- Volume 63 , Number 2
- Page: 265–8
Prevalence of maxillary sinusitis in leprous individuals from a medieval leprosy hospital
ABSTRACT
The maxillary sinuses of 133 skeletons f rom the medieval hospital of St. James and St. Mary Magdalene, Chichester, England, were analyzed for evidence of sinusitis. Of the sample, 16 individuals were considered to have suffered f rom lepromatous leprosy and 13 f rom tuberculoid leprosy. The most common bone change seen within the sinuses was the presence of new bone formation followed by pitting. Bone change was seen in 56.3% (9 of 16) of the individuals with lepromatous leprosy and 54.8% (57 of 104) of nonleprous individuals. These results are not statistically significant. Clinical evidence suggests that one should see a higher frequency in the lepromatous group. Possible explanations of this include environmental factors promoting the spread of droplet infection in an immunosuppresscd community, in addition to which the small sample of leprous skeletons may bias the result.RÉSUMÉ
Les sinus maxillaires de 133 squelettes provenant de l'hôpital médiéval de Saint-Jacques et Sainte Marie Madeleine, à Chichester, en Angleterre, ont été examinés pour rechercher les signes de sinusite. Dans l'échantillon, 16 personnes furent considérées comme ayant souffert de lèpre lépromateuse et 13 de lèpre tuberculoide. La modification osseuse la plus fréquemment vue dans les sinus était la présence de nouvelle formation osseuse, suivie du creusement de géodes. Des modifications osseuses ont été observées chez 56.3% (9 sur 16) des personnes avec une lèpre lépromateuse et 54.8% (57 sur 104) des personnes non lépreuses. Ces résultats ne sont pas statistiquement significatifs. L'évidence clinique suggère que l'on devrait observer une fréquence plue élevée dans le groupe lépromateux. Les explications possibles incluent des facteurs environnementaux facilitant la dissémination de goutelettes infectieuses dans une communauté immunodéprimée, en plus du fait que le petit nombre de squelettes lépreux peut biaiser les résultats.RESUMEN
Se analizaron los senos maxilares de 133 esqueletos del hospital medieval de St. James and St. Magdalene, en Chichester, Inglaterra, para buscar evidencias de sinusitis. Se estableció que de los individuos estudiados 16 tuvieron lepra lepromatosa y 13 lepra tuberculoide. El cambio más común dentro de los senos fue la presencia de neoformaciones óseas con horadaciones. Esto se observó en el 56.3% (9 de 16) de los individuos con lepra lepromatosa y en el 54.8% (57 de 104) de los individuos no leprosos. Estos resultados no difieren estadísticamente entre si aún cuando las evidencias clínicas sugieren que la frecuencia de estas alteraciones debería ser más elevada en el grupo lepromatosos que en la población no leprosa. Dentro de las posibles explicaciones a este hallazgo se incluye la participación de factores ambientales capaces de promover la dispersión de la infección por gotitas de exudado nasal en una comunidad inmunosuprimida. El pequeño tamaño de la muestra de esqueletos afectados por la lepra también pudo haber influido en el resultado.A number of papers have recently explored the association between sinusitis and its occurrence in individuals with lepromatous leprosy ( 5,6.16,17). No systematic study of the relationship between these two diseases appears to have been carried out forarcheological material. Moller-Christensen, in his classic study of Danish leprous skeletons, mentions only briefly the presence of sinusitis, and does not associate the two conditions (14).
An investigation into maxillary sinusitis in the remains of individuals from the medieval hospital of St. James and St. Mary Magdalene, Chichester, England, offered an opportunity to study the possible relationship between this condition and leprosy in an archeological population.
MATERIALS AND METHODS
The sample of skeletons used for this investigation was derived from the cemetery of the hospital of St. James and St. Mary Magdalene, Chichester, England. The hospital was founded in A.D. 1118 to house male leprosy sufferers. With the decline in leprosy in the later Middle Ages there was a change in function of the hospital to that of an almshouse, the last documentary evidence for leprous inmates being recorded in A.D. 1418 (12).
Of the total cemetary adult population, 133 skeletons had sufficiently well preserved maxillary antra to be included in the present study. This inclusion was determined by the presence of at least one antral floor. Of the 133 skeletons 16 had bone changes exhibiting the rhinomaxillary syndrome pathognomic of lepromatous leprosy (1); 13 had tuberculoid leprosy, diagnosed by the absence of rhinomaxillary change and only unilateral hand/foot changes; the remaining 104 skeletons had no obvious manifestations of leprosy (11).
All sinuses were analyzed visually for the presence of bone change. Viewing of intact antra was performed using straight, 30º and 70º Storz. sinuscopes connected to a Rimmer Brothers CLS 150-2 light box. Access to intact antra was gained by trephining the posterior aspect of the maxilla. Radiography proved to be of little use for the study of sinusitis in dry bone since the bone deposits are too subtle to be identified on X-ray.
