- Volume 63 , Number 2
- Page: 213–21
Long-term effect of leprosy control in two prefectures of China, 1955-19931
ABSTRACT
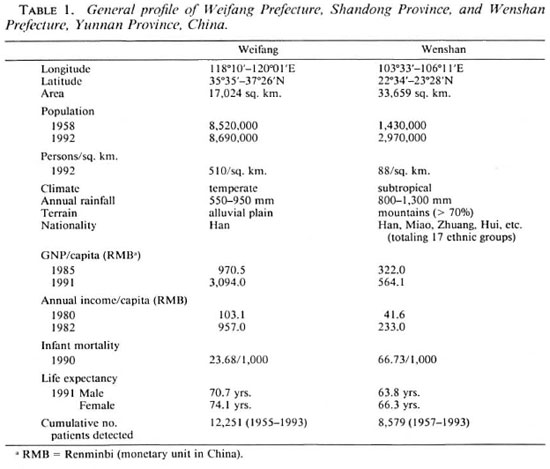
In Weifang Prefecture, Shandong Province, and Wenshan Prefecture, Yunnan Province of China, leprosy was highly prevalent in the 1950s. Due to differences in geographical conditions and socioeconomic development, the decline in leprosy prevalence between 1955 and 1993 was 99.5% (10.1 to 0.05/10,000) in Weifang and 93.9% (19.7 to 1.2/10,000) in Wenshan. The decrease in the detection rate was 99.9% (35.2 to 0.05/10,000) in Weifang and 91.7% (69.9 to 5.8/10,000) in Wenshan. The decrease was more apparent in these two prefectures since the implementation of multidrug therapy (MDT) in 1986. Findings such as specific detection rates by age, sex and type, as well as the multibacillary, child, and deformity rates of patients detected since 1980 were studied. Using the detection and prevalence rates between 1980 and 1993, the number of patients until the year 2000 is extrapolated for these two prefectures.RÉSUMÉ
La lèpre était hautement prevalente dans la Préfecture de Weifang, Province de Shandong, et la Préfecture de Wenshan, Province de Yunnan, en Chine, dans les années 1950. Par le fait de differences de conditions géographiques et de développement socio-économique, la diminution de la prevalence de la lèpre entre 1955 et 1993 fut de 99.5% (10.1 à 0.05/10,000) à Weifang et de 93.9% (19.7 à 1.2/10,000) à Wenshan. La diminution de la prevalence était plus évidente dans ces deux préfectures depuis l'introduction de la polychimiothérapie (PCT)en 1986. On a étudié des facteurs tels que les taux de détection spécifiques pour l'âge, le sexe et le type de lèpre, ainsi que les proportions de multibacillaires, d'enfants et d'incapacités parmi les les patients détectés depuis 1980. On a, à partir des taux de détection et de prevalence, extrapolé pour ces deux préfectures le nombre de patients jusqu'à l'an 2000.RESUMEN
La lepra fue altamente prevalente en los años 1950s en las Prefecturas de Weifang, Shandong y Wenshan, de la provincia de Yunnan, China. Debido a los cambios en las condiciones geográficas de la zona y al desarrollo socioeconómico de la población, entre 1955 y 1993 la lepra disminuyó en un 99.5% (10.1 a 0.05/ 10,000) en Weifang y en un 93.9% (19.7 a 1.2/10,000) en Wenshan. La disminución en la frecuencia de detección de casos fue del 99.9% (35.2 a 0.05/10,000) en Weifang y del 91.7% (69.9 a 5.8/10,000) en Wenshan. Lo anterior resultó más aparente desde que en las dos prefecturas se implemento la poliquimioterapia(PQT), en 1986. En el presente estudio se analizaron las frecuencias de detección por edad, sexo y tipo de lepra, la multibacilaridad, el tamaño de la progenie, y la frecuencia y grado de deformidad de los pacientes detectados desde 1980. Usando las frecuencias de detección y prevalência entre 1980 y 1993, en el estudio se hace una extrapolación del número de pacientes que habrá en el año 2000 en estas dos prefecturas.It is well known that leprosy has an uneven distribution and its prevalence is associated with the socioeconomic development of the area concerned. China is a country of 9.6 million sq. km. with a wide range of geographical conditions. Its 1.12 billion population consists of 56 ethnic groups of which 96% are Han. Besides Mongolians in the north, Uyur in the northwest and Tibetans on the high Himalayan Plateau, the other divergent ethnic minorities live mostly in the mountainous areas of the southwestern provinces. Taking these into consideration, China set a two-tier objective at the 1981 Second National Leprosy Conference in Guangzhou: to eliminate leprosy (prevalence < 0.1/10,000/county) from at least 95% of its 2510 counties by the end of this century.
