- Volume 62 , Number 4
- Page: 539–46
Epidemiological studies in children of a low-endemic region, a high-endemic region, and dwellers of a leprosy colony: evaluation of anti-ND-BSA antibodies and lepromin response
ABSTRACT
Children residing in a low-endemic region (LER), a high-endemic region (HER), and a leprosy colony contact population (CP) were evaluated for lepromin response as well as reactivity to the Mycobacterium leprae specific synthetic antigen, ND-BSA. The mean reactivity to ND-BSA in the LER group (OD 0.03 ± 0.03, N = 71) was significantly lower (p < 0.001) than that in the contact population (OD 0.14 ± 0.09, N = 140) as well as the population residing in the HER (OD 0.09 ± 0.08, N = 1340). ELISA-positive results were the highest (21.4%) with the CP group and lowest (0.0%) in the LER group, suggesting that it was a measure of the extent of exposure to M. leprae. In the contact population, females showed a preponderance for ELISA positivity over males (p < 0.005), a finding not observed with the HER population. The Mitsuda responses showed a Gaussian-type distribution in all of the three populations examined with the mean response being highest in the LER (6.0 mm ± 2.9) and lowest in the HER (4.5 mm ± 2.0) groups. The percent positivity for the Mitsuda reaction was found to be highest in the LER (93.0%) and lowest in the HER (88.3%) groups. The Mitsuda response thus appears to be independent of M. leprae exposure, and its interpretation in a given population needs consideration of several factors, such as nutritional, environmental, etc. The percent positivity as well as the mean Fernandez response was found to be highest in the LER (52.1%, 5.5 ± 4.6) and lowest in the HER (24.4%, 3.1 ± 3.0) groups, indicating more of a reflection of an individual immunological response rather than a prior exposure to M. leprae. The humoral and cell-mediated immune responses (Mitsuda) in the same individual showed a poor correlation between the two in all three groups studied. However, the percent-positive ELISA results associated with lepromin-negative individuals in the CP group was significantly higher (5/12, 41.7%) than that observed in HER group (10/156, 6.4%). The clinical utility and the predictive value of the two tests along with the cost-effectiveness for the outcome of the disease need close and longer follow-up studies.RÉSUMÉ
Des enfants résidant dans une région à basse endémicité (RBE), une région à haute endémicité (RHE), et une population de contacts d'une colonie de lépreux (PC) ont été évalués quant à leur réponse à la lépromine ainsi que pour leur réactivité à Itigene synthétique ND-BSA, spécifique au Mycobacterium leprae. La réactivité moyenne au ND-BSA dans le groupe RBE (OD 0.03 ± 0.03, N = 71) était significativement plus faible (p < 0.001 ) que celle dans la population-contact (OD 0.14 ± 0.09, N = 140) ainsi que dans la population résidant dans la RHE (OD 0.09 ± 0.08, N = 1340). Us résultats positifs à l'ELISA étaient les plus élevés (21.4%) dans le groupe PC et les plus faibles (0.0%) dans le groupe RBE, suggérant qu'il s'agissait là d'une mesure du degré d'exposition au M. leprae. Parmi la population-contact, les femmes montraient une prépondérance sur les hommes quant à la positivité à l'ELISA (p < 0.005), une observation qui ne se retrouvait pas dans la population RHE.Les réponses au Mitsuda montraient une distribution de type Gaussien dans les trois populations examinées, avec la réponse moyenne la plus élevée dans le groupe RBE (6.0 mm ± 2.9) et la plus faible dans le groupe RHE (4.5 mm ± 2.0). Le pourcentage de positivite pour la réaction de Mitsuda était le plus élevé dans la RBE (93.0%) et le plus bas dans la RHE (88.3%). La réponse au Mitsuda apparaît done être indépendante de l'exposition au M. leprae, et son interprétation dans une population donnée demande de prendre différents facteurs en considération, tels que la nutrition, l'environnement, etc. Le pourcentage de positivite ainsi que la réponse de Fernandez moyenne furent trouvés les plus élevés dans la RBE (52.1%, 5.5 ± 4.6) et les plus faibles dans la RHE (24.4%, 3.1 ± 3.0), donnant plus une image d'une réponse immunologique individuelle que celle d'une exposition antérieure à M, leprae.
