- Volume 62 , Number 4
- Page: 547–51
Current profile of active leprosy in Greece; a five-year retrospective study (1988-1992)
ABSTRACT
The epidemiological characteristics of newly diagnosed, active leprosy cases (incidence, N = 16 Greeks and 4 expatriates) and relapsed cases (recurrences, N = 25, all Greeks) were studied. Most of the cases were multibacillary, over 50% being lepromatous. The relapses were analyzed by sex, disease duration and residence (rural or urban). Most of the newly diagnosed cases presented with nonreactional skin lesions (70%). The relapses were self-reported and detected mainly because of type 2 leprosy reactions (56%). The main source of the infection for new cases was members of their former extended family. The statistical trend of leprosy in Greece is a continuing decline in a country which already has a very low endemicity.RÉSUMÉ
Les caractéristique épidémiologiques des cas actifs et nouvellement diagnostiqués de lèpre (incidence, N = 16 Grecs et 4 expatriés) et des cas de rechutes (N = 25, tous Grecs), ont été étudiés. La plupart des cas étaient mutibacillaires, plus de 50% étant lépromateux. Les rechutes ont été analysées par sexe, durée de la maladie et résidence (rurale ou urbaine). La plupart des cas nouvellement diagnostiqués présentaient des lésions cutanées non reactionnelles (70%). Les patients avec rechutes s'étaint présentés spontanément et leur détection était due principalement à des réactions lépreuses de type 2 (56%). La source principale d'infection pour les nouveaux cas était des membres de leurs anciennes familles élargies. La tendance statisque de la lèpre en Grèce est une diminution continue dans un pays qui a déjà une très faible endémicité.RESUMEN
Se estudiaron las características epidemiológicas de 20 casos incidentes de lepra activa (de reciente descubrimiento) y de 25 casos de lepra recurrente. Los casos incidentes incluyeron a 16 griegos y a 4 expatriados; todos los casos recurrentes fueron griegos. La mayoría de los casos fueron multibacilares, con más del 50% de casos lepromatosos. Las recaídas se analizaron en función del sexo, duración de la enfermedad, y área de residencia (rural o urbana). La mayoría de los casos nuevos se presentaron con lesiones dérmicas no reaccionales (70%). Las recaídas fueron autoreportadas y se detectaron principalmente debido a la aparición de reacciones del tipo 2 (56%). La fuente principal de la infección de los casos nuevos fueron miembros familiares. La tendencia estadística de la lepra en Grecia, un país de muy baja endemia, señala una continua disminución de la enfermedad.Leprosy still exists in Greece and epidemiological represents a challenge both for dermatology and public health.
It has previously (4) been summarized that the rate at which leprosy spreads in a community depends upon the proportion of susceptible individuals in the population, the opportunity for contact with the disease and, most importantly, the intensity of infection in the community. We, therefore, undertook a 5-year retrospective study including new/incident and relapsed (prevalent) cases of active leprosy. Given that since 1960 our unit works as the only national referral center and leprosarium in Greece, we considered that this nosocomial epidemiologic study might satisfactorily record the actual trends of the disease within a very low en demicity area.
PATIENTS, MATERIALS AND METHODS
All leprosy patients are classified across the spectrum of the disease by a co-estimation of their clinical picture, histopathology, bacterial index (BI) from skin lesions, lepromin test, and medical and epidemiological history. Applied therapeutic modalities have always been those recommended by the World Health Organization (WHO) and data in the leprosy literature.
Yearly incident and relapsed cases were recorded. A total of 20 incident cases (16 Greek, 4 of other nationalities) and 25 relapsed cases (all Greek) were studied within a 5-ycar period (1988-1992). Relapses were mainly old cases who had been treated from first diagnosis with Diasonc® or dapsone monotherapy. After having been discharged from the hospital and after repeated negative tests, they had not shown good compliance and, therefore, had not been properly followed up. It is reasonably suspected that their treatment was neglected or was intermittent.