This paper compares the prevalence and detection rates since 1955 plus the features of new patients detected after 35 years of control (1980-1993) in two prefectures of widely divergent geographical conditions and socioeconomic development. The prevalence and detection rates until the year 2000 are extrapolated with the purpose that appropriate measures be taken to meet the national goal by year 2000.
MATERIALS AND METHODS
Weifang Prefecture, situated on the alluvial plain of the Yellow River in the Shandong Peninsula, consists of 10 counties. The effects of 25 years of intensive control have been reviewed previously (3). Wenshan Prefecture of Yunnan Province, one of the 30 autonomous prefectures established within the country, borders on Vietnam and has eight counties. Besides Han, Zhuang and Miao there are a total of 17 different ethnic groups living in this subtropical, landlocked, mountainous area. Although leprosy control as part of the national program was initiated in the late 1950s, organized control only began 10 years later when the Prefectural Institute of Dermatology was established (Fig. 1; Table 1).
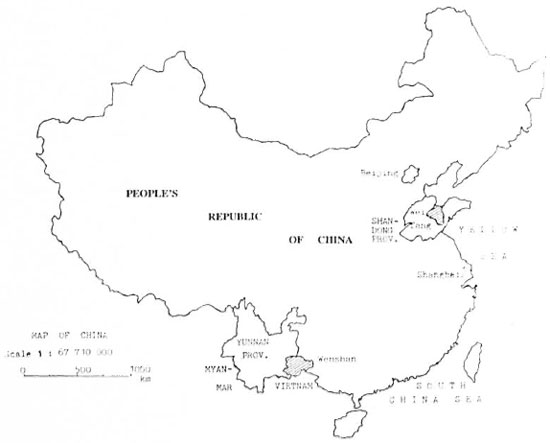
Fig. 1. Map of the People's Republic of China.
Measures of control were mainly clue survey plus contact tracing followed by institutionalized dapsone monotherapy until clinical cure (clinical, histopathology and smear negative) plus 2-5 years of maintenance therapy with dapsone. In clue surveys, the 10 major symptoms of leprosy plus methods of case finding were taught in 2-3 days to the primary health workers of the township health center and the village clinics under its administration. In addition to health education on leprosy, the major leprosy symptoms also were made widely known to the public in the villages concerned. All suspects were examined clinically and smears taken for acid-fast bacilli (AFB) by experienced leprosy workers and technicians and were further confirmed by histopathology (3,5).
China followed the Madrid classification until 1970, but the Ridley-Jopling classification has since been adopted of which borderline (B) and LL-BL-BB are classified as multibacillary (MB) for the present study.
Rifampin plus dapsone was introduced in 1979 and substituted by multidrug therapy (MDT) in 1986. Weifang treated all patients with MDT until smear negative; Wenshan adopted the fixed duration regimen [MB 24/ 36, paucibacillary (PB) 6/9 months] (11).
