- Volume 63 , Number 3
- Page: 417–21
Persistence of lepromatous granuloma in clinically cured cases of leprosy
ABSTRACT
Multibacillary (MB) leprosy patients are declared cured when they become bacteriologically negative and their lesions do not show any signs of clinical activity. Whether there is also a corresponding histological clearance of skin lesions is not known. The present study was carried out on the histopathology of the skin of 40 MB cases who were declared cured with multidrug (MDT). In 22 of them, small lepromatous,granulomas were seen to persist, although acid-fast bacilli were not found in them. The presence of these granulomas was not found to have any significant association with the duration of the disease, length of treatment, or the period of cessation of therapy.RÉSUMÉ
Les patients lépreux multibacillaires (MB) sont déclarés guéris quand ils deviennent bactériologiquement négatifs et que leurs lésions ne montrent aucun signe d'activité clinique. Y a-t-il également un nettoyage histologique correspondant des lésions cutanées, cela on ne le sait pas. L'étude présente concerne l'histopathologie cutanée de 40 patients MB déclarés guéris suite à une polychimiothérapie (PCT). Chez 22 d'entre eux, on a vu que des petits granulomes lépromateux persistaient, bien qu'on n'y ait pas trouvé de bacilles acido-résistants. On n'a pas trouvé que la présence de ces granulomes était associée de quelque manière que ce soit avec la durée de la maladie, la durée du taritement, ou la période d'arrêt du traitement.RESUMEN
Los pacientes con lepra multibacilar (MB) son declarados curados cuando llegan a ser bacteriológicamente negativos y sus lesiones no muestran ningún signo de actividad clínica. No se establece, sin embargo, si también ocurre una mejoría en las características histológicas de las lesiones de la piel. El presente estudio sobre la histopatología de la piel, se llevó a cabo en 40 casos MB que fueron declarados curados después de su tratamiento con poliquimioterapia. Se observó que en 22 de los casos persistieron pequeños granulomas lepromatosos, aunque no se encontraron bacilos ácido resistentes. No se encontró ninguna asociación significativa entre la presencia de granulomas y la duración de la enfermedad, la duración del tratamiento, o el período de suspensión de la terapia.After the introduction of standardized multidrug therapy (MDT) for leprosy in 1981, the cumulative MDT coverage has reached 89% of the registered cases (11). As of April 1994, it has been estimated that over 5.6 million leprosy patients have been "cured" through MDT (10). The World Health Organization (WHO) Study Group on the Chemotherapy of Leprosy (10) states that after the start of therapy, all lesions and bacilli should eventually clear. A relevant question, therefore, would be whether in these clinically "cured" cases there is histopathological clearance as well. The present study was carried out on the histopathology of the skin of multibacillary cases who were declared cured with MDT and were consistently bacteriologically negative for a long period of time.
MATERIALS AND METHODS
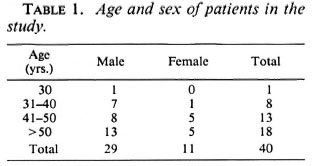
Study subjects. The study sample included 40 patients (29 males, 11 females), ranging from 30 to 65 years of age from Manohar Dham Dattapur, a leprosy hospital and rehabilitation center located in central India (Table 1). These patients were originally multibacillary (clincally classifed as lepromatous and with high bacterial indexes) cases who had been treated with MDT. Thirty-five of them had dapsone monotherapy prior to MDT. Following treatment, their lesions had clinically regressed, and they had become bacteriologically negative. Subsequently they were on continuous surveillance and were consistently bacteriologically negative.
Skin biopsies. At the time of obtaining the biopsy, the patients were thoroughly examined clinically to exclude any signs of disease activity. Slit-skin smear examination was carried out on them from the routine sites (i.e., ear lobes, forehead, chin and any other suspicious area) and their bacteriological negativity was confirmed. Skin biopsies were then taken from the back or from the sites of possible prior lesions (37 from the back and 3 from the posterior shoulder).
The biopsy specimens were fixed in 10% neutral formalin. Paraffin sections of 5- µ m thickness were stained with hematoxylin and eosin (H&E) as well as by the Fite-Faraco method.