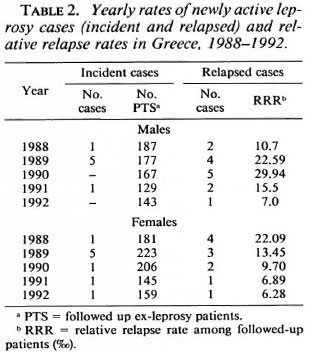
The following parameters were studied: a) disease form distribution, alone and as related to duration, sex and residence; b) distribution of relative relapse rates (8) which indirectly reflects the efficacy of the health policy in regard to tertiary prevention. Yearly diagnosed active, relapsed leprosy cases were the numerator and yearly followed-up cx-leprosy patients (Table 2) were the denominator. All patients are under dapsone maintenance therapy and are examined periodically on clinical grounds and by evaluation of their Bis at our center. After repeated negative tests some patients do not follow instructions when not obliged to be examined at regular periods. Therefore, the number of yearly patients examined patients is not constant (Table 2); c) prevailing symptom that led to the diagnosis (i.e., mainly "cold" or progressive skin lesions or leprosy reaction type 2); and d) statistical forecasting regarding leprosy trends in Greece was also attempted (5,6).
RESULTS
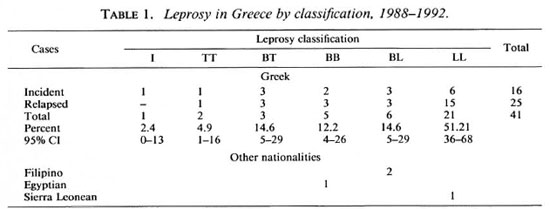
As shown in Table 1, most of the recorded active cases arc Greek. The prevailing forms are multibacillary and the highest frequency is that of lepromatous leprosy with a total of 51.2%; 95% confidence intervals (CI) do not overlap with those of other leprosy forms, a fact that indicates this is the true type distribution of the disease. Fisher's exact test (3,5) revealed no differences of disase-form distribution [paucibacillary (PB) vs. multibacillary (MB)] as a function of disease duration, sex, and residence (rural or urban). It is worth noticing that only in the year 1989 was the rate of the incident cases (10) or new cases detection rate found to be higher than the mean yearly rate of 3.2 new cases. In that year, a place cluster was noted involving 3 out of 5 members of a nuclear family. The source of infection was the mother, misdiagnosed and treated as scleroderma by a rheumatologist (1989, Table 2). Both yearly and relative relapse rates did not show any significant fluctuations.
The need for dermatologic intervention (Table 3) for the incident cases (16 Greek, 4 expatriates) was due to "cold" or progressive, nonreactionsl skin lesions (70%), to type 2 leprosy reaction (25%), and to neurologic symptoms in one case (5%).
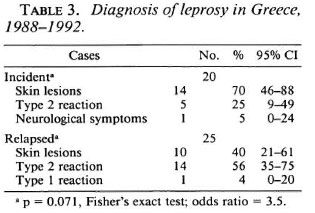
In the 25 relapsed cases group (Table 3) recurrence was recognized by the expression of a type 2 leprosy reaction (56%) "cold" skin lesions (40%) and type 1 reaction in one case of borderline lepromatous leprosy (4%). Thereafter, the presenting problem that led to the diagnosis revealed no clear difference between new and relapsed cases (p = 0.071, Fisher's exact test, odds ratio 3.5).
The mean age of the new cases at the time of diagnosis (6) was 54.8 ± 15.7 years for the MB cases and 26.6 ± 20 years for the PB cases (p = 0.004, 95% CI of the difference, 11-44 years).
Two out of the 16 Greek cases (12.5%) were children <14 years old (6), and they belonged to the previously mentioned family cluster. They were diagnosed as having, respectively, indeterminate and borderline tuberculoid leprosy, making up almost half of the new PB cases.
Age at relapse detection time was 62.2 ± 8.8 years (range 42-82). Age at detection time showed a most significant difference between new (45.9 ± 21.3) and relapsed cases (p < 0.0001). Disease duration of the relapsed cases was 29.4 ± 11.9 years (range 8-48). When estimating disease progression, it was found that 7 out of 25 relapsed cases progressed from PB to MB (28%), 4 remained PB (16%) and the remaining 14 cases were MB from the moment of diagnosis (56%).
