- Volume 63 , Number 1
- Page: 109–11
Erythema nodosum leprosum in malaysians
To the Editor:
Reactions and relapses in leprosy pose major problems in the management of the disease. A reaction is an allergic inflammatory process which is not an essential part of the infective process of leprosy. Reactions which occur in the multibacillary type of leprosy are erythema nodosum leprosum (ENL), exacerbation reactions, the Lucio reaction, and reversal or upgrading reaction (1). Clinically, it is difficult to differentiate reactions from relapse. Microscopic examination of the lesion is very useful for the proper diagnosis. This study documents the histological features of ENL with clinical correlation in Malaysian patients.
Skin biopsies from leprosy patients sent to the Institute of Medical Research, Kuala Lumpur, Malaysia, during the period between January 1988 and December 1992 were reviewed. Sections cut from paraffinembedded material were stained with hematoxylin and eosin (H&E) and Fite's stain for acid-fast bacilli (AFB). In addition, Martius' scarlet blue stain for fibrin and immunohistochemical stains were performed in suspected cases of ENL. Specifically, the immunoperoxidase method of Sternberger (10) was applied with modification. Antisera were obtained from Dakopatts and included immunoglobulin IgG and complement component C3. The diagnosis was based on the criteria of Ridley and Jopling (7).
A total of 189 biopsies from suspected leprosy patients were reviewed. The histological diagnosis was tuberculoid leprosy (TT) 5 cases, borderline tuberculoid leprosy (BT) 38 cases, borderline leprosy (BB) 2 cases, borderline lepromatous leprosy (BL) 49 cases, and lepromatous leprosy (LL) 95 cases. The features of ENL were observed in 6 LL patients and 1 BL patient. These patients were composed of 6 males and 1 female. The age range was between 19 to 32 years. All 7 patients with ENL presented with tender nodules, 5 of the 7 having concomitant fever. Two patients had edema of the legs. All 7 patients except one had received antileprosy therapy consisting of multiple drug therapy (5 cases) and dapsone (1 case).
Histology showed infiltration of the granulomas by neutrophils in all cases (The Figure). The interstitium also showed minimal infiltration of neutrophils in all cases. The primary site of inflammation was mainly in the dermis in 6 cases, with extension of inflammation into the subcutaneous fat in 2 cases. Mild edema of the upper dermis was observed in 2 cases. Vasculitis involving a medium sized vein in the dermis was noted in 1 case. None of the cases had ulceration of the skin. Acid-fast stain revealed a few highly fragmented AFB in 1 case. Immunocytochemical stains did not show deposits of IgG or complement in any of the cases.
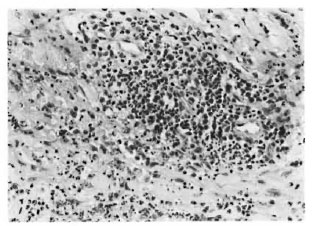
The figure. Erythema nodosum leprosum showing infiltration of the granuloma by neutrophils (H&E x 500).
ENL is a known complication occurring in patients with multibacillary (MB) leprosy, and it is one of the most common type of reactions in leprosy (2). ENL usually occurs after the commencement of chemotherapy (1) but sometimes it can develop prior to any medication. (5).
In our study, the histological diagnosis of ENL was made in 4.8% (7/146 cases) of MB leprosy. Some of the histologic features noted in our study, such as inflammatory reaction with predominant involvement of the upper dermis, absence of ulceration and low incidence of vasculitis are similar to those seen in Malaysian patients in the previous report by Ridley, et al. (8). In that study, the workers noted well-developed edema in the dermis. In contrast, in our study subepidermal edema was noted only in 2 (28.5%) cases and it was mild in both. In Mexican patients, the primary site of inflammation was mainly in the deep dermis and subcutis in 15/18 cases (83.3%). In Singapore, biopsies of patients with ENL showed four patterns: classic, subepidermal bulla or edema, vasculitis, and nonspecific change. Subepidermal bulla with upper dermal edema was the predominant pattern (3).