RESULTS
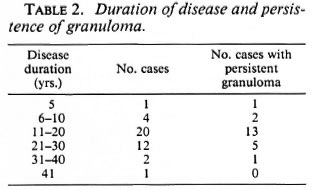
Twenty-two patients out of the 40 studied showed evidence of persistent granuloma in the skin after complete cure. The granulomas consisted of very small collections of vacuolated macrophages located in relation to skin appendages or nerve. There were varying numbers of round cells, mainly lymphocytes infiltrating the granuloma. Careful examination of multiple sections stained by the Fite-Faraco method did not reveal any acid-fast bacilli (AFB). The duration of the disease varied from 5 to 41 years, with a majority of the patients having had the disease for 11 to 30 years (Table 2). Dividing the patients into different groups based on duration of the disease, it was seen that nearly half the number of patients in each group had a recognizable granuloma. However, using the chi-squared test, there was no significant association between the duration of the disease and the presence of granulomas (p > 0.05).
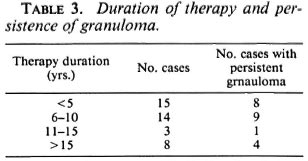
All of the patients included in this study had the full regimen of MDT prescribed for multibacillary cases. Thirty-five patients had varying periods of dapsone monotherapy prior to MDT. The total duration of therapy for all the patients ranged from 2 to 21 years.
Grouping the patients into different categories based on the duration of the therapy, it was again found that nearly half the patients in each category had recognizable, persistent granulomas (Table 3). Using the chi-squared test, there was no significant association between the duration of the therapy and persistence of granulomas (p > 0.05).
At the time of collection of skin biopsies, these patients, who had completed treatment and who were declared cured, had been clinically inactive and bacteriologically negative for varying periods of time (Table 4). Categorizing these patients into various groups based on the period between cessation of treatment and biopsy, it was found that granulomas persisted in a number of patients in each group. However, using the chi-squared test, there was no significant association between the period of time after cessation of treatment and persistence of granulomas (p > 0.05).

DISCUSSION
A chronic infective disease such as leprosy runs a long clinical course despite the effective antimicrobial therapy available. Clinical cure and clearance of bacilli are naturally prolonged. Cochrane (1) in 1947 stated that leprosy bacilli might lurk in the internal organs for a long time after the skin became bacteriologically negative. This was confirmed by Desikan and Job (2) who, at autopsy of treated, clinically inactive cases, found lepromatous leprosy lesions in the testes in 4 cases, in the liver in 2 cases, in the lymph node, adrenals and spleen in 1 case each. There are several reports of bacilli being present in nerves of long-treated cases (3,6,7). Viable bacilli have been demonstrated in the Dartos muscles in treated, bacteriologically negative cases (8). It was, therefore, of interest to make a histological examination of the skin of the treated, cured multibacillary leprosy patients to look for any persistence of granulomas or bacilli in deeper structures.
In the present study, a recognizable granuloma was found to persist for a number of years after clinical cure in 22 out of the 40 cases studied. While the granuloma was classically of the lepromatous type, being composed of vacuolated macrophages, careful examination after Fite-Faraco staining did not reveal any AFB. The occurrence of these granulomas did not depend on the duration of the disease or the duration of the therapy. Another important finding was that in five cases, the granulomas persisted for as long as 3 to 5 years after clinical cure and cessation of therapy.
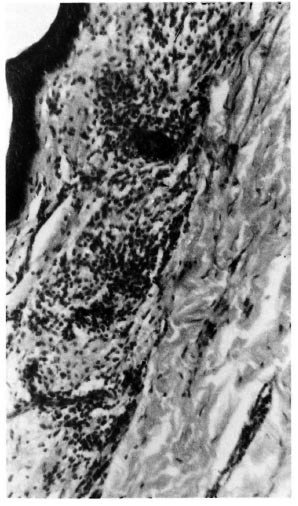
Fig . 1. Lepromatous granuloma in a case treated for 10 years (monotherapy and MDT); biopsy performed 2 years after cure. Patient had leprosy for 15years (H&E x 500).
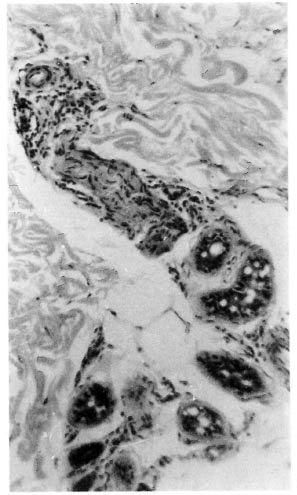
Fig. 2. Granuloma in a nerve in a lepromatousleprosy case treated for 5 years; biopsy performed 1year after cure. Patient had leprosy for 7 years (H&Ex 500).