Les réponses immunitaires humorale et à médiation cellulaire (Mitsuda) chez la même personne montraient une faible correlation entre elles dans chacun des trois groupes étudiés. Cependant, le pourcentage de résultats ELISA positifs associés à des tests à la Iépromine négatifs était significativement plus élevé dans le groupe PC (5/12,41.7%) que celui observé dans le groupe RHE (10/156, 6.4%). L'utilité clinique et la valeur prédictive des deux tests ainsi que le rapport coût efficacité quant à l'issue de la maladie nécessitent des études de suivi plus approfondies et plus longues.
RESUMEN
Se midió la reactividad a la lepromina y al antígeno sintético ND-BSA específico del Mycobacterium leprae, en niños de dos regiones, una de baja endemia (RBE) y otra de alta endemia (RAE), y en niños contactos de pacientes con lepra (CP). La reactividad promedio contra el ND-BSA en el grupo de la RBE (DO 0.03 ± 0.03, N = 1340) fue significativamente menor (P = 0.001) que la del grupo de contactos (DO = 0.14 ± 0.09) y que la del grupo de la RAE (DO 0.09 ± 0.08, N = 1340). Los resultados positivos por ELISA fueron más altos (21.4%) en el grupo CP y más bajos (0%) en el grupo de la RBE, sugiriendo que este parámetro es una medida del grado de exposición al M. leprae. Entre la población de contactos, los pacientes femeninos mostraron mayor positividad por ELISA que los masculinos (p < 0.005), hallazo que no fue observado en la población de la RAE.Las respuestas tipo Mitsuda mostraron una distribución Gaussiana en las 3 poblaciones examinadas, siendo la respuesta promedio más alta en el grupo de la RBE (6.0 mm ± 2.9) y más baja en el grupo de la RAE (4.5 mm ± 2.0).
El porcentaje de positividad para la reacción de Mitsuda fue mayor en el grupo de la RBE (93.0%) y más baja en el grupo de la RAE (88.3%). Así, la respuesta tipo Mitsuda parece ser independiente de la exposición al M. leprae; la interpretación de esta reacción en una población dada necesita la consideración de varios factores de tipo nutricional, ambiental, etc. El porcentaje de positividad y la respuesta promedio tipo Fernández fueron mayores en el grupo de la RBE (52.1% y 5.6 mm ±4.6) y más bajos en el grupo de la RAE (24.4% y 3.1 m m ± 3.0), reflejando ésto, más una respuesta inmunológica individual que una exposición previa al M. leprae. Las respuestas inmunes humoral y celular (Mitsuda)en el mismo individuo, mostraron una pobre correlación entre si en los 3 grupos estudiados. Sin embargo, el porcentaje de resultados positivos por ELISA entre los individuos lepromino-negativos del grupo CP, fue significativamente mayor (5/12,41.7%) que el observado en el grupo de la RAE (10/156, 6.4%). La valoración de la utilidad clínica y el valor predictivo de las dos pruebas, requiere de estudios más precisos y de mayores tiempos de seguimiento.
The usefulness of the determination of circulating antibodies to phenolic glycolipid-I (PGL-I) and/or its synthetic analogs (believed to be specific for Mycobacterium leprae) for the diagnosis and the evaluation of response to therapy and relapse in lepromatous leprosy patients has been well documented (2-4,13,15,19). Furthermore, immunologically a reciprocal relationship between the humoral response and the degree of the cell-mediated immune response as judged by the Mitsuda reaction has been demonstrated in patients with lepromatous leprosy (6). However, the clinical utility of these tests to identify an individual at high risk for development of the disease or to detect subclinical infection in individuals who are infected but in whom the disease has not manifested, has not been proved perhaps because of the long period required to manifest the disease. Moreover, a few epidemiological studies conducted with the currently available techniques have shown the low sensitivity of these tests (1,5,7,9,10,12,18).
The response of an individual to lepromin is yet another parameter used as a test to identify an individual who is likely to manifest the disease (8,11,14).
