- Volume 63 , Number 3
- Page: 448–50
Rhinosporidiosis in Leprosy; a case report
In an effort to increase the utility of the JOURNAL in continuing medical education, in this section we welcome contributions dealing with practical problems in leprosy work. Submissions to this section will undergo minimal editorial changes and may well contain controversial po'ints. Letters to the Editor pointing out other viewpoints are welcome.
Leprosy is a chronic, granulomatous, infectious disease and is known to be associated with other granulomatous infections such as tuberculosis' and syphilis.2 Deep mycotic infections like chromoblastomycosis3 and mycetomas4 also have been reported in leprosy patients. Rhinosporidiosis is a fungal infection which commonly affects the nasal mucosa. Although it is endemic in some districts of Tamil Nadu, India, hardly any association between leprosy and rhinosporidiosis has been noticed. In this paper we report a case of rhinosporidiosis from Tamil Nadu in a patient with borderline tuberculoid leprosy and also record the efficacy of dapsone in the treatment of rhinosporidiosis.
Case Report
A 55-year-old male, agricultural laborer reported to the outpatient department on September 1964 with two small hypopigmented patches, one on the right side of his chest and the other on the left forearm. On examination the patches were slightly raised and were anesthetic to light touch. There was no nerve thickening or muscle paralysis. He was diagnosed clinically as borderline tuberculoid leprosy, was treated with dapsone 100 mg daily for 8 years, and was released from treatment on October 1972. However, he was attending the outpatient department once in a while for treatment for his bronchial asthma.
In January 1982 he reported with epistaxis. An ear-nose-throat (ENT) examination showed a small polyp in the left nostril. Although rhinosporidiosis was suspected, no firm diagnosis was made at that time. In June 1990 he complained of hoarseness of voice and difficulty in swallowing. An ENT examination at that time revealed a large nasopharyngeal polyp which was diagnosed clinically as rhinosporidiosis, and the patient was advised surgery. Initially he was not willing to undergo an operation, but he later consented to surgery because his breathing was becoming increasingly difficult. He was operated on in September 1990.
The pathological examination of the nasal lesion was done at the Armed Forces Institute of Pathology, Washington, D.C., U.S.A. It showed a polypoid structure lined partly by ciliated columnar epithelium and mostly by stratified squamous epithelium, and contained a large number of sporangia packed with small spores of about 6 µ m to 7 µ m in diameter characteristic of rhinosporidiosis. The sporangia were at various stages of development and were embedded in loose connective tissue densely infiltrated by lymphocytes, plasma cells and macrophages.
The patient was seen again in November 1992, and there was a suspicious lesion in the previously operated area. Dapsone has been reported to be effective in the treatment of rhinosporidiosis5 and, therefore, he was advised to take dapsone 100 mg daily.
When he reported in July 1993 with a recurrent growth in the nasopharyngeal area, he was found to have taken dapsone irregularly and only for 3 months. He was operated on again in August 1993 and, because of excessive bleeding, the growth was only partially removed.
A histopathological examination of the specimen showed a polypoid lesion covered by stratified squamous epithelium containing many empty degenerating sporangia (Fig. 1), only a few containing spores (Fig. 2). There also were several areas showing granulomatous reaction composed of epithelioid cells and foreign body giant cells around some of the degenerating organisms (Fig. 3). The patient was again put on dapsone 100 mg daily and was asked to be regular in taking the drug. When he was examined in February 1995 it was found that the lesion at the nasopharyngeal area had completely disappeared.
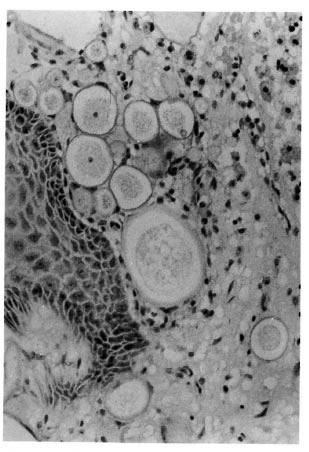
Fig. 1. Nasal polyp with thinosporidiosis showing several empty sporangia [hematoxylin and eosin(H&E)x250].
