- Volume 63 , Number 3
- Page: 450–2
An unusual presentation of recurrent corneal abrasion in a lepromatous patient with impaired corneal sensation
It is well known that in a certain category of leprosy patients the corneal sensation often is impaired. Although there has been a study1 that described a correlation between impaired corneal sensation and various ocular complications, the literature is scarce on the precise nature and magnitude in which corneal damage occurs in patients with reduced corneal sensation. Since most studies pertaining to corneal sensation were cross-sectional,2,3 it is not quite clear whether the ocular complications follow corneal sensory impairment or whether the corneal sensation is decreased as a result of these ocular complications.
In this communication we report a leprosy patient who had decreased corneal sensation and who developed an unusual corneal abrasion in the eye that had markedly reduced corneal sensation.
Case Report
A 57-year-old, male, lepromatous leprosy patient reported in January 1995 to the eye outpatient department of the Schieffelin Leprosy Research and Training Center in South India with complaints of discomfort and redness in the left eye for a week. The patient had been diagnosed with lepromatous leprosy in 1972, and had received dapsone monotherapy from 1972 to 1986. He was subsequently given 27 doses of multidrug therapy (MDT) according to the World Health Organization (WHO) regimen for multibacillary patients and released from treatment in April 1988. Skin smears were negative from 1990. No history of past episodes of type 1 or type 2 reactions could be elicited. However, there was record of iridocyclitis occurring in the right eye in 1990. There was no history of trauma to either eye.
On examination, the right eye had a visual acuity of 3/60 that did not improve with corrective glasses. Old keratic precipitates without any sign of active iridocyclitis and a very irregular, small pupil that did not respond to light stimuli due to dense posterior synechiae were present. The lens had a cataract. The applanation tension was 12 mmHg. The corneal sensation estimated by the Cochet and Bonnet esthesiometer was 3.20 gm/sq/mm (30-mm fiber length). The left eye also had a visual acuity of 3/60. A 4 mm x 2 mm oval, corneal, epithelial abrasion that stained with fluorescein was found in the 2 o'clock and 3 o'clock positions 1 mm inside the limbus. There were a few old keratic precipitates and a mild flare. Cataract was present with posterior synechiae in the 4 o'clock position. The applanation tension was 4 mmHg. The corneal sensation was 6.64 gm/sq/mm (20-mm fiber length). There was bilateral madarosis and no lagophthalmos. The patient satisfied all attributes of a case of resolved lepromatous leprosy with eye complications.
The right eye was treated with topical 1 % atropine drops and 10% phenylephrine drops to release the posterior synechiae. The left eye was treated with ciprofloxacin eye drops given every waking hour and 1% atropine eye drops three times a day. The abrasion was completely healed the next day with no breaks in the epithelium and the fluorescein staining was negative. The topical drops were continued for another 10 days. However, a week later the patient complained of mild pain in the left eye and slit-lamp biomicroscopy showed multiple, thin, hair-like, linear, vertical abrasions that stained with fluorescein dye (The Fig.). This was an unusual presentation and on close questioning the patient admitted to having rubbed his eye with a cotton cloth towel. This seemed the only plausible explanation for this peculiar presentation. Ciprofloxacin and atropine drops were given again, and the abrasions healed completely by the next day. Despite repeated admonition and advice not to rub the eye, the patient again developed similar linear abrasions on the cornea in a week's time due to a similar reason. With adequate treatment the abrasions healed, and 3 weeks after the date of reporting, the corneal surface of the left eye remains normal.
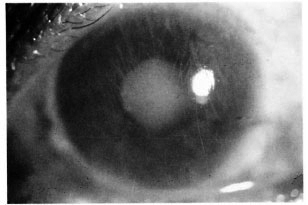
The figure. Superficial linear corneal abrasions.
The extent to which sensory impairment of the cornea contributes to ocular morbidity in leprosy has not been well documented. We have presented this case in which a patient with decreased corneal sensation developed recurrent corneal abrasions while still an inpatient in the hospital. Even after receiving intensive health education, he could not resist the temptation to rub his eyes with the cloth again and again. However, for the present repeated instructions appear to have had some effect. The progression of an abrasion into a secondarily infected corneal ulcer is not very difficult, and may lead to a situation where blindness is inevitable. This case demonstrates the inadequacies still present in trying to manage a patient presenting with decreased corneal sensation. It also highlights the importance of knowing whether a patient has good corneal sensation and the importance of formulating systematic, intensive and continuous eye care for these patients. The onus of protecting the eye rests on good and frequent eye check ups and ceaseless eye health education because, at present, we do not have any other protective methods to counter the sensory impairment of the cornea.
The patients who are released from treatment (RFT) are seen much less frequently than those under antileprosy treatment. This is a potentially dangerous situation for those with reduced corneal sensation, as this patient illustrates. When leprosy patients are removed from the register and are no longer considered patients, it is necessary to assess the corneal sensation of these patients before they are released from treatment. If, at that time, any corneal sensory deficit is detected, it is imperative that their eyes are periodically checked even after RFT.
Estimating corneal sensation under field conditions has its limitations since it tends to be highly subjective. This is an area in which controlled studies are necessary in order to quantify and to standardize as much as possible the assessment of corneal sensation using commonplace things, such as a cotton wisp or a piece of sewing thread. Attempts are underway at this institution to quantify the sensory testing of the cornea using a cotton wisp which, at present, is the only practical tool for estimating corneal sensation under field conditions by the paramedical worker. A study is being designed to check variables such as the thickness of the cotton wisp, where the cotton wisp is held from its tip, the area on the cornea where the tip of the wisp is to be placed, and the verbal response or the blink reaction of the patient as a response to the touch stimuli. The testing is to be correlated with readings obtained with the Cochet and Bonnet esthesiometer and with readings obtained from matched nonleprosy controls. Since quantification of corneal sensation is possible with the Cochet and Bonnet esthesiometer, it would also be important to do a longitudinal study in a group of leprosy patients to assess the frequency of ocular complications with the severity of corneal sensory loss.
- Ebenezer Daniel, M.B.B.S., M.S., D.O.
Head, Department of Ophthalmology
Schiejfelin Leprosy Research and Training Center
Karigiri, North Arcot District
Tamil Nadu 632106, India
- Margaret E. Brand, M.B.B.S.
7026 California Lane SW
Seattle, WA 98116, U.S.A.
Acknowledgment. We would like to thank Dr. C. K.. Job for his useful discussion and advice which helped in the preparation of this clinical note.
1. Karacorlu, M. A., Cakiner, T. and Saylan, T. Corneal sensitivity and correlations between decreased sensitivity and anterior segment pathology in ocular leprosy. Br. J. Ophthalmol. 75(1991)117-119.
2. Shorey, P., Krishnan, M. M., Dhawan, S. and Garg, B. R. Ocular changes in reactions in leprosy. Lepr. Rev. 60(1989)102-108.
3. Hobbs, H. E. and Choyce, D. P. The blinding lesions of leprosy. Lepr. Rev. 42(1971)131-137.