Although both of these parameters have been well studied in leprosy patients, available comparative data on various populations, e.g., close contacts, nonendemic, lowor high-endemic regions for leprosy are at variance. In the present studies, we have attempted to relate the humoral response, as indicated by the presence of antibodies to natural disaccharide-bovine serum albumin (ND-BSA) and the cell-mediated immune response, as evaluated by the Fernandez and Mitsuda reactions, in children residing in a low-endemic region (LER), a contact population (CP) of children living in a colony of leprosy patients (household contacts), and those residing in the high endemic region (HER) for leprosy in the city of Bombay, India.
MATERIALS AND METHODS
Study subjects. For this study, children ranging in age between 10 and 14 years were investigated.
Low-endemic region (LER) population. Seventy-one children (16 females, 55 males) living in the region not considered to be endemic for leprosy constituted the LER group.
Contact population (CP). Children (N = 140; 56 females, 84 males) residing in the colony of leprosy dwellers were considered as the CP group.
High-endemic region (HER) population. For this HER group, 1495 children in a school located in the high-endemic region for leprosy were investigated. However, the results of the Fernandez reaction were available for only 1340 children (623 females, 717 males); for analytical purposes only the data from these 1340 children were considered.
Reactivity to ND-BSA. The reactivity to ND-BSA was measured on blood spots collected on a filter paper according to the method described earlier (16). A value of > 0.225 expressed as Δ OD 492 nm was considered positive for the presence of anti-ND-BSA antibodies. The Δ OD 492 nm was calculated by subtracting the OD at 492 nm with BSA-coated wells (nonspecific binding) from the OD at 492 nm with ND-BSA-coated wells (specific binding).
Lepromin test. The early (Fernandez at 48-72 hr) and the late (Mitsuda 21 -28 days) responses to lepromin were measured using a human lepromin preparation (10 million AFB/ml) obtained as a kind gift from Dr. Sengupta, JALMA, Agra, India. The early and late reactivities to lepromin were considered positive with responses of > 5 and > 3.0 mm in diameter, respectively.
Statistical analysis. The data gathered were analyzed by the SPSS/PC + computer program (version 4). For comparison of groups, the two-tailed x2 test was used.
RESULTS
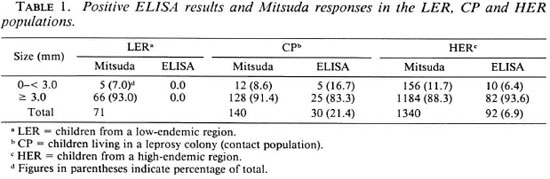
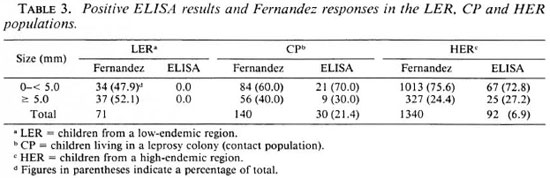
Reactivity to ND-BSA in LER, CP and HER populations. The overall positive ELISA results for anti-ND-BSA antibodies were 0.0%, 21.4% and 6.9% in the LER, CP and HER groups, respectively (Table 1).
The percent positivity of ELISA results in the CP group was 33.9% (19/56) in females which was significantly higher (p <0.005) than that seen in males, 13.1% (11/84). However, in the HER group the reactivity to ND-BSA was comparable in both sexes (5.8%, 36/623 in females; 7.7%, 55/717 in males).
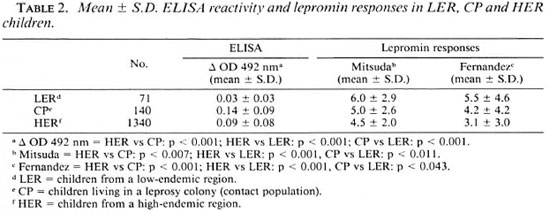
Mean reactivity and frequency distribution. The mean reactivity to ND-BSA in the LER group (0.03 ± 0.03, N = 71) was significantly lower (p <0.001) than in the CP population (0.14 ± 0.09, N = 140) as well as the population residing in the HER (0.09 ± 0.08, N = 1340) (Table 2). A significant difference was also observed in the mean reactivity to ND-BSA between the HER and CP groups (p <0.001).