The etiology of ENL is uncertain. There are two hypotheses regarding the pathogenesis of ENL. Modlin, et al. (4) proposed that the cell-mediated immune response plays an important role in ENL pathogenesis based on a study of the subsets of T lymphocytes in LL patients with and without ENL. They noted a high ratio of helper-suppressor cells in ENL tissue and low ratio in LL patients without ENL.
Wemambu, et al. (11) observed deposits of complement components and immunoglobulin in the vessel walls of an ENL lesion, and suggested that ENL is a manifestation of the Arthus phenomenon. Ridley and Ridley (10) observed deposits of bacterial antigen, immunoglobulin IgG, IgM, and complement components at the site of ENL lesions. These deposits were seen extracellularly and intraccllularly in the neutrophils and degenerating macrophages. They concluded that ENL is an immune complex phenomenon, but differs from the classic serum sickness because the immune complexes are extravascular. In our study there were no deposits of complement or immunoglobulin.
- P . Jayalakshmi, M.Path., M.R.C.Path.
Associate Professor
Department of Pathology
Faculty of Medicine
University of Malaya
59100 Kuala Lumpur, Malaysia
Member, Leprosy Research Committee, Malaysia
- T . Ganesapillai, F.R.A.C.P., F.A.A.D. (U.S.A.)
Chief Consultant Dermatologist
General Hospital
Kuala Lumpur, Malaysia
Technical Advisor, Leprosy Research Committee, Malaysia
- J . Ganesan, F.R.C.P.A.
Institute of Medical Research
Kuala Lumpur, Malaysia
Member, Leprosy Research Committee, Malaysia
REFERENCES
1. BROWNE, S. G. Erythema nodosum in leprosy. J. Chronic Dis. 16(1963)23-30.
2. CHOPRA, N. K.. AGARWAL, J. S. and PANDHYA, P. G. Reactions in leprosy, a study of 250 patients in a multidrug therapy project, Baroda district, Gujart, India. Int. J. Dermatol. 29(1990)490-493.
3. GIAM, Y. C, ONG, B. H. and TAN, T. Erythema nodosum leprosum in Singapore. Ann. Acad. Med. Singapore 16(1987)658-662.
4. MODLIN, R. L.. BAKKE. A. L., VACCARO. S. E.. HORWITZ, D. A., TAYLOR, C. R. and REA, T. H. Tissue and blood T lymphocyte subpopulations in erythema nodosum leprosum. Arch. Dermatol. 121(1985)206-209.
5. REA, T. H. and RIDLEY, D. S. Lucio's phenomenon: a comparative histological study. Int. J. Lepr. 47(1979)161-168.
6. RIDLEY, D. S. Skin Biopsy in Leprosy: Histological Interpretation and Clinical Application. 3rd edn. Basle: Documcnta Gcigy, 1990.
7. RIDLEY, D. S. and JOPLING, W. H. Classification of leprosy according to immunity; a five-group system. Int. J. Lepr. 34(1966)255-273.
8. RIDLEY, D. S., REA, T. H. and MCADAM, K. P. W. The histology of erythema nodosum leprosum: variant forms in New Guineans and other ethnic groups. Lepr. Rev. 52(1981)65-78.
9. RIDLEY, D. S. and RIDLEY, M. J. The immunopathology of erythema nodosum leprosum: the role of extra vascular complexes. Lepr. Rev. 54(1983)95-107.
10. STERNBERGER, L. A., HARDY, P. H., Jr., CUCULIS, J. J. and MEYER. H. G. The unlabelled antibody enzyme method immunohistochemistry. J- Histochem. Cytochcm. 18(1970)315-333.
11. WEMAMBU, S. N. C, TURK., J. L., WATERS, M. R. F. and REES, R. J. W. Erythema nodosum leprosum; a clinical manifestation of the Arthus phenomenon. Lancet 2(1969)933-935.