- Volume 63 , Number 3
- Page: 422–9
Integration of leprosy control into basic health services; an example from nepal
ABSTRACT
The need for integration of vertical projects into the Basic Health Services (BHS) has been felt in Nepal since 1968. In 1987 it was decided to provide integrated BHS all over the country. The Nepal Leprosy Control Project (NLCP) was one of the vertical projects which had to be integrated f rom that year. In order to prepare the BHS staff for this new task the NLCP developed a Comprehensive Leprosy Training course. Besides adequate training, three other prerequisites for successful integration are: a) adequate supply of drugs and equipment; b) regular supervision and specialist referral facilities; and c) a well functioning BHS system in which to integrate.This article tries to assess to what extent these prerequisites have been met for leprosy control in Nepal. To do this, some results of an evaluation of the training are used as well as existing literature on the functioning of the BHS system.
The first three prerequisites are not fully met, but problems and obstacles related to these are mainly due to problems in the last prerequisite: a not so well functioning BHS System. It was, therefore, recommended to continue a (semi)vertical support System of leprosy control in those districts where the BHS is not so well developed.
RÉSUMÉ
Le besoin d'intégrer les projets verticaux dans les Services de Santé de Base (SSB) a été ressenti au Népal depuis 1968. En 1987, il fut décidé de pourvoir tout le pays en SSB intégrés. Le Programme Népalais de Lutte contre la Lèpre (PNLL) était l'un des programmes verticaux qui devaient être intégrés à partir de cette année-là. Afin de préparer le personnel des SSB à cette nouvelle tâche, le PNLL dévelopa un cours général de formation sur la lèpre. En plus d'une formation adéquate, il y a trois autres conditions à la réussite de l'intégration: a) approvisionnement adéquat en médicaments et équipements; b) supervision régulière et possibilité de référer vers un spécialiste, et c) un système de SSB fonctionnant bien dans lequel on peut faire l'intégration. Cet article tente d'évaluer dans quelle mesure ces conditions ont été remplies en ce qui concerne la lutte contre la lèpre au Népal. Pour ce faire, on utilise certains résultats d'une évaluation de la formation ainsi que la littérature existante se rapportant au système des SSB. Les trois premières conditions ne sont pas entièrement remplies, mais les problèmes et les obstacles concernent surtout la troisième condition: un système de SSB ne fonctionnant pas très bien. Il a dès lors été recommandé de poursuivre un système de support (semi-)vertical pour la lutte contre la lèpre dans les districts où les SSB ne sont pas très bien développés.RESUMEN
En Nepal, desde 1968 se ha visto la necesidad de integrar proyectos verticales dentro de los Servicios Básicos de Salud (SBS). En 1987 se decidió proporcionar SBS integrados, a nivel nacional. El proyeoto sobre control de la lepra en Nepal (PCLN) fue uno de los proyectos verticales integrados al programa de SBS. Para preparar al personal del programa, el PCLN desarrolló un curso de entrenamiento comprensivo sobre la lepra. Además del entrenamiento se consideraron los siguientes tres prerrequisitos: a) el adeouado suministro de medicamentos y equipo; b) la continua supervisión y asesoría del proyecto; c) el adecuado funcionamiento del programa de SBS. Este articulo trata de establecer en que grado se han cubierto estos prerrequisitos en cuanto al programa de control de la lepra en Nepal. Para haoer esta evaluación, se han tomado en cuenta los resultados del curso de entrenamiento y la información publicada sobre el funcionamiento del sistema de los SBS. Los primaros tres prerrequisitos no se han cumplido completamente pero los problemas y obstáculos se han atribuido a fallas en el último prerrequisito: un sistema de SBS funcionando de manera inadeouada. Por lo tanto, se recomienda continuar con el apoyo (semi-) vertical del proyecto de control de la lepra en aquellos distritos donde el SBS no está bien desarrollado.The concept of integration of vertical projects into the basic health services (BHS)* is gaining wide acceptance, based on the consideration that it will lead to much more efficient use of staff, transportation and financial resources (3,4,9,11,14).
The World Health Organization (WHO) adopted the policy of primary health care (PHC) on the basis of the principle of equity and justice. This principle was laid down in 1978 at the International Conference on Primary Health Care in Alma-Ata with the proclamation of the goal of "Health for all by the year 2000." PHC services should make basic but essential health care accessible to individuals and families in the community through their full participation and at costs the community and country can afford(13.14).
