- Volume 63 , Number 1
- Page: 111–3
Follicular keratoses in leprosy and post-kala-azar dermal leishmaniasis
To the Editor:
The term "follicular keratoses" refers to a group of varied etiology in all of which there is a prominent plug of keratin in the follicular orifice (1). Keratosis pilaris, keratosis pilaris atrophicans, keratosis circumscripta, phrynoderma, lichen spinulosa, follicular ichthyosis, to name a few, are the disorders in which this pathology is prominently seen (1). In most of these disorders, the exact cause of keratinization is unclear. In some the type of keratitis is abnormal, in others the shedding mechanism or the rate of production is at fault. The histopathological changes are distinctive in a few instances, but often the morphological differences are more striking.
Many inflammatory conditions of the skin tend to develop a follicular keratosis. Two types of follicular keratoses, keratosis spinulosa (7) and comedo (5) have been described over the lesions of borderline tuberculoid (BT) leprosy. We report such lesions in three patients, one each with borderline lepromatous (BL), lepromatous leprosy (LL) and post-kala-azar dermal leishmaniasis (PKDL).
Case 1. A 45-year-old woman with polar lepromatous leprosy (LLp), with a bacterial index of 4+ and a morphological index of 1%, was receiving the World Health Organization multibacillary multidrug regimen (WHO-MDT-MBR). During her sixth monthly follow up, multiple, 1- to 3-mm keratotic pigmented papules with follicular atrophy at places were seen over some of the infiltrated plaques present on her forearms and legs.
Case 2. A 33-year-old man suffering from borderline lepromatous (BL) leprosy for the last 3 years presented in one of the episodes of type 1 lepra reaction. There were multiple, hyperkeratotic, pigmented follicular papules over a few of the erythematous infiltrated plaques on his back. No follicular scarring or atrophy was appreciated. According to patient's history the keratotic lesions became more prominent during each reactional episode.
Case 3. A 20-year-old man, migrant from Bihar, was diagnosed as having PKDL for the last 3 years. A few of the infiltrated plaques over his neck, axillae and back were studded with multiple, pigmented, keratotic follicular lesions without any scaling or atrophy of the follicular orifices (The Figure).
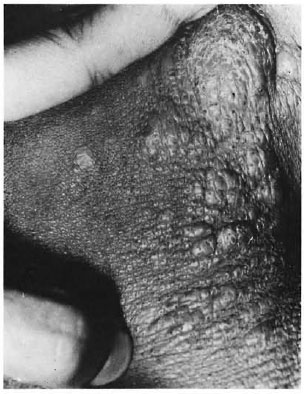
The figure. Close up of right axilla showing multiple pigmented keratotic follicular lesions.
In all three patients the follicular papules were limited strictly to the lesions only. There was no history of similar keratotic follicular lesions in other family members in any of the three patients. Neither was there any personal or family history of atopy. None of the patients had a history of massaging oil over the lesions. There was no evidence of a deficiency state in any of the patients. Histopathological examinations of the skin of all three patients showed follicular hyperkeratosis, keratotic plugging and sparse inflammatory infiltrate around the hair follicles. There was a gradual disappearance of these follicular keratotic lesions during specific treatment of the disease and subsequent follow up.
In an earlier report, comedo-like lesions over infiltrated plaques of borderline tuberculoid (BT) leprosy were attributed to coconut oil massage (5). This history was absent in all of our patients, he keratotic papules were seen only in a few infiltrated plaques in Cases 2 and 3, while in Case 1 more extensive involvement of the infiltrated areas was observed.