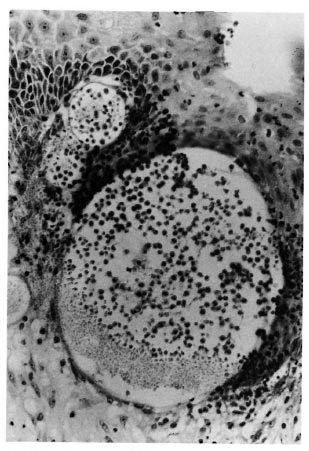
Fig. 2. A few sporangia containing many spores embedded in the stratified squamous epithelium (H&Ex250).
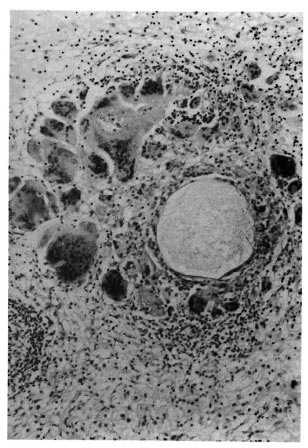
Fig. 3. Granulomatosis reaction composed of epithelioid cells and foreign body giant cells around a degenerating sporangium (H&E x90).
Comments
Rhinosporidiosis is a chronic infectious disease caused by Rhinosporidiutn seeberi. 6 The organs commonly affected are the nasal mucosa and the anterior aspect of the eye. These are also the two sites often affected in lepromatous disease. The infection is common among agricultural laborers exposed to muddy water and dust. It is thought that the soil particles carry the infecting spores.
In a recent paper the destruction of the parasitic agent Rhinosporidiutn seeberi with granuloma formation following dapsone therapy had been well described.7 During the biopsy examination of the lesion in this patient in August 1993 when he was taking dapsone irregularly, the lesion showed degenerative changes of the parasite with well-marked granuloma formation. When he took dapsone regularly, the partially removed lesion completely disappeared and he was disease free for a period of 18 months.
The only case of rhinosporidiosis associated with leprosy was reported from Raipur, Madhya Pradesh, India.8 It is possible that since a large majority of the leprosy patients in Tamil Nadu are covered by mul tidrug therapy (which includes dapsone), infection with rhinosporidiosis has not been reported so far in leprosy patients in Tamil Nadu.
- Joseph Jayakumar, M.B.B.S., D.T.M.&H.
- M. Aschhoff, M.D.
- Charles K. Job, M.D., F.R.C.Path.
St. Thomas Hospital and Leprosy Center
Chettupattu 606801
T.S. District
Tamil Nadu, India
Acknowledgment. This study was made possible through financial support received from the American Leprosy Missions International, Greenville, South Carolina, U.S.A. We are grateful to Dr. W. M. Meyers, Armed Forces Institute of Pathology, Washington, D.C., U.S.A., for the pathological report and to Miss K. Jayanthi for secretarial assistance.
1. Premnath, M. and Ramu, G. The association of leprosy and tuberculosis. J. Indian Med. Assn. 67(1976)143-145.
2. Murray, K. A. Syphilis in patients with Hansen's disease. Int. J. Lepr. 50(1982)152-158.
3. Pavithran, K. Chromoblastomycosis in a residual patch of leprosy. Indian J. Lepr. 60(1988)444-447.
4. Jayakumar, J., Aschhoff, M. and Renuka, G. Mycetomas in leprosy. Indian J. Lepr. 65(1993)229-233.
5. Bhanu, T. S. New drug regime for rhinosporidiosis. Indian J. Otolaryngol. 32(1980)96-97.
6. Karunaretne, W. A. E. Rhinosporidiosis in Man. London: Athlone Press, 1964.
7. Job, A., Venkateswaran, S., Mathen, M., Krishnaswamy, H. and Raman, R. Medical therapy of rhinosporidiosis with dapsone. J. Laryngol. Otol. 107 (1993) 809-812.
8. Poricha, D., Pradhan, S. C. and Agrawal, M. N. Cutaneous rhinosporidiosis in a patient of lepromatous leprosy; a case report. Indian J. Lepr. 58(1986)626-6277.
Reprint requests to Dr. Job.