The size of the granulomas in the skin was found to be extremely small. Hence, it would be reasonable to presume that they are regressing lesions. In a study of tuberculoid and borderline tuberculoid cases of leprosy before and after treatment, Lavania, et al. (5) found persistent granulomas in the treated cases but they were much smaller in size, thus indicating that the lesions were regressing. In another study of 30 treated and cured cases of the indeterminate type of leprosy by histopathological and immunohistological methods, Takahashi, et al. (9) found lesions persisting but regressing. It would make an interesting study to assess the regression of the lesions over a sufficiently long period of time.
The persistence of the granulomas would, however, indicate an ongoing antigenic stimulus causing replenishment of macrophages forming the granuloma. The danger of an ongoing antigenic stimulus is the risk of a progressive lesion. If this occurs, particularly in a nerve, there is a possibility of producing neuropathy even in the absence of viable bacilli, as suggested by Job, et al. (4) . Whether this is true or not would, in itself, be the basis of another study.
Acknowledgment. The authors are thankful to Dr. R. S. Sharma, Secretary, Manohardham Dattapur, for his close cooperation in conducting this study and to Mr. V. Kamalanathan for typing the manuscript.
REFERENCES
1. Cochrane, R. G. Pathology. In: A Practical Textbook of Leprosy. Cochrane, R. E., ed. London: Oxford University Press, 1947, p. 33.
2. Desikan , K. V. and Job, C. K. A review of post morterm findings in 37 cases of leprosy. Int. J. Lepr. 36(1968)36-44.
3. Haimanot, R. T., Mshana, R. N., McDougall, A. C. and Anderson, J. B. Sural nerve biopsy in leprosy patients after varying periods of treatment; histopathological and bacteriological findings on light microscopy. Int. J. Lepr. 52(1984)163-170.
4. Job , C. K., Victor, D. B. I. and Chacko, C. J. G. Progressive nerve lesion in a disease-arrested leprosy patient: an electronmicroscopic study. Int. J. Lepr. 45(1977)255-260.
5. Lavania, R. K., Girdhar , A., Girdhar , B. K. and Desikan K. V. Histological change in tuberculoid leprosy after fixed duration multidrug therapy for six months. Acta Leprol. (Denève) 7( 1990)169-174.
6. Palande, D. D. The ulnar nerve in the lower arm in dimorphous leprosy - some observations. Lepr. India 46(1974)1-6.
7. Pereira, J. H., Palande, D. D. and Gschmeissner , S. E. Mycobacteria in nerve trunks of long term treated leprosy patients. Lepr. Rev. 62( 1991 )134-142.
8. Ramu, G. and Desikan , K. V. A study of scrotal biopsy in subsided cases of lepromatous leprosy. Lepr. India 51(1979)341-347.
9. Takahashi, D., Andrade, H. F., Wakamatsu, A., Manini, M. and De Brito, T. Treated, cured indeterminate leprosy: a search for predictive histopathological and immunological parameters inskin biopsies taken from patients at admission andclinical discharge. Acta Leprol. (Geneve) 8(1982)95-102.
10. Who Study Group. Chemotherapy of leprosy. Geneva: World Health Organization, 1994, pp.1-5.
11. World Health Organization. Global strategy for the elimination of leprosy as a public health problem. WHO/CTD/LEP/94.2, 1994, p. 4.
1. M.D.,Leprosy Histopathology Centre, Mahatma Gandhi Institute of Medical Sciences, Scwagram 442102, Dist. Wardha, Maharashtra State, India.
2. M.D., Leprosy Histopathology Centre, Mahatma Gandhi Institute of Medical Sciences, Scwagram 442102, Dist. Wardha, Maharashtra State, India.
Reprint requests to Dr. P. Desikan, The Wellcome Trust Research Laboratory, Department of Gastrointestinal Sciences, Christian Medical College and Hospital, Vellore 632004, India.
Received for publication on 20 March 1995
Accepted for publication on 11 May 1995.