- Volume 62 , Number 4
- Page: 614–6
Accurate diagnosis of tuberculosis meningitis using polymerase chain reaction
To the Editor:
Tuberculous meningitis (TBM) is unique and important in the pediatric age group and happens to be the most common cause of death in children suffering from tuberculosis. Favorable prognosis depends upon the early diagnosis of tuberculous meningitis, for which reliable methods based on serology are not available. The ultimate diagnosis for TBM depends on isolation and identification of mycobacterial species, which is time-consuming and often gives negative results in spite of clinical disease. We previously have reported the presence of a repetitive sequence on 5.6-Kb Alul restricted Mycobacterium tuberculosis DNA (4). Subsequently, a polymerase chain reaction (PCR)-based test which amplifies the 169-bp DNA fragment unique to the M. tuberculosis complex from a single-copy region lying adjacent to the repeat clement of 5.6-Kb Alu fragment recently has been reported by us (3). This report describes the evaluation of a PCR test on suspected cases of tuberculous meningitis in a blind manner.
Fifty patients, including 25 controls, attending the pediatric ward of Lok Nayak Jai Prakash Narayan hospital, New Delhi, took part in the study. Twenty-five patients were suspected for TBM on the basis of criteria such as fever, altered sensorium, headache, persistent vomiting, convulsions, neurological deficit, nuchal rigidity and positive history of contact with tuberculosis. CSF analysis showed predominant lymphocyte pleocytosis with protein content over 50 mg% and sugar less than 45 mg%. The controls included 25 patients having pyogenic meningitis, asceptic meningitis, enteric encephalopathy and other neurological disorders. Samples were processed in duplicate, and PCR amplification was carried out with primers KS3-5'CAACCAACATCGC-GCTG 3'; KS4-3' ATAGCCGATGACGG-TCG 5' according to Reddi, et al. (3). At the end of the study the results were compared with the clinical histories of the patients along with culture and smear results. Figure 1 represents an autoradiograph of some of the samples. Figure 2 represents a typical CAT scan finding of a suspected TBM patient. The Table details cumulative results obtained on controls and patients.
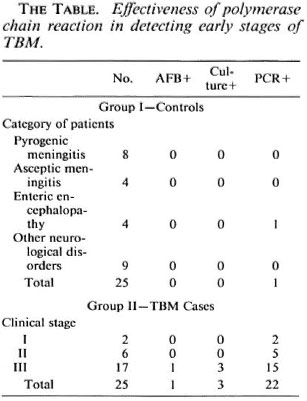
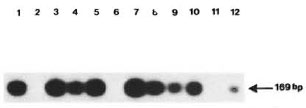
Fig. 1. Typical PCR amplification of some of the CSF samples; arrow indicates presence of 169-bp band.
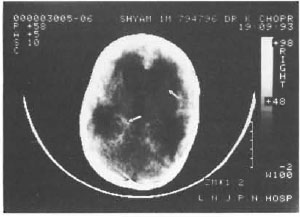
Fig. 2. Typical CAT scan of a suspected TBM patient; arrows denote hydrocephalus and exudative meningitis
Of 25 suspected TBM cases in different stages, a 169-bp amplified product specific to M. tuberculosis was detected in 22; only l was positive by the smear test and 3 were positive by culture tests. Those patients found positive by the PCR test had corroboration with a clinical picture as well as a CAT scan. PCR negativity in three confirmed TBM patients could be due to a low bacilliary load with the clinical manifestation being due to a hypersensitivity reaction. The effectiveness of the PCR test in finding infection in the early stages of the disease is evident (The Table) although studies were carried out on a limited number of samples due to their unavailability. Out of 25 control specimens only one showed false positivity, which could be due to laboratory error.
During the past couple of years, several reports have appeared describing the PCR tests (1,5) and their evaluation of specimens from pulmonary and extrapulmonary tuberculosis cases. Subsequent reports regarding misdiagnosis using the PCR/DNA probe test have appeared (2). The importance of the PCR test in diagnosis is undisputed, and erroneous results occasionally obtained could be due to strain variation-laboratory errors. Thus, it appears important to use more than one set of primer combinations while confirming the diagnosis. The PCR test developed by us initially was evaluated in a blind trial on limited sputum specimens and was found to be 100% accurate with a concordance rate of 76%. The importance of this test is emphasized by the data presented in this communication.
- Amol G. Amin, M.Sc. (Microbiology)
Gene Expression Laboratory
National Institute of Immunology
New Delhi, India
- Ashish K. Garg, M.B.B.S.
Kamlesh Chopra, M.D.
Department of Pediatrics
Lok Nayak Jaiprakash Hospital
New Delhi 110012, India
- Pramod Khandekar, M.Sc, Ph.D.
Gene Expression Laboratory
National Institute of Immunology
Aruna Asafali Marg
New Delhi 110067, India
REFERENCES
1. BRISSON-NOEL, A., AZNAR, C, CHUREAU, C, NGUYEN, S., PIERRE, C, BARTOLI, M., BONETE, R., PIALOUX, G., GICQUEL, B. and GARRIGUE, G. Diagnosis of tuberculosis by DN A amplification in clinical practice. Lancet 338(1991)364-366.
2. BULL, T . J. and SHANSON, D . C. Rapid misdiagnosis by Mycobacterium avium-intracetlulare by rapid PCR/DNA probe tests. Lancet 341(1993)380-381.
3. REDDI, P. P., TALWAR, G. P. and KHANDEKAR, P. S. Repetitive DN A sequence of Mycobacterium tuberculosis: analysis of differential hybridization pattern with other mycobacteria. Int. J. Lepr. 56(1988 ) 592-598.
4. REDDI, P. P., TALWAR, G. P. and KHANDEKAR, P. S. Molecular cloning and characterization of contiguously located repetitive and single copy DN A sequences of Mycobacterium tuberculosis; development of PCR-based diagnostic assay. Int. J. Lepr. 61(1993)227-235.
5. WILSON, S. M., MCNERNEY, R., NYE, P. M., GODFREY-FAUSSETT, P. D., STOKER, N. G. and VOLLER, A. Progress toward a simplified polymerase chain reaction and its application to diagnosis of tuberculosis. J. Clin. Microbiol. 31(1993)776-782.
Reprint requests to Dr. Khandekar.