For integration to be successful some prerequisites have been mentioned (23,6-9,14,15) and include: a) an adequate training of both managerial and technical staff; b) an adequate supply of drugs and equipment; c) regular supervision and specialist support and referral facilities; and d) a well-functioning basic health care system in which to integrate.
Since 1968 an urgently felt need for accelerating the development of integrated BHS was noted by government health officials in Nepal in order to take over the responsibility of malaria vigilance activities after eradication and to strengthen and develop the BHS as such (16). In late 1969 a pilot project was launched to develop integrated BHS in one district. Evaluation of this project showed that integrated BHS resulted in better services to the population and avoided duplication of effort. The provision of health care to the entire community had been largely achieved and, therefore, it was decided to extend the project(12, 16). The respective vertical projects were supposed to provide supplies and equipment for field-level activities, technical supervision, and also to organize a special training course for the integrated districts(12). In 1987 it was decided to provide integrated BHS all over the country at one and the same time.
Essential health care includes control of locally endemic diseases. The WHO has on various occasions urged member states to integrate leprosy control activities within the general health services (8).
In leprosy, there may be an additional positive effect. It could reduce the stigma attached to the disease, because it would be dealt with in the same manner as other diseases and not in a separate clinic by "outsiders" (6,8,11). In addition, early signs and symptoms of the disease, which are not always recognized as such by leprosy patients, could be detected during general examinations (16). Drug compliance and attendance also could, in the long run, be improved by making use of village health workers (VHWs) and community health volunteers (CHVs) (13).
A joint leprosy control project (LCP) run by the International Nepal Fellowship (INF)/His Majesty's Government/Nepal (HMG/N), supported by the German Leprosy Relief Association, is operating in the Western and Mid-Western Regions of Nepal. From 1975 to 1987 the LCP was run as a separate, vertical control program. In 1987 HMG/N decided to integrate the LCP into the basic health services.
When the LCP was run as a vertical project, one or two leprosy workers based in the district conducted leprosy clinics at the health posts (HP) once a month. Depending on the accessibility and the caseload they were, if needed, assisted by a mobile team (MT) from the Leprosy Control Section (LCS) of the Regional Office. After integration, the HP staff conduct the clinics themselves, while the district leprosy workers visit the clinics for supervision and support. Leprosy patients are, once diagnosed, registered in the health post. They should come to the clinic every month to be examined and to collect their medicines. They usually get a combination of drugs, the so-called multidrug therapy (MDT) according to the guidelines of the WHO (19). After completion of the drug therapy, the patient is released from treatment (RFT).
Although many introductory leprosy courses for BHS staff have been held at the Green Pastures Training Centre in Pokhara, Nepal, during the past 15 years, these were aimed at teaching health workers to recognize leprosy patients and to refer suspects to the LCP for treatment and management. Therefore, INF developed (in cooperation with the HMG/N LCS) a task-oriented leprosy training course, called the Comprehensive Leprosy Training (CLT). Its aim is to prepare BHS staff for integrated leprosy work. This 6-day training is given district-wise to groups of maximal 12 BHS staff of the same level.
This paper discusses to what extent the prerequisites for successful integration have been met in the case of the leprosy control program in Nepal.
METHODS
The aspects looked at to assess to what extent the four prerequisites are met are: a) adequate training of staff: number of staff who received training; involvement of trained staff in leprosy care; quality of care as perceived by patients and supervisors, b) an adequate supply of drugs and equipment: supply observed during visits and according to staff, c) effective supervision and referral system: structure of supervision and referral, d) a well-functioning BHS system in which to integrate: literature research on this subject. The first two points are mainly based on some of the results of an evaluation of the Comprehensive Leprosy Training (CLT).
The evaluation of the training is done according to the facility based assessment (FBA) method (5). This method uses a coordinated set of data collection activities designed to determine the extent to which patients arc properly diagnosed, treated, and cared for in the treatment facility. In this evaluation of the CLT, the data collection activities were: questionnaire survey, observation on the basis of checklists, and analysis of routine statistical data. The aims and objectives of the training were used as a guideline for the evaluation.