The frequency distribution of ND-BSA reactivity among these populations is shown in Figure 1. As evident, the median values for the LER, CP and HER groups were 0.02, 0.12, and 0.08, respectively, while the mode in each group was 0.01, 0.23, and 0.0, respectively.
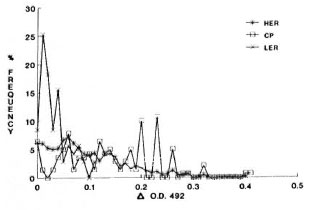
Fig. 1. Frequency distribution of Δ OD 492 nm inthe low-endemic region (LER), contact (CP) and high-endemic region (HER) populations.
Mitsuda reaction. The percent positivity for the Mitsuda response in the LER, CP and HER groups was 93.0, 91.4, and 88.3, respectively, with a criteria for positivity of >3.0 mm in size.
Mean response and frequency distribution. The mean Mitsuda response in the LER was 6.0 ± 2.9, N = 71 which was significantly higher than that seen with the HER population (4.5 ± 2.0, N = 1340, p <0.0001) as well as the CP group (5.0 ± 2.6, N = 140, p - 0.011) (Table 2). A significant difference also was observed between the CP and HER groups (p = 0.007) in the mean reactivity for the Mitsuda response.
The frequency distributions of the Mitsuda responses in these three populations is shown in Figure 2. The median values in the LER, CP and HER groups were 5.5, 5.0, and 4.5, respectively, while the mode for each group was 5.0.
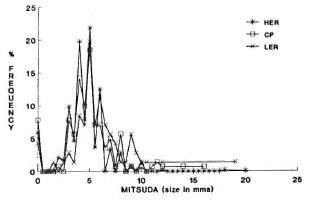
Fig. 2. Frequency distribution of Mitsuda responses in the low-endemic region (LER), contact (CP) and high-endemic (HER) populations.
ELISA results and Mitsuda response. The distribution of the positive ELISA results with respect to lepromin size of <3.0 mm in the CP group (41.7%, 5/12) was significantly higher (p <0.001) compared to that in the HER group (6.4%, 10/156) (Table 1). However, of the total positive ELISA results, the percentage of individuals with a negative lepromin response was not different in the two groups evaluated (5/30, 16.6% in CP; 10/92, 10.9% in HER) (Table 1).
Fernandez reaction. The percent positivity for the Fernandez responses in the LER, CP and HER groups was 52.1 %, 40.0%, and 24.4%, respectively, considering criteria for positivity as >5.0 mm in size (Table 3).
Mean response and frequency distribution. The mean response to the Fernandez reaction in the LER children (5.5 ± 4.6, N = 71) was significantly higher compared to that seen with the HER group (3.1 ± 3.0, N = 1340, p <0.001) as well as that seen with the CP group (4.2 ± 4.2, p <0.043) (Table 2). Similarly, there was a significant difference in the size of the Fernandez responses of the CP and HER groups (p <0.001).
The frequency distributions of the Fernandez responses in these three populations arc shown in Figure 3. The median and mode in the LER population was 5.0 and 0.0; in the CP group, 3.5 and 0.0; and in the HER group, 3.0 and 0.0, respectively.
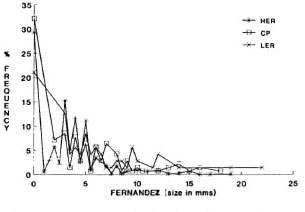
Fig. 3. Frequency distribution of Fernandez responses in the low-endemic region (LER), contact (CP) and high-endemic (HER) populations.
ELISA reactivity and Fernandez response. Within the Fernandez-negative individuals, the percent positive ELISA individuals were significantly higher in the CP group (25.0%, 21/84) compared to that in the HER group (6.6%, 67/1013). However, of the total positive ELISA results, the percentage of individuals associated with a negative Fernandez response was not different in the two groups evaluated (21/30, 70.0% in the CP group; 67/92, 72.8% in the HER group) (Table 3).