The prominence of the keratotic lesions during type 1 lepra reaction in Case 2 suggests that it could be the manifestation of an immunological reaction in the skin, type 1 reaction being a delayed type hypersensitivity (DTH) reaction (2). While investigating the role of delayed immune reactions of human epidermal keratinocytes, Kaplan, et al. (3) observed that during DTH reaction, there is marked thickening of the epidermis associated with an increase in the both size and number of keratinocytes and in the expression of keratinocytic-Ia antigen in the epidermis. They further suggested that one or more epidermal growth factors may be generated in the course of a delayed immune reaction in the dermis. Thangaraj, et al. (6) demonstrated significant epidermal changes in lesions of leprosy patients undergoing type 1 reaction in the form of an increase in epidermal cell layers, the consistent presence of Ia in all keratinocytes, an increase in Langerhans' cell numbers, and scattered T cells within the epidermis. T-cell activation can lead also to the production of lymphokines, e.g., gamma interferon (IFN-γ) with subsequent induction of la on epidermal keratinocytes. All of these can lead to keratinocyte proliferation leading to follicular plugging.
In Case 1 with LLp, such keratotic papules developed after 6 doses of WHO-MDT-MBR. This could be due to the fact that after 6 months' treatment there was a gradual return of cell-mediated immunity with activation of T cells through the expression of keratinocyte-Ia antigen, resulting in follicular hyperkeratosis and keratotic plugging (6).
A similar pathomechanism can be postulated for the development of such follicular keratotic papules over infiltrated plaques of PKDL. The type of PKDL presenting mostly with infiltrated plaques and nodular lesions is thought to be due to DTH reaction to Leishmania donovani antigen (4). Therefore, follicular keratotic plugging could be a manifestation of localized keratinocyte proliferations as a result of DTH reaction having a similar immunopathological connotation as reactional leprosy. However, to the best of our knowledge, such keratotic follicular papules in relation to the plaque lesion of PKDL have not been reported earlier.
- Sandipan Dhar, M.D., D.N.B.
Senior Resident
- Inderjeet Kaur, M.D.
Associate Professor
- Vinod K. Sharma, M.D.
Associate Professor
- Bhushan Kumar, M.D., M.N.A.M.S.
Additional Professor
Department of Dermatology, Venereology and Leprology
Postgraduate Institute of Medical Education & Research
Chandigarh 160012, India
REFERENCES
1. GRIFFITHS, W. A. D., LEIGH, I. M. and MARKS, R. Disorders of keratinization. In: Textbook of Dermatology . Champion, R. H., Burton, J. L. and Ebling, F. J. G., eds. Oxford: Blackwell Scientific Publications, 1992, pp. 1352-1358.
2. JOPLING, W. H. and MCDOUGALL, A. C. Handbook of Leprosy. Oxford: Heinemann Professional Publishing, 1988.
3. KAPLAN, G., WITMER, M. D., NATH, I., STEINMAN, R. M., LAAL, S., PRASAD, H. K., SARNO, U. N., ELVERS, U. and COHN Z. A. Influence of delayed immune reactions on human epidermal keratinocytes. Proc. Natl. Acad. Sci. U.S.A. 83(1986)3469- 3473.
4. NANDY, A., NEOGY, A., GHOSH DASTIDAR, B., SARKER, M., MALLICK, K. K. and CHOWDHURY, A. B. Immune response and drug response in kala-azar and post kala-azar dermal leishmaniasis. Proceedings of the Indo-U.K. Workshop on Leishmaniasis, 1983, pp. 161-170.
5. SRINIVAS, C. R., PADHEE, A., BALCHANDRAN C., SHENOY, S. D. , ACHARYA, S. and RAMNARAYAN, K. Comedones induced by coconut oil in a borderline tuberculoid lesion. Int. J. Lepr. 56(1988)471-472.
6. THANGARAJ, H., LAAL, S., THANGARAJ, I. and NATH, I. Epidermal changes in reactional leprosy: keratinocyte-Ia expression as an indicator of cell-mediated immune responses. Int. J. Lepr. 56(1988)401-407.
7. THANKAPPAN, T. P. and SULOCHANA, G. Keratosis spinulosa developing in borderline tuberculoid lesions during type 1 reaction: two case reports. Lepr. Rev. 62(1991)49-51.
Reprint requests to Dr. B. Kumar.