The district in which the first CLT was given in 1991 was selected as the pilot district. This district is situated in the flat southern plains of Nepal which have a relatively good infrastructure and better-developed health services than the hill and mountain districts. Since there had been no opportunity to do a pretraining questionnaire survey, a neighboring district also in the plain area was selected as the control district. In both districts the mobile team (MT) conducted leprosy clinics in some of the HPs. For comparison, a district in the hills without a MT was selected and included in the assessment.
Questionnaire survey. Two questionnaires have been developed in Nepal, one for leprosy patients and one for HP staff. During the development, two interviewers who were independent from the project were selected. They were introduced to the basics of leprosy and trained in interview techniques. They also pretested the questionnaires in nonselected districts. The questionnaire includes questions about the experience with/after the training and handover of care to the HP staff, treatment, care, provided information, etc. Questions with answer categories, based on answers given by patients during extensive pretesting of the questionnaires, were asked as open questions. Depending on the answers given, the interviewers picked out the matching categories. The respondent therefore did not know the expected answers.
The interviewers started their survey work in June 1992 in the "control" district with a pretraining survey. According to their schedule, they first visited all of the 10 HPs to interview the staff and then they went back on a clinic day to interview as many leprosy patients as possible. Some of the staff who were not present on the first visit were interviewed on the clinic day as well.
The second interview session was done in the 10 HPs and two hospitals of the pilot district 6 months after the leprosy control activities had been handed over to the BHS staff. The third survey was conducted in the hill district before CLT was provided (seven HPs and two hospitals). The fourth survey has been conducted in the pilot district again, 1 year after the handover of leprosy care. All of the interviews have been done by the same interviewers and according to the same schedule.
Checklist. An existing checklist was adjusted for the evaluation. It was completed by the Regional Leprosy Supervisors on their supervision visits to the HPs. Items included in the checklist were: involvement of HP staff in leprosy control activities, availability of medicines, number of registered and attending patients, competence of the staff.
The Regional Leprosy Supervisor visits the HPs on clinic days according to an annual schedule. Priority is given to HPs with a high caseload and HPs in districts where the care has been handed over to the HP staff.
Statistical data. Routine statistical data can be used to measure trends. Important are registered prevalence, new patients found, disability-, child- and multibacillary-proportion among new cases. Data were available from monthly reports, aggregated from patient cards.
Data from the questionnaires were translated into English. These data and the data from the observation checklists were then entered into a microcomputer and analyzed with Epi-Info, a software package designed for field-based epidemiological data handling (Dean, A. G., Dean, J. A., Burton, A. H. and Dicker, R. C. Epi-Info Version 5. Atlanta: Centers for Disease Control, 1990).
In this article, attention is focused only on interview and observation results. The use of the FBA method for the evaluation of leprosy training will be discussed in a separate article.
RESULTS
Samples. The numbers of patients and staff interviewed in the four questionnaire surveys are shown in Table 1. The patient interview sample (24%-38%) represents the number of interviewed patients on treatment divided by the number of patients registered for treatment. The patients "on observation" were omitted because nothing can be said about when they should visit the HP. Assuming that in every HP five HP-based staff [1 health assistant (HA), 2 assistant health workers (AHW) and 2 auxiliary nurse midwives (ANM)] are posted (the normal number), the interview sample of HP-based staff ranged between 51% and 66%.
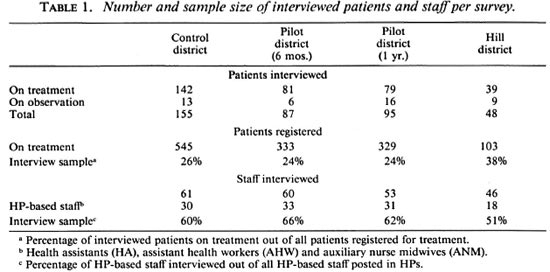
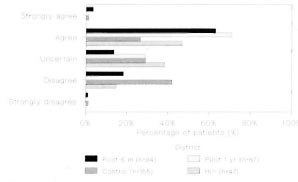
Fig. 1. Opinion about the statement: "The HP staff knows what to do."
The Regional Leprosy Supervisors visited four HPs and one hospital in the pilot district between 0 and 6 months after the handover and two HPs and one hospital between 7 months and 1 year after the handover. In the control district five HPs were visited before the CLT was conducted. In four of these HPs the Mobile Team conducted the clinic. No supervision information was available for the hill district. More than 70% of the HP-based staff were present during the visits, but some data about posted and present staff were missing.