RESULTS
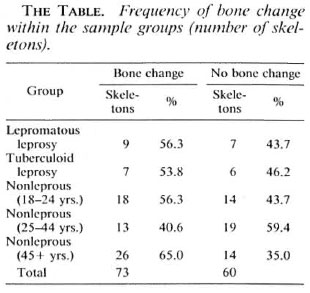
The most common changes seen within the antra were pitting and bone formation on the walls and floors (The Figure). Of these, bone formation was the most common, ranging in appearance from localized depositions of bone to the formation of new bone covering most of the antral floor and walls. In what is believed to be the early stages of the disease, the new bone formation is cancellous in appearance, subsequently remodeling to form compact bone. The Table shows the frequency of bone change in each of the groups studied. From the results it can be seen that there is little difference in frequency between lepromatous, tuberculoid and nonleprous individuals. A χ2 test comparing nonleprous and lepromatous individuals yielded a value of 0.026 (df rejection value at 0.1 = 2.74), thus suggesting that there is no significant difference in the frequency of sinusitis between these two groups.

The figure. Changes within the antra showing pitting and new bone formation within the maxillary sinus.
DISCUSSION
Bone formation within the sinuses was the most common finding in all groups. Because the periosteum retains osteoblastic potential throughout life, evidence of periosteal reaction would be expected in response to chronic disease; this would take the form of new bone formation. Von Buchner and Lessel have commented that (18)while evidence among the classic literature for bone change as a result of chronic sinusitis is scant, the majority of authors support the possibility of bone involvement. From their own studies they found evidence of osseous changes in 16 out of 64 patients in the form of periosteal reaction of varying extent. Histological study showed that the bone formation was characterized by delicate bars of bone. The possibility of bone formation also has been noted by Norlander, et al. (15), who found evidence for periosteal thickening associated with fibroblast proliferation, bone resorption and/or bone formation in experimental animals with deliberately induced chronic sinusitis.
A high frequency of nasal infection has been noted in patients with lepromatous leprosy (3,10). Because the antral mucosa is essentially a continuation of the nasal mucosa, involvement of the sinuses in lepromatous leprosy would be anticipated. It has been noted that the nasal mucosa tends to be involved early in leprosy (8,9), although the paranasal sinuses are more likely to be infected in the later stages of the disease (l6).
Radiography has been used by a number of workers to assess the level of antral involvement. Hauhnar, et al. (5) found that 57.1% (40 of 70) of patients had radiographic abnormalities, Soni (16) found 60% (18 of 30), and Barton (2) 100% (16 of 16). The most common finding was a thickening of the antral mucosa. Sinuscopic investigation demonstrated the most common finding to be inflammation of the mucosa, followed by ulceration and granulomas (6,17).
The results of our survey would seem to suggest that there is little difference in the frequency of sinusitis between leprous and nonleprous individuals in this sample. From the clinical literature, a greater frequency in the lepromatous group due to the involvement of the nasal mucosa in the disease process is suggested. Therefore, an explanation for the similarity between the two groups must be sought. It must be stated that the sample population was small, with only 16 individuals being classed as lepromatous. It is possible that some individuals might not have yet displayed bone lesions.
Viral infections, notably upper respiratory tract infections, are major factors in predisposing an individual to sinus infection. The most common viral infection in humans is the common cold. Viral infections cause swelling of the mucous membrane, resulting in obstruction of the ostium, reduced sinus drainage, and a multiplication ofthe normal nasal flora (7,19). Repeated attacks of acute sinusitis may lead to an individual developing chronic sinusitis. Any factor which impairs the drainage of the sinus will predispose the antra to secondary bacterial infection and thus, potentially, sinusitis.
General (7,19). A number of systemic defects can increase the incidence of infection, such as malnutrition and the presence of chronic infection (4). Environmental pollutants, such as smoke particles, can cause ciliary paralysis and, thus, increase the risk of infection ( ) . Any factor which increases the chance of droplet infection will also predispose to sinusitis. Overcrowding, underventilation and overheating are all favorable to droplet infection. It is these same factors of inadequate nutrition and poor housing that are important in the spread of leprosy (9).
Within the context of the confined nature of much medieval urban housing, it is not surprising that the population was equally predisposed to sinusitis. It is possible that many of the individuals used in our sample represent the disadvantaged of medieval society. Determining the exact etiology of sinusitis observed in this cemetery population is difficult due to the multifactoral etiological nature of this disease. Generalized predisposing factors, such as those increasing the risk of droplet infection, inadequate diet and depressed immune status, may overide what effect leprosy has in predisposing to sinusitis and, thus, explain why there is homogeneity among the sample.