DISCUSSION
Since leprosy is a disease in which a long incubation period is required for clinical manifestation, it is essential that an individual who is infected but who has not manifested the disease be identified at the earliest possible time for diagnosis and further management as well as control of the spread of the disease. To reach this goal, several in vitro immunoassays using M. leprae-specif ic antigen preparation(s) as well as the in vivo response to lepromin have been evaluated. ND-BSA, a synthetic analog of PGL-I, specifically detects antibodies to M. leprae and is widely used in seroepidemiological studies. The titers of the anti-ND-BSA antibodies arc raised mostly in the lepromatous type of leprosy, and sera from other forms of leprosy either have low titers or are negative for the presence of anti-ND-BSA antibodies. While there is general agreement that anti-ND-BSA antibodies have an inverse relationship with the Mitsuda response in leprosy patients, such a relationship has not been established in control or contact populations.
Of the three populations examined in the present report, the highest mean ELISA reactivity along with the largest percent positive ELISA results were seen in the CP group; the lowest were seen in the LER group. This finding is not surprising since the children examined in the CP group were living in a leprosy colony and were continuously exposed to M. leprae . However, a higher percentage of ELISA-positive results have been reported in a contact population by Dhandayuthapani, et al. (7) using ND-O-BSA and by Sampatavanich, et al. (17) using the FLA-ABS test. The observed lower ELISA positivity in our studies could be due to a) technical, b) sampling differences, and/or c) the implementation of the MDT program (which might have affected the infectivity of the organism). It is interesting to note that the percent positive ELISA results seen in the LER (0.0) and HER (6.9) groups in the present studies arc very similar to that reported by David, et al. (5).
The frequency distribution analysis of ELISA results showed a larger number of ELISA-positive results in the lower range of Δ OD 492 nm in the LER group (median value 0.02), indicating a nonparametric type of distribution. Similarly, in the HER group a larger number of its population was seen with a lower range of Δ OD 492 nm (median value 0.07) which progressively declined in the higher range (Fig. 1). In contrast, for the CP group the ELISA results were spread over a larger range of Δ OD 492 nm (median value 0.12) with more values in the higher range.
The most striking observation of this study was that while there was a higher percentage of ELISA-positive results associated with females in the CP group, this was not the case in the HER group. The relation of the ELISA results to sex has been a controversial issue. Whether this is due to the age differences, populations surveyed, or any other unknown factor(s) remains to be established.
Unlike the ND-BSA antibody reactivity, the Mitsuda reaction showed a frequency distribution of the Gaussian type in all three of the populations evaluated. Similar findings of a Gaussian-type distribution for the Mitsuda reaction recently has been described by David, el al. (5). Interestingly, the overall mean size as well as the percent positivity for the Mitsuda reaction varied significantly among the populations investigated (LER > CP > HER). Moreover, the administration of lepromin is believed to be a microvaccination and the Mitsuda reaction is a reflection of an immunological competency of an individual which depends upon environmental, nutritional and several other factors. Thus, the criteria for positivity and the interpretation of the Mitsuda reaction may vary for a given population.
It is interesting to note that the mean reactivity and percent positivity for the Fernandez reaction showed a trend similar to the Mitsuda reactivity (LER > CP > HER), implying that it also is a reflection of the underlying immunology. Furthermore, among the antibody-positive individuals, a large proportion of individuals (70.0% in the CP and 72.8% in the HER groups) was Fernandez negative, indicating the Fernandez reaction to be a reflection of immune competence and not only a result of prior exposure to the organism.
An attempt to correlate the humoral response as evaluated by the ELISA results and the cell-mediated immune response (Mitsuda/Fernandez) in the same individual showed poor correlation between the two parameters in all three groups. These findings further support the view that the lepromin response is independent of exposure to M. leprae, and is an immunological reflection of an individual. Nonetheless, it is worth noting that there was an inverse relationship between the two tests evaluated in the LER population, where the mean ELISA results were lowest and the mean Mitsuda response the highest. In the CP group, of the total 30 positive ELISA results 16.7% (5/30) were associated with a Mitsuda reaction of <3.0, which constituted 41.6% (5/12) of the total Mitsuda-negative individuals in the CP group. In contrast, in the HER group, although the negative Mitsuda test was seen in 11.7% (156/1340) of the population examined, only 6.4% (10/156) were also positive in the ELISA. Thus, in the HER population, the Mitsuda reaction was independent of the ELISA reactivity. These findings are corroborated with those of David, el al. (5) who showed that there was no relationship between the Mitsuda responses and the ELISA results in army recruits tested in a leprosy-endemic region.