RESULTS
Prevalence
Prevalence was highest in 1960 for Weifang (10.1/10,000) and in 1973 for Wenshan (19.7/10,000). In Weifang prevalence declined gradually through reduction of reservoir of infection by repeated systematic clue surveys (1965, 1971, 1975 and 1983) and the treatment of all confirmed cases with dapsone until smear negative as well as decreases due to death, lost to follow up, etc. There was a sharp decline from 1985 (0.05/ 10,000; 395 patients) to 1986 (0.02/10,000; 15 patients) due to screening of old patients for MDT and deleting from the registry those who were declared clinically cured.
In Wenshan, on the other hand, prevalence remained at about 18.0/10,000 through 1979, when rifampin plus dapsone therapy was introduced, and declined further after the implementation of fixed duration MDT, from 0.49/10,000 in 1985 (1335 patients) to 0.27/10,000 in 1986 (763 patients). Although patients completing 624 months of MDT were not counted any more as patients, prevalence again remained at about 1.0/10,000 between 1988-1993 while annual input of about 150 new patients, presumably from individuals infected before MDT, remains steady (Fig. 2).
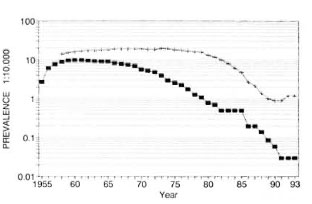
Fig. 2. Registered leprosy prevalence in Weifangand Wenshan Prefectures of China, 1955-1993. ■=Weifang; + = Wenshan.
Case detection
Before the implementation of MDT, Weifang already had kept leprosy under control, reducing the detection rate from 35.23/100,000 in 1956 to 0.66/100,000 in 1985; decreasing further with MDT (0.05/ 100,000 in 1993), reflecting the reduction of transmission since the 1960s.
In the late 1950s Wenshan placed more effort on case finding which caused the sharp decline between 1957-1961, but in the following 10 years the detection rate remained at lOto 15/100,000. With the establishment of a network of eight county skin disease control stations in 1973 and the introduction of rifampin plus dapsone therapy in 1979, improved case finding activities plus cure and deleting from the registries due topatients lost to follow up and deaths causedthe drop in the two following years (1974-1975 and 1979-1980); thereafter, however,it remained at about 5/100,000 (Fig. 3).
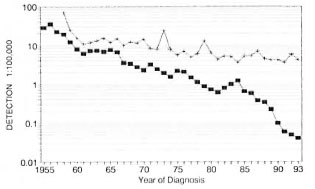
Fig. 3. Leprosy detection rates in Weifang andWenshan Prefectures of China, 1955-1993.■= Weifang; + = Wenshan.
The prevalence and case detection ratesin Weifang already coincide with each otherbetween 1975 and 1981. With the more vig-orous case finding in the 1980s, the rate of decline was also similar. In Wenshan these two rates declined very slowly until 1986. After the implementation of fixed duration MDT (l0), the annual relative decline of prevalence increased from 4.7% (1960-1985) to 18.2% (1986-1992) (Table 2); whereas the detection rate remained unchanged.

Features of new patients detected
Type-, age- and sex-specific rates. In Wenshan the detection rate was lower in females in both MB and PB types of leprosy. The peak of detection was in the 30-39 agegroup for males. For females, it was in the20-29 age group for MB and between 20-49 years for PB patients. In females proportionally more cases were detected between the age of 20-49 years, which be-speaks the proneness to leprosy during childbearing age, and more for MB leprosy. The type-, age- and sex-specific detection rates in Wenshan, compared with the findings reported by Lechat (2), shifted toward the older age groups, reflecting the delay in case detection. But the decline in the general trend of leprosy in China may also play a role (Fig. 4, a and b).
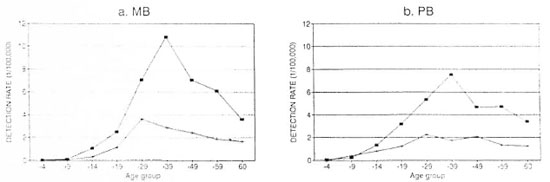
Fig. 4. Detection rates of leprosy by sex, age and type in Wenshan Prefecture, China, 1980-1993. ■= Males;+ = females.