In the pilot district, 112 staff members had done the CLT, of whom 36 were HP-based staff. Of all the staff, after 6 months 37% were interviewed and after 1 year, 35%. Of the HP-based staff, during both interviews 75% (27) of the trained staff have been interviewed.
HP staff involvement in leprosy care. Although according to their job descriptions HP staff should do the leprosy care, not all staff are involved in the care. The numbers of HP-based staff involved, as stated during the interview as well as observed during supervision visits, are shown in Tables 2A and 2B.
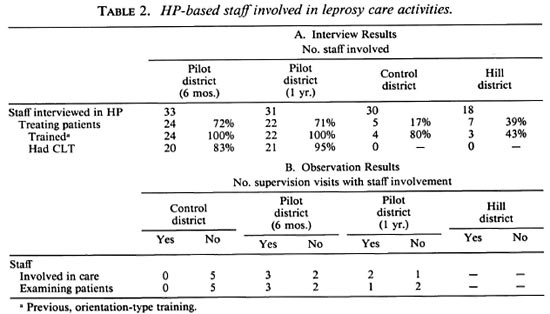
In the pilot district more HP-based staff said they were involved than in the control and hill district (71% vs 17% and 39%, respectively). Of the 27 CLT-trained HP-based staff, 20 (74%) and 21 (78%), respectively, said they were treating leprosy patients (Table 2A).
During the supervision visits, HP staff involvement has been observed in some HPs (3 out of 5 and 2 out of 3, respectively) in the pilot district. In the control district HP staff were not reported to be involved in leprosy care. Although involvement of HP staff was observed, at no occasion have the HP staff taken care of the leprosy work by themselves with only supervision by the district or regional leprosy supervisors (Table 2B).
Quality of care. During all interview sessions, more than 90% of the patients reported that the leprosy care received was good. When asked in another way, however, the patients seemed less satisfied. Three statements about care were given to the patients. The statements were: 1. The HP staff knows what to do. 2. The HP staff is more interested in other diseases. 3. The HP staff listens to my complaints. The respondents could choose answers from the following scale: 1 = strongly agree; 2 = agree; 3 = uncertain; 4 = disagree; 5 = strongly disagree. Figures 1, 2 and 3 demonstrate the opinion about these three statements for the surveyed districts.
In the pilot district most patients agreed with the first statement, while in the control and hill district patients are uncertain or even disagree with the statement (Fig. 1). The second statement shows uncertainty by most of the patients. In the control district more patients agreed than disagreed with the statement (Fig. 2). In each survey most patients said the HP staff listen to their complaints (Fig. 3), but in the control district some patients were uncertain (30%) or even disagreed (21%). Overall, the patients in the pilot district seemed to be more satisfied with the care of the HP staff.
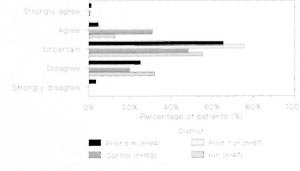
Fig. 2. Opinion about the statement: "The HP staffis more interested in other diseases."
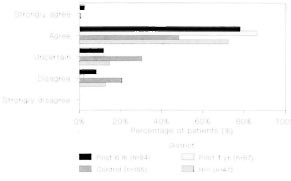
Fig. 3. Opinion about the statement: "The HP staff listens to my complaints."
The 40 and 28 patients in the pilot district (after 6 months and 1 year, respectively) who were on treatment for 6 months before the handover were asked if they had experienced changes after the handover. Fourteen of the 40 patients (35%) and 2 of the 28 patients (7%) said that some aspects of care were better previously; 63% and 64%, respectively, said they did not experience any changes.
During the supervision visits, the HP staff involved in leprosy care were not found to be working very competently. In two of the three HPs where staff were involved during the first interview session in the pilot district, most of the aspects of leprosy care were classified as not competently performed. After 1 year the staff competency was classified as good in only one HP.
Drugs and equipment. The supply of leprosy drugs was reported to be sufficient by the leprosy supervisors, although at some HPs the supply was provided by the district leprosy supervisors and not kept in the HPs. Dressing materials were available during only two visits in the pilot district during the second survey period.
According to the HP staff, during the first survey period in two HPs only dapsone, which is used for monotherapy, was available. During the second period, however, MDT was said to be available in all HPs. In the control district, MDT was only said to be available in three HPs.