Keeping in mind the long incubation period of M. leprae before manifestation of symptoms, the predictive value of the two immunodiagnostic tests for the detection of subclinical infection requires a longitudinal study. In our earlier studies with children of the HER, 9 children were found to develop the disease within a 2-year follow-up period (16). Of these, only 4 children had raised levels of anti-ND-BSA antibodies (1 at initial screening and 3 at a later stage) and 2 had a negative Mitsuda response. All but one developed a TT-type single lesion. Only one child who had a Mitsuda response of 2.0 mm along with raised levels of anti-ND-BSA antibodies developed BT-type leprosy. This was expected, since the disease was detected at the initial stages, and the children were immediately brought under MDT. Although the hypothesis suggested by David, et al. (5) relating the size of the Mitsuda response to ELISA results for predicting the type of leprosy is attractive, our data with a limited number of only 9 cases are inadequate to validate it. Nonetheless, it should be borne in mind that we detected the disease at a very early stage where the hypothesis may not be applicable. Additional follow-up years may add more information for interpretation of the Mitsuda and ELISA results.
Acknowledgment. The authors are grateful to Mr. Ajay Kumar, Radiation Medicine Centre (BARC), for his invaluable assistance in data analysis. The authors also are grateful to the Executive Health Officer, Bombay Municipal Corporation, for the permission given for the project.
REFERENCES
1. CARTEL, J.L., CHANTEAU, S., BOUTIN, J.P., PLICHART, R., RICHEZ, P., ROUX, J.F. and GROSSET, J.H. Assessment of anti-phenolic glycolipid-I IgM levels using an ELISA for detection of M. leprae infection in populations of the South Pacific Islands. Int. J. Lepr. 58(1990)512-517.
2. CHO, S.N., CELLONA, R.V., FAJARDO, T.T., JR., ABALOS, R.M., DELÀ CRUZ, E., WALSH, G.P., KIM, J.D. and BRENNAN , P.J. Detection of phenolic glycolipid-I antigen and antibody in sera from new and relapsed Iepromatous patients treated with various drug regimens. Int. J. Lepr. 59(1991)25-31.
3. CHO, S.N., YANAOIHARA, D.L., HUNTER, S.W., GELBER, R.H. and BRENNAN, P.J. Serological specificity of phenolic glycolipid-I from Mycobacterium leprae and use in serodiagnosis of leprosy. Infect. Immun. 41(1983)1077-1083.
4. DANDEKAR, S.R., SHAH, D.H., NAIK, S.S. and GANAPATHI , R. Serodiagnosis of leprosy with PGL-I using ELISA technique. Indian J. Med. Res. 85(1987)597-603.
5. DAVID, H.L., FERNAND, P., CRUAUD, P., BERLIE, H.C., MAROJA, M. DE F., SALEM, J.I. and COSTA, F.C . Relationship between titers of antibodies immunoreacting against glycolipid antigens from Mycobacterium tuberculosis, the Mitsuda and Mantoux reactions, and bacteriological loads: implications in the pathogenesis, epidemiology and serodiagnosis of leprosy and tuberculosis. Int. J. Lepr. 60(1992)208-224.
6. DAVID, H.L., MAROJA, M.F. and CRUAUD, P. Quantitative relationship between anti-PGL-Ispecific antibody levels and the lepromin reaction. Int. J. Lepr. 59(1991)332-334.
7. DHANDAYUTHAPANI, S., ANANDAN, D. and BHATIA V.N . ELISA and lepromin skin tests in household contacts of leprosy patients. Indian J. Med. Res. 91(1990)431-436.
8. DHARMENDRA . Detection of subclinical infection in leprosy. Lepr. India 54(1982)193-207.
9. DOUGLAS, J.T., STEVEN, L.M., HIRSCH, D.S., FUJIWARA, T., NELSON, K.E., MADARANG, M.G. and CELLONA , R.V . Evaluation of four semi-synthetic Mycobacterium leprae antigens with sera from healthy populations in endemic and non-endemic areas. Lepr. Rev. 63(1992)199-210.