MB rate. In Weifang, the MB rate was 53% in 1982, decreasing to 44% in 1984, and then increasing steadily to 80% in 1991 and 1993, representing only 4-5 patients detected each year. Although Wenshan generally also has shown a rising MB rate, this increase was less marked and appeared with less regularity (Fig. 5).
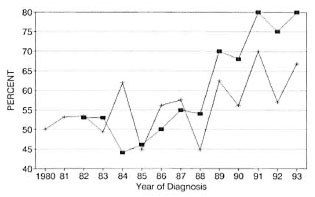
Fig. 5. Multibacillary rates at diagnosis. ■= Weifang; + = Wenshan.
Deformity rate. Visible deformity (10) was consistantly high for the patients detected each year in Wenshan; in Weifang it varied between 0% and 32% in the last 5 years, representing the few patients detected each year (6/10, 1/9, 0/5, 1/4 and 1/5 in the successive years between 1989 and 1993). They were most likely the last few patients who had escaped detection in the past (Fig. 6).

Fig. 6. Percentages of deformities in cases detectedin Weifang and Wenshan Prefectures, China. = ■ Wei-fang; + = Wenshan.
Child rate. In Weifang no children < 15 years old were detected in the last 8 years due to interruption of transmission several decades ago, as mentioned above, and in Wenshan this figure varied between 4%-9% (Fig. 7). In 1985, a survey of 228,057 (a survey of 47.5% of the total population of children) 4 to 15-year-old children detected only 3 patients (one each of indeterminate, TT and BT; 1.3/100,000) (unpublished data). This low figure is likely due to local leprosy workers missing early cases.
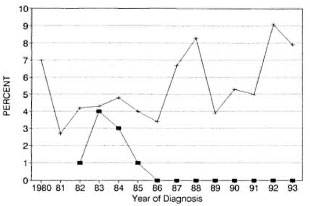
Fig. 7. Percentages of children with detected leprosy. ■= Weifang; + = Wenshan.
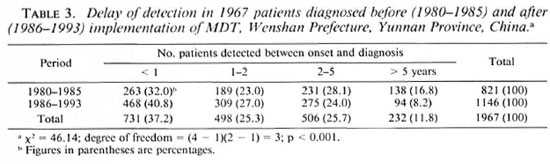
Detection at the year of onset. The increased early detection since MDT implementation in Wenshan is highly significant (Table 3); it fluctuated widely in Weifang, again due to the small number of patients detected each year.
Voluntary reporting. There was an increasing discrepancy in the proportion of voluntary reporting by patients between these two prefectures. In Weifang voluntary reporting increased to 100% in 1991 and 1993; in Wenshan it increased from 22% in 1982 to 60% in 1986 and, after a decrease to 49% in 1987 and an increase to 55% in 1990, has been falling rather rapidly in the last 3 years (Fig. 8).
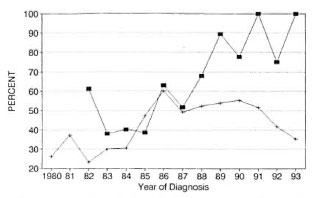
Fig. 8. Percentages of those reporting voluntarilyin newly diagnosed leprosy. ■ = Weifang; + = Wenshan.