Forecasts of new leprosy cases for the years 1988 to 2000 were based upon the abovementioned yearly number of new Greek cases. From the summary of a fit table, the linear model had the smallest standard error (4.03) and R2 was only 0.17. Obviously the trend was not significant. The linear model equation was Y = 6.2 - 1.0 t, which is only indicative of a permanent decline. These data are presented in Figure 1.
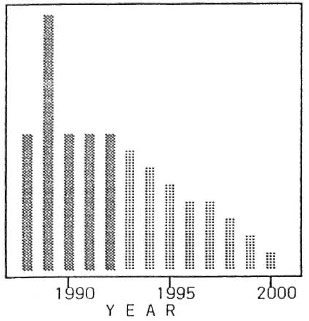
Fig. 1. Leprosy incident cases in Greece for the years 1988 to 2000.  = linear model forecast.
= linear model forecast.
Forecasts of active leprosy relapses are shown in Figure 2. From the summary of a fit table, a quadratic model presented a MAPE = 18.5, SE = 1.23 and R2 = 0.86, the trend was marginally significant, and the quadratic model equation was Y = 4.6 + 2.23 t -0.57 t2.
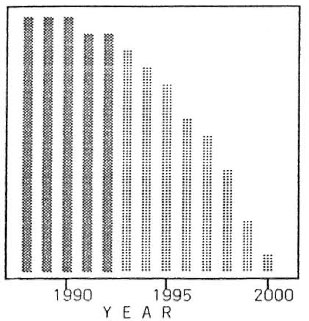
Fig. 2. Recurrences of leprosy in Greece for the years 1988 to 2000.  = quadratic model forecast.
= quadratic model forecast.
A clear decline (Fig. 3) is expected, under present conditions, for the population of followed-up ex-leprosy individuals. A linear model presented a MAPE = 8.6, SE = 39.35 and R2 = 0.59. The linear trend model was statistically significant and the equation was Y = 420.9 - 25.9 t.
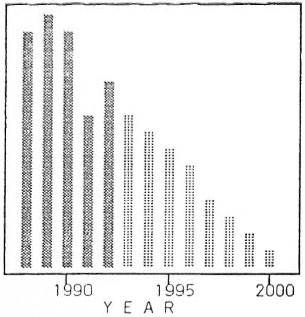
Fig. 3. Followed-up ex-leprosy patients in Greece for the years 1988 to 2000.  = linear model forecast.
= linear model forecast.
COMMENT
In the 20th century, leprosy in Greece has presented a gradual reduction of incidence. No eradication program based on case finding has ever been undertaken. When analyzed by us, general dermatologie nosocomial statistics (8) exclusively (1,2) have shown that in the beginning of the century (1912-1913) the case detection rate of active leprosy among the dermatologie outpatients was 13.87 ‰ (34:2451); in the thirties (1931-1938) it became 2.8 ‰ (182: 64815); in the period studied (1988-1992) it was negligible (< 0.01‰). Further analysis of the same historical data revealed the failure of the asylum-type segregation system which can easily be shown when comparing proportional frequencies of disease forms in the "community" (2) (1931 -1938) and those of leprosaria (7) (1934). Proportional frequencies among dermatologie outpatients (2) were: macular (roughly tuberculoid) 53, tubercular (roughly lepromatous) 88, neural 10, and mixed 5. Among all patients segregated in leprosaria (7) the disease form distribution was: macular 34, tubercular 284, neural 133, and mixed 88. These two series showed a most significant difference with regard to disease form distribution (x2, P < 0.001). This is due to the fact that individuals with macular forms of the disease in the community were fivefold less frequent within leprosaria where MI3 forms prevailed. The etiology of this difference in disease type distribution is difficult to elucidate completely today but might be attributed to the low overall effectiveness of chaulmoogra oil therapy which was associated with a high probability of relapse. In the closed asylum milieu the increased bacillary load could lead to further disease progression.
During the period 1962-1971 (11), a median yearly rate of 35 newly active cases (incident and relapsed) were confirmed at our center; only 8 active cases per year were confirmed in the period studied (1988-1992) with a general reference population of 8 million and 10 million, respectively.