10. FINE, P.E.M., PONNIGHAUS, J.M., BURGESS, P., CLARKSON, J.A. and DRAPER, C.C. Seroepidemiological studies of leprosy in northern Malawi based on an enzyme linked immunosorbent assay using synthetic glycoconjugate antigen. Int. J. Lepr. 66(1988)243-254.
11. GUINTO, R.S., DOULL, J.A. and MABALAY, E.B. The Mitsuda reactions in persons with and without household exposure to leprosy. Int. J. Lepr. 23(1955)135-138.
12. KRISHNAMURTHY, P., RAO, P.S., REDDY, B.N., SUBRAMANIAM, M., DHANDAYUDAPANI, S., BHATIA, V., NEELAN, P.L. and DUTTA, A. Seroepidemiological study of leprosy in a highly endemic population of south India based on an ELISA using synthetic PGL-I. Int. J. Lepr. 59(1991)426-431.
13. LEWIS, W.R., MEEKER, H.C., SCHULLER-LEWIS, G., SERSEN, E. and SCHWERER, B. IgM and IgG antibodies to phenolic glycolipid-I from Mycobacterium leprae in leprosy: insight into patients' monitoring, erythema nodosum leprosum and bacillary persistence. J. Invest. Dermatol. 86(1986)529-534.
14. LORD, R., NAISH, C, TAYLOR, C, STANFORD, C.A., STANFORD, J.L., CHAKO, C.J.G., DEBANDU, C , SAMSON, P.D., BERCHMANS, J., SURENDRAN, D., RAMU , G. and REES, R.J.W. Skin test studies on close contacts of leprosy patients in India. Int. J. Lepr. 57(1989)801-809.
15. MEEKER, H.C., SCHULLER-LEVIS, G., FUSCO, F., GIARDINA-BECKET, M.A., SERSEN, E. and LEWIS, W.R. Sequential monitoring of leprosy patients with serum antibody levels to phenolic glycolipid-I, a synthetic analog of phenolic glycolipid-I and mycobacterial lipoarabinomannan. Int. J. Lepr. 58(1990)503-511.
16. SAHASRABUDHE, R., DANDEKAR, S., SHAH, D.H., NAIK, S. and GANAPATHI, R. Filter paper blood spot test for detection of anti-ND-BSA antibodies in school children. Indian J. Med. Res. 95(1992)105-111.
17. SAMPATAVANICH, S., SAMPOONACHOT, P., K.ONGSUEBCHART, K., RAMASOOTA, T., PLNRAT, U., MONGKOLWONGROI, P., OZAWA, T., SASAKI, N. and ABE, M. Immuno-epidemiological studies on subclinical infection among leprosy household contacts in Thailand. Int. J. Lepr. 57(1989)752-765.
18. ULRICH, M., SMITH, P.G., SAMPSON, C, ZUNIGA,M., CENTENO, M., GARCIA, V., MANRIQUE, X., SALGAIX), A. and CONVIT, J. IgM antibodies to native phenolic glycolipid-I in contacts of leprosy patients in Venezuela: epidemiological observations and a prospective study of the risk of leprosy. Int. J. Lepr. 59(1991)405-415.
19. YOUNG, D.B. and BUCHANAN, T.M. Serological test for leprosy with a glycolipid specific for Mycobacterium leprae. Science. 221(1983)1057-1059.
1. B.Sc. (Hons.), B.Sc. (Tech.), Ph.D.; Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Centre (Annexe), Parel, Bombay 400012, India.
2. M.Sc. (Res.), Radiation Medicine Centre, Bhabha Atomic Research Centre, Tata Memorial Centre (Annexe), Parel, Bombay 400012, India.
3. B.Pharm.; Acworth Leprosy Hospital Society for Research, Rehabilitation and Education in Leprosy, Wadala, Bombay 400031, India.
4. M.Sc, M.Sc. (Res.), Acworth Leprosy Hospital Society for Research, Rehabilitation and Education in Leprosy, Wadala, Bombay 400031, India.
5. B.Sc, M.B.B.S., D.V.D., Bombay Leprosy Project, Vidnyan Bhavan, V. N. Purav Marg, Sion-Chunabhatti, Bombay 400022, India.
Received for publication on 6 December 1993;
Accepted for publication in revised form on 5 August 1994.