Socioeconomic development
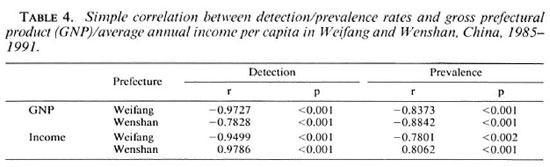
With the reform and open-door policy in China since 1978, Weifang has experienced a rapid growth of average annual income (AIC) and gross prefectural product per capita (GNP) since 1985 (increase of 9.3-fold and 3.2-fold, respectively). In Wenshan, however, the economic development has been rather slow (increase of GNP 5.6-fold and AIC 1.75-fold) (Fig. 9, a and b). The negative correlations between the growth of GNP with the detection and prevalence rates of leprosy are highly significant for both prefectures. However, there is a negative correlation of these rates with AIC in Weifang and a positive correlation in Wenshan. This is likely due to the increased control activities in Wenshan since the implementation of MDT in 1986 (Table 4).
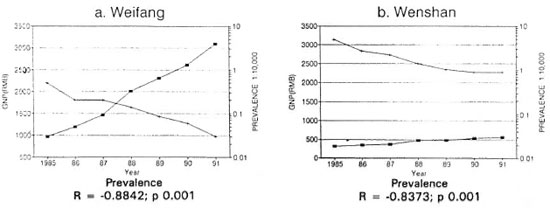
Fig. 9. Correlation between gross prefectural product (GNP) and leprosy prevalence, 1985-1991. ■= GNP[RMB (renminbi = monetary unit in China)]; + = prevalence.
Prediction of leprosy trend
Comparing with the grey dynamic (improved exponential) (9) and linear regression models, it was found that the geometric progression method can reflect the epidemiological trend more satisfactorily. Using the data of detection and prevalence rates of these two prefectures for the period between 1986 and 1993, the number of patients in the coming years was extrapolated. It was found that by year 2000, Weifang may detect only one patient and will have six patients undergoing MDT. Based upon the estimated population by the year 2000, the detection rate will be 0.13/100,000; the prevalence rate, 0.008/10,000. Wenshan may detect 100 new patients and 106 patients may still be undergoing therapy, giving a detection rate of 2.98/100,000 and a prevalence rate of0.32/10,000 by year 2000 (Fig. 10, a and b).

Fig. 10. Numbers of cases detected and prevalence in Weifang and Wenshan Prefectures, China, 1986-2000. ■ = Detection; + = prevalence.
DISCUSSION
Leprosy control was launched in China in the mid-1950s with dapsone monotherapy until clinical cure plus prolonged maintenance therapy. Leprosy was prevalent and more effectively controlled in the provinces along the coast, but the economically lessdeveloped provinces in the southwest were lagging behind. Since the introduction of MDT in 1986, Wenshan Prefecture (based upon the experiences gained at Menla County, Yunnan Province since 1983 4,5) adopted the fixed-duration regimen and Weifang Prefecture treated all patients until smear negative according to the standards set at the 1982 National Leprosy Technical Conference in Nanjing (5). Therefore, the study of the effects of control in these two prefectures has nationwide implications. After 10 years of control there has been a markedly downward prevalence trend in Weifang since 1965 through effective case finding and treating all patients with dapsone until clinical cure. In Wenshan, on the other hand, the downward trend began only in 1979, when rifampin plus dapsone was introduced, and took momentum since 1985, when 572 old cases were screened for MDT and removed from the registry.
In Weifang, the detection and prevalence rates were already close to the elimination level when MDT was introduced. With the continued control efforts, these two rates were almost identical (a difference of 1:10) from 1975 until 1981. Case finding again was intensified following the declaration of the basic elimination in November 1981; hence, the rising detection rate between 1981-1984 and, correspondingly, no decrease of prevalence during this period. Since 1985 with the declining detection numbers and increasing number of patients cured, these two rates again were clearly together.
In Wenshan, due to the underdetection and the treatment of patients until clinical cure, there were proportionally more patients on the registry, the number of whom declined sharply with the shortened period of therapy and having been deleted from registries as cured since 1986 (l0). The detection rate remained constant; thus causing the increasing difference between detection and prevalence rates.
It is well known that leprosy prevalence is associated with socioeconomic development (1, 7,8, 12), and the effectiveness of control depends upon communication facilities and input from the health services. The difference in the socioeconomic growth and prevalence rates in Weifang increased more than in Wenshan with the open-door policy and market reform since 1985.
