- Volume 62 , Number 4
- Page: 527–31
Prevalence of hiv infection and high-risk characteristics among leprosy patients of south india; a case-control study
ABSTRACT
With the observation of the occurrence of the human immunodeficiency virus (HIV) infection among leprosy patients in our pilot study carried out in Tamil Nadu, South India, a case-control study was planned to explore whether HIV infection is a risk factor for leprosy and to understand the characteristics of HIV infection and high-risk behaviors among leprosy patients. We screened 556 patients and 1004 nonleprosy controls (matching 502 cases for age, sex and area of residence) for HIV-1 and HI V-2 antibodies. They also were interviewed for personal information on history of blood transfusion, intravenous drug abuse, high-risk sexual behavior, and sexually transmitted diseases. Of the 1019 total cases screened (of both pilot and extended studies), 5 were found to be position for HIV antibodies (HIV-1 = 4, HIV-2 = 1); of the 1019 nonleprosy controls, 6 were positive for HIV-1 antibodies. An analysis by odds ratio revealed no association between leprosy and HIV infection (OR = 0.824, 95% CI = 0.201 -3.593). A strong association was found only between high-risk behavior and HIV infection (OR = 5.186, 95% CI = 1.717-15.667). However, unmarried, unmarried after 30 years of age, exposure to spouses of the leprosy patients, and a history of surgery were all observed to be significantly more common among leprosy patients than the controls.RÉSUMÉ
Après l'observation de la survenue de l'infection par le virus de l'immunodeficience humaine (VIH) parmi les malades de la lèpre dans notre étude-pilote réalisée au Tamil Nadu dans le Sud de l'Inde, une étude castémoins fut planifiée afin d'explorer dans quelle mesure l'infection VIH est un facteur de risque pour la lèpre, et afin d'explorer les caractéristiques de l'infection VIH et les comportements à haut risque parmi les malades de la lèpre. Nous avons dépisté 556 malades et 1004 témoins non-lépreux (en appariant 502 cas pour l'âge, le sexe et al zone de résidence) pour la présence d'anticorps vis-à-vis du VIH-1 et du VIH-2. Ils furent également interogés quant à des antécédents personnels de transfusion sanguine, toxicomanie intraveineuse, comportment sexuel à haut risque et maladies sexuellement transmises. Parmi le total de 1019 patients dépistés (provenant à la fois de l'etude-pilote et de la nouvelle étude), 5 furent trouvés positifs pour la recherche d'anticorps anti-VIH (VIH-1 = 4 et VIH-2 = 1); parmi les 1019 témoins non-lépreux, 6 étaint positifs pour la recherche d'anticorps anti-VIH-1. Une analyse par odds ratio n'a montré aucune association entre la lèpre et l'infection VIH (OR = 0.824, LC 95% = 0.201 et 3.593). On a seulement trouvé une forte association entre un comportement à haut risque et l'infection VIH (OR = 5.186, LC 95% = 1.717 et 15.667). Cependant, le fait d'être non marié, non marié après 30 ans, des contacts avec des conjoints de malades de la lèpre, et des antécédents chirurgicaux sont tous plus fréquemment observés parmi les malades de la lèpre que parmi les témoins.RESUMEN
En un estudio piloto realizado en Tamil Nadu, al Sur de la India, se observó la ocurrencia de infección por el virus de la inmunodeficiencia humana (VIH), entre los pacientes con lepra de esa región. Con base en este hallazgo, se proyectó explorar si la infección por el VIH constituye un factor de riesgo para adquirir la lepra. Así mismo se trató de encontrar alguna relación entre el riesgo de infeción por VIH y los hábitos de vida de los pacientes con lepra. Se buscaron anticuerpos contra VIH-1 y VIH-2 en 556 pacientes con lepra y en 1004 controles sanos, empatando 502 casos por edad, sexo, y área de residencia. Los individuos se interrogaron en cuanto a antecendentes de transfusión sanguínea, abuso de drogas intravenosas, prácticas sexuales de alto riesgo, y enfermedades de transmisión sexual. Del total de 1019 casos entrevistados (incluyendo los casos del estudio piloto), cinco tuvieron anticuerpos contra VIH (4 VIH-1, 1 VIH-2). Éntrelos 1019 controles sanos, hubieron 6 individuos con