- Volume 62 , Number 4
- Page: 609–10
Milia in leprosy
This department is for the publication of informal communications that are of interest because they arc informative and stimulating, and for the discussion of controversial matters. The mandate of this JOURNAL is to disseminate information relating to leprosy in particular and also other mycobacterial diseases. Dissident comment or interpretation on published research is of course valid, but personality attacks on individuals would seem unnecessary. Political comments, valid or not, also are unwelcome. They might result in interference with the distribution of the JOURNAL and thus interfere with its prime purpose.
To the Editor:
Milia arc superficially located, whitish, 4 months later, all of the lesions had flat globoid firm lesions 1-2 mm in size (3).
Primary milia arise spontaneously on the face in predisposed individuals and are derived from the lowest portion of the infundibulum of the vellus hairs. Secondary milia may develop from any epithelial structure, such as a hair follicle and an eccrine sweat duct (3). We report two cases of milia following a subsiding type 1 leprosy reaction.
Case 1
A 50-year-old male with mid-borderline Hansen's disease on treatment with multidrug therapy (rifampin, clofazimine and dapsone) developed erythematous nodules and plaques over his face, trunk and extremities. Type 1 reaction was diagnosed and prednisolone (30 mg/day) was started. The patient was reviewed at regular intervals. After 4 months of therapy all lesions had flattened and there was post-inflammatory pigmentation and atrophy. Multiple, asymptomatic, pin-head-size, whitish papules were seen overlying the subsiding reaction lesions, sparing the normal skin (Fig. 1). Milia was diagnosed clinically and the lesions were extracted. However, a biopsy was not performed.
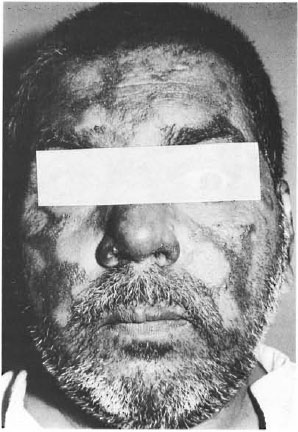
Fig. 1. Milia over subsiding lesions on the face.
Case 2 A 24-year-old male diagnosed to have borderline tuberculoid Hansen's disease on treatment with multidrug therapy (dapsone and rifampin) developed reddish plaques over the face, ears, trunk and extremities with a right-side foot drop. Type 1 reaction was diagnosed and prednisolone (30 mg/ day) was started. On reviewing the patient 4 months later, all of the lesions had flat-tened. Multiple milia were seen over theears and the subsiding lesions (Fig. 2). Ex-traction was advised.
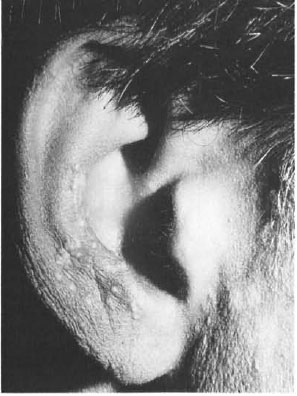
Fig. 2. Milia over the ears.
Secondary milia represent retention cysts caused by proliferative tendencies of the ep-ithelium after injury (3). In our case, the reaction could lead to epidermal damage, and the subsequent repair could be responsible for the development of milia. Secondary milia often is seen in diseases associated with subepidermal bullae, such as bullous pemphigoid, dystrophic epidermolysis bullosa, porphyria cutanea tarda and lichen sclerosus et atrophicus, after dermabrasion, and following trauma (2). It also has been noted after topical steroid therapy (4) and topical 5 fluorouracil therapy (1).
- Acharya Sandhya, M.D.
C. Balanchandran, M.D.
C. R. Srinivas, M.D.
Shruthakirthi D. Shenoi, M.D.
L. Sabitha, M.D.
P. Satish, M.D.
Department of Skin and STD
Kasturba Medical College
Manipal 576119, Karnataka, India
REFERENCES
1. ARNOLD, H. L., JR., ODOM, R. B. and JAMES, W. D. Epidermal nevi, neoplasms and cysts. In: Andrews' Diseases of the Skin: Clinical Dermatology. 8th edn. Philadelphia: W. B. Saunders and Company, 1990, p. 806.
2. LEEPARD, B. and SNEDDON, I.B. Milia occurring in LSEA. Br. J. Dermatol. 92(1975)71 1-714.
3. LEVER, W. F. and SCHAUMBERG-LEVER, G. Histopathology of the Skin: Tumors and Cysts of the Epidermis. 6th edn. Philadelphia: J. B. Lippincott Company, 1983,484-485.
4. TSUJI, T., KADOYA, A., TANAKA, R., KONO, T. and HAMADA, T. Milia induced by corticosteroids. (Letter) Arch. Dermatol. 122(1986)139-140.