies (2, l0, 18). The increased PCT reflecting the ocular autonomic dysfunction is yet another corroborative feature of the slowing of nerve conduction in leprosy although its pathophysiology, especially when occurring in an apparently clinically normal organ, needs to be elucidated.
The increased PCTs of MB patients is also a reflection on the inclusion of a number of patients who had had erythema nodosum leprosum (ENL) within the MB group. It has been shown in this study that those patients who had ENL have a significantly higher PCT than those who did not. A decrease in nerve conduction velocities during reactions in leprosy has been well documented (14, l5). Paradoxically, our study shows a decrease in the PCT of patients who had had reversal reactions. This is difficult to explain and could be due to selection bias that is an inherent feature of any hospitalbased study. Being smear positive or having an increasing bacillary load did not alter PCT. This is in keeping with the fact that mere invasion of various ocular tissues by the bacilli does not produce any functional alteration unless the ocular tissues begin to react to the bacilli, producing inflammatory episodes.
Acknowledgment. The authors thank Miss Nisha Kurian who helped with the statistical analysis and Mr. P. Yovan and Mr. S. Babu for their help in some aspects of the study.
REFERENCES
1. CAMPBELL , F. W. and WHITESIDE , T. C. D. Induced pupillary oscillations. Br. J. Ophthalmol.34(1950)180-189.
2. HACKETT, E. R., SHIPLEY, D. E. and LIVENGOOD, R. Motor nerve conduction velocity studies of the ulnar nerve in patients with leprosy. Int. J. Lept. 36(1968)282-287.
3. HUSSEIN, N., CHIANG, T., EHSAN, Q. and HUSSEIN, R. Intraocular pressure decrease in household contacts of patients with Hansen's disease and endemic control subjects. Am. J. Ophthalmol. 114(1992)479-483.
4. KARACORLU, M. A., SUREL, Z., CAKINER, T., HANYALOGLU, E., SAYLAN, T. and MAT, C. Pupil cycle time and early autonomic involvement in ocular leprosy. 13r. J. Ophthalmol. 75(1991)45-48.
5. LEPORE, F. E., SANBORN, G. E. and SLEVIN, J. T. Pupillary dysfunction in myasthenia gravis. Ann. Neurol. 6(1979)29-33.
6. LEWALLEN, S., COURTRIGHT, P. and LEE, H.-S. Ocular autonomic dysfunction and intraocular pressure in leprosy. Br. J. Ophthalmol. 73(1989)946-949.
7. MACLEAN, H. and DHILLON, B. Pupil cycle time and human immunodeficiency virus (HIV) infection. Eye 7(1994)785-786.
8. MANOR, R. S., YASSUR, Y., SIEGAL, R. and BEN-SIRA, I. The pupil cycle time test: age variations in normal subjects. Br. J. Ophthalmol. 65(1981)750-753.
9. MARTYN, C. N. and EWING, D. J. Pupil cycle time: a simple way of measuring an autonomic reflex. J. Neurol. Neurosurg. Psych. 49(1986)771-774.
10. MCLEOD, J. G., HARGRAVE, J. C, WALSH, J. C, BOOTH, G. C, GYE, R. S. and BARRON, SISTER A. Nerve conduction studies in leprosy. Int. J. Lepr. 43(1975)21-31.
11. MILLER, S. D. and THOMPSON, H. S. Edge light pupil cycle time. Br. J. Ophthalmol. 62(1978)495-500.
12. NOORDEEN, S. K., LOPEZ-BRAVO, L. and SUNDERASAN, T. K. Estimated number of leprosy cases in the world. Indian J. Lepr. 64(1992)521-527.
13. PILLAT, A. Leprosy bacilli in the scrapings from the diseased cornea in a leper and comments on keratitis punctata supcrficialis leprosa. Arch. Ophthalmol. 3(1930)306-317.
14. SHESKJN, J., MAGORA, A. and SAGHER, F. Motor conduction velocity studies in patients with leprosy reaction treated with thalidomide and other drugs. Int. J. Lepr. 37(1969)359-364.
15. SOHI, A. S., KANDHARI, K. C. and SINGH, N. Motor nerve conduction studies in leprosy. Int. J. Dermatol. 10(1971)151-155.
16. SOOD, A. K., MITHAL, S., ELHENCE, A. and MAINI, A. Pupil cycle time. Indian J. Ophthalmol. 33(1985)41-43.
17. SWIFT, T. R. and BAUSCHARD, F. D. Pupillary reactions in lepromatous leprosy. Int. J. Lepr. 40(1972)142-148.
18. VERGHESE, M., ITHIMANI, K. V., SATYANARAYANAN, K. R., MATHAI, E. and BHAKTHAVIZIAM, C. A study of conduction velocity of the motor fibrea of ulnar and median nerves in leprosy. Int. J. Lepr. 38(1970)271-277.
1. M.B.B.S., M.S., D.O., Head, Department of Ophthalmology;
2. Dr.P.H., Director, Schieffelin Leprosy Research and Training Center, Karigiri, North Arcot District, Tamil Nadu 631 106, India.
Received for publication on 2 February 1995;
Accepted for publication on 6 July 1995.