anticuerpos contra VHI-1. El análisis estadístico de los resultados, no indicó ninguna asociación significativa entre la lepra y la infección por le VHI (OR = 5.186, 95% CI = 1.717-15.667). Sin embargo, se notó que los individuos no casados, los antecedentes de cirugía, fueron más frecuentes en el grupo de pacientes que en el grupo control.The associations between the human immunodeficiency virus (HIV) and tuberculous and certain nontuberculous mycobacterial infections have been established (5). HIV infection was suggested to constitute an important risk factor for leprosy (13), but only a few studies have been carried out in some African countries to determine the association between leprosy and HIV infection (2,4,6,8,9). Some of these studies had limitations in design and some found no association between the two diseases. India has the greatest number of known cases of leprosy and appears to be on the rising curve of an HIV endemic potentially as significant as that in Africa (3), but some of the earlier studies done in north and northeastern India did not find HIV infection among leprosy patients (10,11). An uncontrolled study reported a very low prevalence of HIV infection among leprosy patients from north India (7). Our pilot study done in Tamil Nadu, a south Indian state, showed a higher prevalence of HIV infection among leprosy patients (1), but there was no way in that study to analyze whether such infection has any association with leprosy. With that background, an extended, case-control study was planned to explore whether HIV infection is a risk factor for leprosy and to understand the characteristics of HIV infection and high-risk behaviors among leprosy patients.
MATERIALS AND METHODS
Leprosy patients older than 16 years of age of both sexes attending the outpatient department of the Central Leprosy Teaching and Research Institute, Chengalpattu, India, have been included in the study.
The pilot study (between November 1992 and February 1993) included 463 leprosy patients. About 3 ml of blood was collected from each patient, after obtaining consent, for HIV serology.
The extended study (between July 1993 and October 1993) included 556 leprosy patients. After explaining the study and obtaining their consent, blood was drawn. Relevant information on history of a) blood transfusion; b) intravenous drug abuse; c) high-risk behaviors, namely, extramarital sex (EMS), premarital sex (PMS), extramarital sexual relationships (EMR) of spouses and homosexual sex; and d) sexually transmitted diseases (STD) were collected in a pre-tested pro forma by three well-trained investigators. Absolute confidentiality was assured and maintained.
Controls were selected from the patients attending the nearby Chengalpattu Medical College Hospital, carefully matching the cases for age (± 3 years), sex and area of residence. A total of 1004 appropriate controls could be selected, matching the 502 cases in the extended study (two matched controls for every case). For the remaining 54 cases, we could not select matching controls. Blood samples were drawn from these after obtaining consent. They were interviewed and information collected as per the same pro forma by the same investigators, using the same approach as done for the case group. Subjects who appeared to have leprosy or tuberculosis were not included as controls.
Blood samples were collected using disposable syringes and needles, and were assigned a predetermined code number. The sera were separated and kept at 4ºC until the assays were done and then stored at -20ºC.
HIV antibody screening. The samples collected in the pilot study were tested with an indirect ELISA (Vironostika-HIV MIXT; Organon Tecknika, Holland) and the positive samples were subjected to repeat testing using another indirect ELISA (Rapid Ela-via-MIXT; Diagnostics Pasteur, France).
The samples collected from both the case and control groups in the extended study were tested initially with an indirect ELISA (DETECT-HIV; Biochem Immuno Systems Inc., Canada), and the positive samples were repeat tested with a sandwich ELISA (Wellcozyme-HIV 1 and 2; Murex Diagnostics Ltd., U.K.).