Despite different leprosy classifications through the years, the prevailing form during the 20th century was lepromatous leprosy with a gradual increase in the proportion of lepromatous cases to date (Table 1).
Rapid urbanization and the predominance of the nuclear family pattern (12), which also applies in our country, are factors which result in a shortened exposure of susceptible individuals to Mycobacterium leprae. It has been consistently verified from the epidemiological histories of new cases that the source of infection was one or more relatives within their former extended families.
Avoidance of a clinically apparent stigma was the motive for self-reporting in conjunction with the expectation of an effective therapy and follow up. Our statistical analysis has shown that new case yearly data have the epidemiologic characteristics of a disappearing disease: limited foci, clusters, and erratic time fluctuations (9'), as revealed by the frequency distributions and nonsignificant trends.
The 95% CIs of children <14 years of age, whose leprosy might have been avoided, clearly show that 12.5% was a random chance finding. This is epidemiologically consistent with the decline of relapses as well as the decline in the number of folIowed-up ex-leprosy individuals.
The importation of leprosy from endemic areas by foreign workers and househelpers noted elsewhere (10) seems, at present, to be of negligible epidemiologic impact when estimating only the newly detected cases.
A future leprologic screening of these people may result in social discrimination and will have an adverse side effect upon the secondary and tertiary prevention of leprosy in Greece and in other very low endemicity countries as well.
REFERENCES
1. ARCHIVES OF A. SYGROS HOSPITAL. Yearly statistical tables. G. Fotinos, ed. Athens, 1912-1913 (in Greek).
2. ARCHIVES OF A. SYGROS HOSPITAL. Yearly statistical tables. G. Fotinos, cd. Athens, 1931-1938 (in 8 volumes) (in Greek).
3. ARMITAGE, P., ed. Statistical Methods in Medical Research. Oxford: Blackwell Scientific Publications, 1980.
4. BRYCESON, A.D.M. Leprosy. In: Rook, Wilkinson, Ebling Textbook of Dermatology. Champion, R. H., et at., eds. Oxford: Blackwell Scientific Publications, 1992, pp. 1065-1083.
5. DOANE, D.P., cd. Exploring Statistics with the IBM PC. 2nd edn. Reading, Massachusetts, U.S.A.: Addison Wesley Publishing Co., 1988.
6. HABBEMA, J.D.F., JOSEFZOON, E. and VAN OORTMARSSEN, GJ. Towards the use of decision sciences in leprosy control. Lepr. Rev. 63(1992)48s-52s.
7. KOPANARIS, F. Leprosy. In: Public Health in Greece. Athens: Chronopoulos, 1933, pp. 259-276 (in Greek).
8. KUPPER, L.L., MCMICHAEL, A.J., SYMONS, M.J. and MOST , B.M. On the utility of proportional mortality analysis. J. Chron. Dis. 31(1978)15-22.
9. LECHAT , M.F. Epidemiometric modelling in leprosy based on Indian data. Lepr. Rev. 63(1992)31s-39s.
10. MAHMOUD, S.F. and AZADEH, B. Leprosy in Qatar. Int. J. Dermatol. 30(1991)125-126.
11. PARISSIS, N., STRATIGOS, J., KOUKOUTZAKOGLOU, K. and MARCELOU-KINTI U. Observations epidemiologiques sur la lepre en Grece pendant la periodc 1962-1971. Arch. Inst. Pasteur Hell. 20(1974)95-103.
12. SAIKAWA , K . The effect of rapid socioeconomic development on the frequency of leprosy in a population. Lepr. Rev. 52 Suppl. 1(1981)167-175.
1. M.D., M.P.H., Senior Registrar; Consultant and Head, Department of Dermatology, West Attica General Hospital and Leprosy Center, Greece.
2. M.D., Senior Registrar; Consultant and Head, Department of Dermatology, West Attica General Hospital and Leprosy Center, Greece.
3. M.D., Consultant and Head, Department of Dermatology, West Attica General Hospital and Leprosy Center, Greece.
Reprint requests to Dr. K. P. Kyriakis, 52 Koumanoudi Str., GR-114 74 Athens, Greece.
Received for publication on 22 February 1994.
Accepted for publication in revised form on 10 August 1994.