Supervision and referral. Although the Regional Leprosy Supervisors are not able to visit the HPs very often, the District Leprosy Supervisors visit the HPs every month on clinic days. They usually do most of the leprosy care. The referral system makes it possible to refer patients with problems via the monthly clinic at the district headquarters, run by Regional Leprosy staff, to the leprosy hospital at the Regional headquarters.
DISCUSSION
As mentioned above, effective integration of a vertical project into the BHS requires that four conditions are present: a) a welltrained staff; b) an adequate supply of drugs and equipment; c) effective supervision and referral system; and d) a well-functioning BHS system in which to integrate.
The CLT has been taken by most of the staff eligible for it. They seemed to be positive about the course, and many were actively involved in the care of leprosy patients. According to the observations of the Regional Leprosy Supervisors, the care provided by the HP staff was not always up to standard. Specific attention therefore should be paid to the weak aspects during follow-up training and supervision visits.
The patients said the care was good, although this may be the "expected answer" since their opinions of the statements about the HP staff were not equally positive. A bias also might have occurred due to the fact that the patients interviewed are mostly regular patients. Most patients who have experienced changes after the handover were referring to the care of the Mobile Team which was said to be better and more elaborate, e.g., provision of nonleprosy medicines. The provision of medicine not related to leprosy, however, should not be a measure of the quality of leprosy care. It also should be noted that the HP staff were nowhere the only ones providing leprosy care; the leprosy supervisors also were actively involved. Patients do not distinguish the care of the HP staff from that of the leprosy staff.
Although in some cases no drugs were available in the HP, the district leprosy staff could provide them. The availability of drugs seemed to have been improved 1 year after handover. It should still be monitored carefully, because leprosy staff will not always be assisting the leprosy clinic in the future. Dressing materials were a larger problem. The importance of dressing as well as the maintenance of materials and equipment should be stressed, and new materials will have to be provided.
The supervision is being done by the District Leprosy Supervisors as well as by the Regional Leprosy Supervisors. The latter have no delegated authority over the BHS stafT (18). This could cause problems and clarification should be given.
From this information, it can be concluded that although some staff were involved in the care of leprosy patients after they have done a comprehensive leprosy training, improvement in their skills and encouragement is still needed. This is a specific task for District and Regional Supervisors. The supply of drugs seems to be no problem, but the availability of dressing materials is. The supervision and referral structure are quite satisfactory.
The obstacles for successful integration, found within these three preconditions, are more or less related to the fourth prerequisite: an adequate functioning of the general health service. This factor was already recognized as an important factor for integration 20 years ago (15).
Health management is critical for success and managerial skills merit increasing priority in developing countries, especially at intermediate/district levels where decision making and support structures must be built up (20). Careful attention to the specific conditions in a particular country are necessary before leaping into initiatives which can have very negative consequences in the short and even in the long term (2).
The problems of the health care system in Nepal have been discussed at many instances, and also by HMG/N itself (10). The uniform distribution of health facilities in every district does not correspond with the principle of the primary health care system that it should be near to the people. It leads to long walking distances in the mountain areas while there are large numbers of patients in the plains (12). A uniform distribution of drugs and equipment does not meet recognized needs because there is no relation between the quantity of drugs and the illness patterns and population coverage estimates (10,12). The budget is inadequate and is not released in time (18). The facilities are poorly maintained (10). The management and support functions often have limited capacity. There is no regular supervision, monitoring and evaluation of the programs (10,18 and His Majesty's Government of Nepal, Ministry of Health, National Leprosy Policy, Kathmandu, 1991). Often in the HPs, as well as among the District Leprosy Supervisors, sufficient trained staff is lacking due to low salaries and allowances (1,10,18). Lack of facilities and opportunities for promotion and private practice lead to even more staffing problems in rural and remote areas (10). With integration the staff have to do more tasks than before at no extra remuneration. The HP staff in the integrated HP do not feel responsible for the leprosy service. They give preliminary treatment and refer the patients to the leprosy workers (12).
All of these factors are leading to a low quality of care, which partly explains the low levels of attendance at HPs. It is estimated that the national health structure is within reach of only 15% of the population, mostly in and around urban areas (10). The experience of integrating the services of vertical projects docs not provide an optimistic picture regarding the provision of an integrated BHS all over the country by the end of the year 2000 to meet the target (12).