All of those samples found repeatedly positive by ELISA were confirmed by Western blot tests for HIV-1 (NEW LAV-BLOT I; Sanofi Diagnostic Pasteur, France) and HIV-2 (NEW LAV-BLOT II; Sanofi) separately. The procedures for the different tests and the interpretation of results were all done as per the instructions of the manufacturers. Those samples found to be positive by the two ELISAs and further shown to be positive by confirmatory tests were declared as positive for HIV-1 or HIV-2 antibodies.
Data processing was done using computer SPSS software packages and 2 x 2 significance was tested by Fisher's exact chisquared test using EPI-INFO software packages. Multiple logistic regression for calculating the odds ratio was performed using MULTLR software packages.
RESULTS
Of the total 1019 cases screened by both the pilot study and the extended study, 807 were men [32 tuberculoid (TT), 238 borderline tuberculoid (BT), 15 borderline borderline (BB), 107 borderline lepromatous (BL), 346 lepromatous (LL), 61 pure neural (PN), 8 indeterminate (IND)] and 212 were women (14 TT, 39 BT, 2 BB, 30 BL, 72 LL, 11 PN, 4 IND).
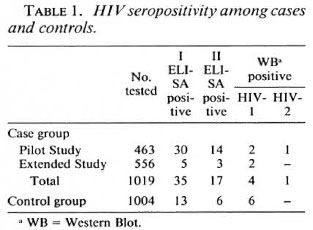
In the pilot study, out of 463 patients screened 30 were positive by the first ELISA (Table 1). The second ELISA detected only 14 out of 30 as positive. Of these, 2 were confirmed to be positive for HIV-1 and 1 was confirmed to be HIV-2 positive.
In the extended study, out of 556 patients screened 5 were positive by the first ELISA (Table 1). The second ELISA identified only 3 out of the 5 to be positive, and of these, 2 were confirmed to be positive for HIV-1.
In the control group, out of the total of 1004 subjects (matched with 502 cases of the extended study) screened, 13 were positive by the first ELISA (Table 1). The second ELISA detected only 6 out of the 13 to be positive and all 6 were confirmed to be positive for HIV-1.
Thus, 5 out of 1019 (0.49%) in the leprosy case group and 6 out of 1004 (0.59%) in the nonleprosy group were observed to be positive for HIV infection.
Regarding their disease status, out of the 5 seropositive leprosy patients, 2 had LL, 2 had BL, and 1 had the BT type of leprosy. All of them had a long duration of disease, ranging from 4 to 20 years. All of them were treated with monotherapy, or multidrug therapy, or both. All of them were found to be bacteriologically negative.
The personal characteristics of the seropositive leprosy patients showed that all of them belonged to the younger age group (28 to 38 years). All were male. Except for one, all were unmarried (80%). Their educational status varied, ranging from a primary to a high school education. All of them had high-risk behavior-had visited commercial sex workers (CSW). Of the 5 cases, 4 had HIV-1 infection and 1 had HIV-2 infection.
The personal characteristics of the 6 seropositive controls showed that they also belonged to the younger age group (22 to 35 years). Four of them were male and 2 were female. Except for one, all were married. Their educational status was variable in this group also. All of them, except for one, belonged to a high-risk group-the men gave a history of visits to CSW and the women revealed extramarital relations (EMR) on the part of their spouses (both of them attended a STD clinic). All 6 controls were positive for HIV-1 infection only.
High-risk behavior was graded for analysis as follows: grade 0 = no history of (h/ o) extramarital sex/premarital sex (EMS/ PMS) of individual/EMR of spouses; grade 1 = h/o EMS/PMS of individual/EMR among spouses; grade 2 = h/o EMS and PMS.
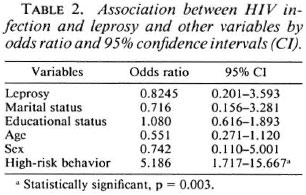
An analysis of the association between HIV infection and leprosy disease, marital status, educational status and high-risk behavior in terms of odds ratio (calculated from matched-set case control by age, sex and area of residence) was done using multiple logistic regression (Table 2). The highest odds ratio (OR = 5.186, CI = 1.717 - 15.667) was between HIV infection and high-risk behaviors, indicating a strong association between HIV infection and high-risk behavior. Leprosy disease had no positive association with HIV infection (OR = 0.824, CI = 0.201 -3.593) or any of the other variables.