Acknowledgment. We would like to acknowledge the help of Mrs. Anne Pearson in translating the paper by Von Buchner and Lessel, Ms Jean Brown for photography, Ms Mary Lewis for her information on leprous individuals, and the Chichester District Council
REFERENCES
1. ANDERSON, J. G. and MANCHESTER, K. The rhinomaxillary syndrome in leprosy: a clinical, radiological and palaeopathological study. Int. J. Ostcoarchacol 2(1992)121-129.
2. BARTON, R. P. E. Radiological changes of the paranasal sinuses in leprosy. J. Laryngol. Otol. 93(1979)597-600.
3. BARTON, R. P. E. and MCDOUGALL, A. C. The paranasal sinuses in lepromatous leprosy. Lepr. India 51(1979)481-484.
4. CHAPNICK, J. S. and BACH, M. C. Bacterial and fungal infections of the maxillary sinus. Otolaryngol. Clin. North Am. 9(1976)43-54.
5. HAUHNAR, C. Z., KAUR, S., SHARMA, V. K. and MANN, S. B. S. A clinical and radiological study of the maxillary antrum in lepromatous leprosy. Indian J. Lepr. 64(1992)487-494.
6. HAUHNAR, C. Z., MANN, S. B. S., SHARMA, V. K... MEHTA, S. and RADOTA, B. D. Maxillary antrum involvement in multibacillary leprosy: a radiological, sinuscopic and histological assessment. Int. J. Lepr. 60(1992)390-395.
7. HICKISH, G. W. Ear, Nose and Throat Disorders. London: Churchill Livingstone, 1985.
8. JOB, C. K., KARAT, A. B. A. and KARAT, S. The histopathological appearance of leprous rhinitis and pathogenesis of septal perforation in leprosy. J. Laryngol. 80(1966)718-732.
9. JOPLING, W. H. and MCDOUGALL, A. C. Handbook of Leprosy. 4th cd. Oxford: Heinemann, 1988.
10. KAUR, S., MALIK, S. K., KUMAR, B., SINGH, M. P. and CHAKRAVATY, R. N. Respiratory system in volvement in leprosy. Int. J. Lepr. 47(1979)18-25.
11. LEWIS, M., ROBERTS, C. A. and MANCHESTER, K. Inflammatory bone changes in the leprous skeletons from the medieval hospital of St. James and St. Mary Magdalene, Chichester, England. Int. J. Lepr. 63(1995)77-85.
12. MAGILTON, J. and LEE, F. The leper hospital of St. James and St. Mary Magdalene, Chichester. In: Burial Archaeology: Current Research Methods and Developments. Roberts, C. A., Lee, F. and Bintliflf, cds. Oxford: British Archaeological Reports, 1989, pp. 249-265. British Series 211.
13. M ARAN, A. An Integrated System of Study. Vol. 4 Otorhinolaryngology. Boston: MTP Press, 1989.
14. MOLLER-CHRISTENSEN, V. Hone Changes in Leprosy. Copenhagen: Munksgaard, 1961.
15. NORLANDER, T., FORSGEN, K., KUMLIEN, J., STI-ERNA, P. and CARSLOO, B. Cellular regeneration and recovery of the maxillary sinus mucosa: an experimental study in rabbits. Acta Otolaryngol. (Stockholm) Suppl. 492(1992)33-37.
16. SONI, N. K. Radiological study of the paranasal sinuses in lepromatous leprosy. Indian J. Lepr. 60(1988)285-289.
17. SONI, N. K. Antroscopic study of the maxillary antrum in lepromatous leprosy. J. Laryngol. Otol. 103(1989)502-503.
18. VON BUCHNER, J. H. and LESSEL, W . Uber Knochenveranderungen bei chronischen odontogenen kieferhoflenentzundungen. Stomatol. DDR 28(1978)883-887.
19. WRIGHT, D. Acute sinusitis. In: Scott-Brown's Diseases of the Ear, Nose and Throat. Volume J. 4th edn. Ballantyne, J. and Groves, J., cds. London: Butterworths, 1979, pp. 243-271.
1. M.Sc; Calvin Wells Laboratory, Department of Archaelogical Sciences, University of Bradford, Bradford BD7 1DP, U.K.
2. Ph.D.; Calvin Wells Laboratory, Department of Archaelogical Sciences, University of Bradford, Bradford BD7 1DP, U.K.
3. D.Sc; Calvin Wells Laboratory, Department of Archaelogical Sciences, University of Bradford, Bradford BD7 1DP, U.K.
Reprint requests to Dr. Charlotte Roberts.
Received for publication on 22 November 1994.
Accepted for publication on 16 December 1994.