From the features of new patients detected since 1980, Weifang's MB rate rose faster than Wenshan's and no more children < 15 years old were detected since 1986. It may be noted that Weifang already has kept the infection and spread of leprosy under control. In Wenshan the detection rate is still high and, in conjunction with the high child and deformity rates plus the decreasing rate of voluntary reporting, more effortin case finding and health education activ-ities is urgently required. Perhaps the ex-isting rural health system should be up-graded and more fully utilized.
A previous study of age at onset by yearof birth in Shandong indicated continueddeclining age-specific incidence rates formales and females for the cohorts from1920-1929 to 1950-1959 (3). A continuedanalysis of the succeeding cohorts for 1960-1969 showed a similar trend (Fig. 11, a andb) (unpublished data). As Weifang consti-tutes about 1/10 of Shandong's total pop-ulation (8,640,000/84,393,000 = 9.77%;1991) and about 1/4 of Shandong's cumu-lative number of leprosy patients (12,251/53,328 = 22.97%; 1955-1993), it may besaid that the decline in the age-specific in-cidence in the succeeding cohorts of Shan-dong Province is also applicable for Wei-fang Prefecture.
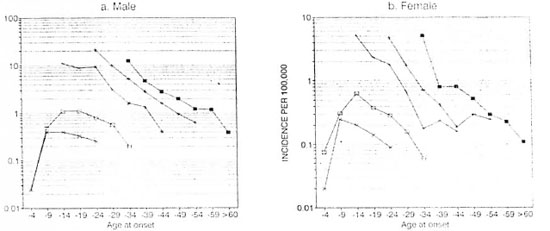
Fig. 11. Age-specific incidence of leprosy by year of birth and sex, Shandong Province, China, 1920-1969.Cohorts and number of patients in each cohort by sex: ■ = 1920-1929 (M = 2009, F = 649); + = 1930-1939(M = 3610, F = 706); * = 1940-1949 (M = 3153, F = 114); □ = 1950-1959 (M = 905, F = 400); x = 1960-1969 (M = 346, F = 177).
The protective effect of BCG vaccinationagainst leprosy was reported to vary be-tween 23% (Chengalpattu, India) to 80%(Uganda). A case-control study in TamilNadu, India, suggested that BCG increased the risk for indeterminate leprosy but wasprotective against the more severe forms (6).Shandong Province initiated BCG vacci-nation in the 1970s, reaching 90% coveragein newborns and schoolchildren in 1990.Since the detection was generally low inchildren and high in adults, with the knownlow detection in indeterminate leprosy, BCGapparently also has played some role in thereduction of morbidity of leprosy. On theother hand, BCG coverage in Yunnan Prov-ince is low in children (52.3%, 1992). BCGvaccination, like other health programs, ishampered by the difficult terrain and lowsocioeconomic development.
Although regularity of MDT was high (>98%) once the patients were detected, othercontrol activities such as surveillance anddisability prevention require continued at-tention in the management of the program.
It is estimated that Weifang may detect 1patient and have 6 patients under therapyby the year 2000 and in Wenshan these fig-ures will be 100 and 106, respectively. Asindicated by WHO, with a high coverage ofMDT the detection/incidence and preva-lence rates will approximate each other by the end of this century (13). Shandong already had reached the elimination goal in all of its 104 counties (inclusive of the 10 counties of Weifang) in May 1994. It is expected that the two most prevalent counties of Wenshan (prevalence 1.3-1.6/10,000) also may meet the national goal of elimination in the early part of the next century, if the present trend of detection continues.
There are more counties, such as those in Wenshan, in the outlying mountainous areas of the country. Only 5-6 years are left for us to reach the elimination target. At the International Conference on Elimination of Leprosy (Hanoi, 4-7 July 1994), the participating countries recommended the implementation of the Global Plan of Action for Health Problem by the Year 2000. It is high time for us to identify such areas and bring the benefit of cure to all persons afflicted with leprosy and to prevent them from becoming disabled.