A comparative analysis of the personal and high-risk characteristics among case and control groups revealed that the unmarried status and being unmarried after 30 years of age were more common among the leprosy patients (p <0.0001) (Table 3). Exposure to EMS and/or PMS was found to be more common among the leprosy patients (p <0.0001). EMR also was observed to be more common among spouses of leprosy patients (p <0.0001). A history of surgical intervention was also more common among leprosy patients (p <0.0001) with those interventions for leprosy complications contributing most (63%). A history of blood transfusion and a history of homosexual sex were found to be minimal and equal in both of the groups. No one was found to have a history of intravenous drug abuse in cither of the two groups, although some admitted to the use of alcohol (data not shown). A majority of both groups had unprotected sex with their pre- and extramarital contacts.

DISCUSSION
The present, extended case-control study confirmed the observation of the occurrence of HIV infection among leprosy patients of our pilot study. The study also showed that the nonleprosy controls were infected equally with HIV. The leprosy disease status was observed to have no positive association with HIV infection. High-risk behaviors in the form of pre- or extramarital sex, especially with commercial sex workers, was found to have strong association. Thus, it indicated that leprosy by itself does not promote the acquisition of the HIV infection.
On closer examination the leprosy patients were found to indulge in high-risk behaviors. Unmarried status and unmarried after 30 years of age were found to be more common among the leprosy group. All of our seropositive cases were males and most of them were unmarried. Extramarital relationships were observed to be more common among spouses of leprosy patients. Although these findings need further confirmation, leprosy patients arc perhaps relatively more likely to acquire HIV infection by virtue of those high-risk behaviors, even if not by their leprosy disease status per se.
The sparse use of condoms (observed in both groups) and the increased surgical interventions (mostly for leprosy complications) may contribute to the HIV problem among leprosy patients.
Although leprosy as such did not show any active association, we observed more HIV infection among multibacillary patients (80%). Although a few others have also reported a similar observation (6), it needs an in-depth, prospective study to further analyze these relationships.
The probable reason(s) for the failure of the few north Indian studies (10,11) to show HIV infection among leprosy patients were because of the small number of subjects studied. The lower prevalence (0.076%) of HIV infection among leprosy patients shown by the previous study done in north India (7) perhaps was due to the lower endemicity of HIV infection/AIDS in the study area. Tamil Nadu, where the present study was carried out, reported large numbers of seropositives and AIDS cases under the National AIDS Surveillance Programme.
Acknowledgment. We thank Drs. A. V. Paul, R. N. Sharma, A. Ramachandran, C. H. D. Vinod Kumar, G. Leela Bai, and S. Thangaiah of the Clinical Division, CLT&RI, for their cooperation at OPD. We also thank Dr. P. Balusamy, Dean, Chengalpattu Medical College and Hospital, for permitting us to select the controls. We also gratefully acknowledge the help rendered by all of the medical officers and paramedical staffs at CMC hospital. Our special thanks to Dr. P. Krishnamurthy for all his guidance. The technical assistance of Mr. G. Munuswamy and Mr. G. Yusuff, the assistance in photography of Mr. K. S. Sethuraman and the data processing assistance of Mr. D. Pugazhendi, Mr. E. Sathish Kumar, Mr. G. Parthasarathy, and Ms. T. T. Shanthi arc thankfully acknowledged.
REFERENCES
1. JAYASHEELA, M., SHARMA, R.N., SEKAR, B. and THIYAGARAJAN, S.P. HIV infection amongst leprosy patients in South India. Indian J. Lepr. (in press)
2. LEONARD, G. SANGARE, A., VERDIER, M., SASSOU-GUESSEAU, E., PETIT, G., MILAN, J., M'BOUP, S., REY, J.L., DUMAS, J.L. HUGON, J., N'GAPORO, I. and DENIS, E. Prevalence of HIV infection among patients with leprosy in African countries and Yemen. AIDS 3(1990)1109-1113.