Integration should be accepted as a long term process, dependent on development of the BHS and district management and support infrastructure (18). A certain vertical structure, therefore, remains justifiable (centrally or regionally) for effective integration at the intermediate level. In districts with less-developed BHS, the (semi)vertical structure of leprosy control work needs to be continued until the BHS are ready for integration.
REFERENCES
1. Agency for International Development (AID). Health Care in Nepal: an assessment of AID's program. Washington, D.C., 1991.
2. Allman, J., Rohde, J. and Wray, J. Integration and disintegration: the case of family planning in Haiti. Health Policy Plan. 2(1987)236-244.
3. Bijleveld, I. In reality: a medical anthropologist's reservations about the viability of leprosy control within primary health care. Lepr. Rev. 53(1982)181-192.
4. Browne, G. The integration of leprosy into the general health services. Lepr. Rev. 43(1972)16-20.
5. Bryce, J., Toole, M. J., Waldman, R. J. and Voigt, A. Assessing the quality of facility-based child survival services. Health Policy Plan. 7( 1992)155-163.
6. Buchmann, H. Leprosy Control Services as an Integral Part of Primary Health Care Programs in Developing Countries. Wurzberg: German Leprosy Relief Association, 1978.
7. Chaulet, P. Integrating tuberculosis control activities into the primary health care system at district level. Bull. Int. UAT. 64(1989)33-35.
8. Feenstra, P. Needs and prospects for epidemiological tools in leprosy control. Lepr. Rev. 63 Suppl.(1992)3s-10s.
9. Haydar, A. H. Leprosy control in a primary health care programme in the Sudan. Lepr. Rev. 53(1982)175-180.
10. Henderson, P. Sustainability in the Health Sector, Part 1: Nepal Case Study. Kathmandu: Save the Children Fund (UK), 1993.
11. Hogerzeil, L. M. and Reddy P. K. General health education as the main approach to leprosy control, Dichpalli, India. Lepr. Rev. 53(1982)195-199.
12. Mathema, P. Primary Health Care in Nepal. Kathmandu: V. R. Mathema, 1987.
13. McDougall, A. C. Leprosy and primary health care. (Editorial) Lepr. Rev. 53(1982)161-163.
14. Nkinda, S. J. Leprosy and primary health care: Tanzania. Lepr. Rev. 53(1982)165-173.
15. Ramu, G. Integration of leprosy with general health service. Lepr. in India XLV 4(1973)263-266.
16. Shrestha, S. K. Integrated basic health services in the district of Bara, Narayani Zone, Nepal. In: Community and Health, an Inquiry into Primary Health Care in Asia . Sepulveda, C. and Metha, N., ed. UNAPDI Health Technical Paper #35/ BCS4, 1980, pp. 198-203.
17. Wardekar, R. V. Integration of leprosy work into general medical service. Int. J. Lepr. 37(1969)308-309.
18. Weakliam, D. Quality of care in a tuberculosis control programme: evaluative study of integrated tuberculosis control activities at health posts in Surkhet District, Nepal. Dissertation, University of Liverpool 1992.
19. World Health Organization. Multidrug therapy for leprosy; an end of sight. Geneva: World Health Organization, 1988.
20. World Health Organization. Tuberculosis Control as an integral Part of Primary Health Care. Geneva: World Health Organization. 1988.
1. M.Sc, Research Associate.
2. Ph.D., Director, INF/Lcprosy Control Project, Pokhara, Nepal.
3. M.D., Chief, HMG/N Leprosy Control Program, Pokhara, Nepal.
Reprint requests to Dr. W. H. van Brakel, INF/LCP, P. O. Box 5, Pokhara, Nepal.
Received for publication on 22 March 1994
Accepted for publication in revised form on 21 June 1995.
* Abbreviations used: AHW = auxiliary health workers; ANM = auxiliary nurse midwives; BHS = bas ic health services; CHVs = community health volunteers; CLT = comprehensive leprosy training; FBA = facility based assessment; HA = health assistants; HMG/N = His Majesty's Government/Nepal; HP = health post; INF = International Nepal Fellowship; LCP = leprosy control project; LCS = leprosy control section; MDT = multidrug therapy; MT = mobile team; PHC = primary health care; RFT = released from treatment; VHWs = village health workers; WHO = World Health Organization.