Acknowledgment. The leprosy control program withmultidrug therapy in Shandong Province is supported by the Sasakawa Memorial Health Foundation; in Wenshan, by the World Health Organization. We are thankful for the assistance in the statistical analysis of data by Dr. Yang Zhong-Min, Associate Professor, Cancer Research Institute. Chinese Academy of Medical Sciences, Beijing, and extend our sincere gratitude to Prof. M. Lechat for his valuable comments.
REFERENCES
1. IRGENS, L. M. Leprosy in Norway. Lepr. Rev. 51 Suppl.(1980)1-130
2. LECHAT, M. F. and VANDERVEKEN, M. Basic epidemiological indicators for monitoring leprosy control. In: Proceedings 4th International Workshop on Leprosy Control in Asia. Tokyo: Sasakawa Memorial Health Foundation, 1983, pp. 42-65.
3. LI, H.-Y., PAN, Y.-L. and WANG. Y. Leprosy con trol in Shandong Province, China 1955-1983, some epidemiological features. Int. J. Lepr. 53(1985)79-85.
4. Li, H.-Y., YU. X.-L. and HUANG, W.-B. Eight years follow up of multibacillary leprosy after 2427 months of multidrug therapy. Int. J. Lepr. 61 Suppl. (1993) 5A.
5. Li, H.-Y., Yu, L., ZHANG, M.-S., DUAN, C.-X., HUANG, W.-B., ZHANG, S.-B., ZHU, K. and MA, J.-F. Short-term multidrug therapy in multiba cillary leprosy-review of 80 cases in two provinces of China (1983-1988). Int. J. Lepr. 57(1989)622-627.
6. MULIYIL, J., NELSON, E. K. and DIAMOND, E. L. Effect of BCG on the risk of leprosy in an endemic area: a case control study. Int. J. Lepr. 59(1991)229-236.
7. SAIKAWA, K. The effect of rapid socio-economic development on the frequency of leprosy in a population. Lepr. Rev. 52 Suppl. 1(1981)167-175.
8. SOMMERFELT, H., IRGENS, L. M. and CHRISTIAN, M. Geographical variations in the occurrence of leprosy: possible roles played by nutrition and some other environmental factors. Int. J. Lepr. 53(1985)524-532.
9. WANG, A.-Q. and Yu, M. Use of grey dynamic model in the prediction of mortality of diseases. Chin. J. Epid. 9(1988)47-52.
10. WHO EXPERT COMMITTEE O N LEPROSY. Sixth report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
11. WHO STUDY GROUP. Chemotherapy of leprosy for control programs. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
12. WORLD HEALTH ORGANIZATION. Global strategy for the elimination of leprosy as a public health problem. Geneva: World Health Organization, 1994. WHO/CTD/LEP/94.2.
13. ZHAO, D., WONG, Y. W. and ZHONG, J. Z. The relationship between leprosy incidence and economic development. China Lepr. J.9(1993)145-147.
1. M.D., M.P.H., Senior Researcher, Beijing Tropical Medicine Research Institute, 95 Yun An Lu, Beijing, China.
2. M.D., Assistant Researcher, Beijing Tropical Medicine Research Institute, 95 Yun An Lu, Beijing, China.
3. Technician, Beijing Tropical Medicine Research Institute, 95 Yun An Lu, Beijing, China.
4. Director, Weifang Prefectural Institute of Dermatology, Shandong Province, China.
5. Statistician, Weifang Prefectural Institute of Dermatology, Shandong Province, China.
6. Director, Wenshan Prefectural Institute of Dermatology.
7. Deputy Director, Yunnan Provincial Institute of Dermatology.
Received for publication on 15 October 1994;
Accepted for publication in revised form on 16 February 1995.