3. LUCAS , S. Human immunodeficiency virus and leprosy. Lepr. Rev. 64(1993)97-103.
4. MEERAN , K. Prevalence of HIV infection among patients with leprosy and tuberculosis in rural Zambia. Br. Med. J. 298(1989)364-365.
5. NUNN, P.P. and MCADAM, K.P.W.J. Mycobacterial infections and AIDS. Br. Med. Bull. 44(1988)801-813.
6. OREGE, P.A., FINE, P.E.M., LUCAS, S.B., OBURA, M., OKELO, C, OKUKU, P. and WERE, M. A case control study on human immunodeficiency virus-1 (HIV-1) infection as a risk factor for tuberculosis and leprosy in western Kenya. Tuberc. Lung Dis. 74(1993)377-381.
7. PATIL, S.A., SHIVRAJ, L., SENGUPTA, U., KULSH-RESHTA, K.K., GIRIDHAR, A. and SRINIVASAN, H. Serosurveillance of high risk groups for the prevalence of HIV infection in Agra, India. Virus Information Exchange Newsletter 8(1991)22-23.
8. PEAN, C, PAPE, J.W., DESCHAMPS, M.M. and DAMBREVILLE , M. Prevalence et evolution de l'infection au virus humain d'immunodeficience (VIH) chez les lepreux en Haiti. (Abstract) Int. J. Lepr. 51 Suppl. (1988) 306-307.
9. PONNIGHAUS, J.M., MWANJASI, L.L., FINE, P.E.M., SHAW, M.A., TURNER, A.C., OXBORROW, S.M., LUCAS, S.B., JENKINS, P.A., STERNE, J.A.C. and BLISS , L. I S HIV infection a risk factor for leprosy? Int. J. Lepr. 59(1991)221-228.
10. SAHA, K., CHATTOPADHYA, D., DASH, K., SAHA, U., TYAGI, P.K., GUPTA, M.M., PARAASHARI, A.and SHARMA , A.K. Sexually transmitted diseases in leprosy patients in north and north eastern India; a futile search for human immunodeficiency virus antibody. Int. J. Lepr. 58(1990)660-665.
11. SHIVRAJ, L., PATIL, S.A., GIRDHAR, A., SENGUPTA, U., DESIKAN, K.V. and SRINIVASAN, H. Antibodies to HIV-1 in sera of patients with mycobacterial infections. Int J. Lepr. 56(1988)546-551.
12. TEKLE-HAIMANOT, R., F ROMMEL, D., TADESSE, T., ABEBE, M., VERDIER, M. and DENIS, F. A survey of human T-lymphocytes virus type-1 and human immunodeficiency viruses in Ethiopian leprosy patients. AIDS 5(1991)108-110.
13. TURK, J.L. and REES, R.J.W. AIDS and leprosy. Lepr. Rev. 59(1988) 193-194.
1. B. Sekar, M.D.; Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
2. M. Jayasheela, M.D.; Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
3. D. Anandan, B.Sc.; Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
4. L. Rathinavel, D.M.L.T.; Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
5. B. Vasanthi, M.D., D.M.L.T., Laboratory Division; Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
6. M. Subramanian, M.Sc; Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
7. P. Sivaramakrishna Rao, M.B.B.S., D.P.H., D.T.M.&H., Epidemiology and Statistics Division, Central Leprosy Teaching and Research Institute, Chengalpattu 603001, Tamil Nadu, South India.
8. D. Chattopadhya, M.D., Division of Microbiology, National Institute of Communicable Diseases, Delhi 110054, India.
Present address for Dr. Jayasheela is Director, BCG Laboratory, Madras, India.
Received for publication on 16 May 1994;
Accepted for publication in revised form on 10 August 1994.