- Volume 62 , Number 4
- Page: 599–608
Sustainability of leprosy control services in low-endemic situations
The leprosy situation is changing. What should be the future strategy for leprosy control? Will there be a continuing need for leprosy control programs after the World Health Organization (WHO) elimination goal has been achieved and if so, how can we sustain effective and affordable leprosy control services?
This paper deals mainly with the prospects of leprosy control after the WHO elimination goal has been achieved. It will be argued that we will continue to face a substantial leprosy problem after the year 2000, and that the need for leprosy services will remain far into the next century. In order to identify an appropriate organization of leprosy services in low-endemic situations, the need to sustain leprosy services will be discussed and the objectives and strategy of leprosy control and the key elements of patient and program management will be reviewed. Emphasis will be on the identification of the most appropriate and cost-effective measures to sustain leprosy control services under low-endemic conditions.
By "low-endemic conditions" I mean areas where the incidence rate is below 5 per 100,000 population. This is, with the current multidrug therapy (MDT) regimens, roughly equivalent to a prevalence rate below 1 per 10,000 in areas with full MDT coverage.
I shall approach the subject of this paper through the eyes of a health services manager who has to make decisions now with the common sense of a down-to-earth public health specialist who knows that the problem almost exclusively occurs in countries with extremely limited health budgets which demand quick, effective, feasible and affordable solutions to their leprosy problem.
NEED TO SUSTAIN LEPROSY CONTROL SERVICES
What do we mean by the "leprosy problem" and how should we quantify this problem? Leprosy may lead to serious physical, psychological, social and economic suffering, not only for patients but also for their families. The magnitude of this suffering cannot adequately be expressed in quantitative terms. It is obvious that mere information on the number of patients in need of chemotherapy does not sufficiently reflect the leprosy problem.1
It is important to have information on the number of cases requiring chemotherapy as well as on the number of patients in need of care for the "sequelae" of leprosy. The current classification of leprosy-related disabilities is not appropriate to express the disability problem in specific rehabilitation needs.2 Such an information system is still to be developed. For the time being the prevalence of registered leprosy cases, the incidence (as reflected by case detection figures) and the number of persons with leprosy-associated disabilities remain the best possible indicators for the leprosy problem. But we must be aware of the limited values of these figures. Moreover, if these indicators are low at the country level, areas with higher rates may still occur within the country. Such pockets arc mainly found in poor, isolated, rural areas with less accessible health services in the slums of big cities. This unequal distribution of leprosy demands a clear definition of the population figure to be taken as the denominator for the incidence and prevalence rates.
The WHO Study Group on the Epidemiology of Leprosy, which met in 1983, already stated that incidence statistics are more useful than prevalence statistics in monitoring the success of a control program.3 Although one may argue that leprosy remains a public health problem so long as there is transmission of the disease, WHO considers leprosy to be eliminated as a public health problem when the prevalence rate is below 1 per 10,000 population.4 It is expected that the implementation of MDT will reduce transmission and, consequently, incidence. The incidence, as reflected by case detection, is indeed gradually declining in countries which have implemented MDT since the early 1980s. Prior to the introduction of MDT, however, most of these countries already showed a declining incidence. These are mainly countries with a good dapsone monotherapy program, a significant BCG coverage, and/or socioeconomic progress, all being factors associated with declining incidence. 5,6,7 There is so far no convincing evidence that the introduction of MDT has speeded up the declining trend of the incidence, 5,8,9,10 although some data are explained as an indication that the implementation of MDT has an impact on the incidence of the disease." Other programs show a drop in prevalence rates by more than 80%, mainly as a result of updating registers and shortening treatment duration, while at the same time case-detection figures of these programs remain unchanged. 9,12
The choice of the elimination target is an arbitrary one.4 There is no proof that the transmission of the disease will sharply decline as soon as the prevalence rate reaches a level below 1 per 10,000 population. On a global scale, case detection increased from 575,000 in 1990 to 590,000 in 1991 and to 650,000 in 1992. Although this partly may be attributed to improved self-reporting and intensified active case finding, and to lack of precision inherent in global data based on routine field reports, it definitely docs not reflect a declining incidence.
In summary, reduced prevalence docs not necessarily reflect a decline in incidence, and we do not yet have convincing evidence that MDT has an impact on the incidence of leprosy. However, in view of the long incubation period of leprosy and the fact that wide MDT coverage has only been established in some countries during recent years, it is probably too early to expect evidence that the MDT implementation has an impact on incidence. I am convinced that leprosy is a disappearing problem and that not only elimination, as defined by WHO, is possible but that in the long run even complete eradication of leprosy is feasible as a result of a combination of various factors, including socioeconomic development, BCG vaccination, early diagnosis and chemotherapy. This will, however, be a slow process. The incidence of leprosy will remain a significant problem beyond the year 2000, even when the elimination goal has been achieved. All new cases must be detected at an early stage of the disease and must be submitted to regular and complete treatment with MDT. Moreover, an important proportion of new cases already will show disability at diagnosis, and many patients will develop disability after diagnosis. In addition, all current patients with nerve function impairment are at risk of developing increasing disability.
In conclusion, despite the strongly reducing prevalence and a slowly declining incidence, the problem of leprosy and leprosy related disability will continue to exist far beyond the turn of the century, not only for the patients and their relatives but also for the health services and social services. Leprosy services will have to be sustained for decades to come.
The question is how such services should be sustained. In order to identify a sustainable approach, the major components of leprosy control will be reviewed.
REVIEW OF MAJOR COMPONENTS OF LEPROSY CONTROL
Objectives and strategy of leprosy control
The objectives of leprosy control arc: 1) to interrupt transmission of the infection, thereby reducing the incidence of disease; 2) to treat patients in order to achieve their cure and, where possible, complete rehabilitation; and 3) to prevent the development of associated deformities.3
The basic strategy to achieve these objectives includes: 1) early case detection; 2) adequate chemotherapy (a complete course of MDT); and 3) provision of comprehensive care for the prevention of disabilities and rehabilitation of patients through effective coverage of the population with accessible and efficient health services which arc acceptable to the community and the patients.
Among the three components of this strategy, the first two arc the most cost-effective for achieving all three leprosy control objectives. Therefore, the establishment of early case finding and treatment with MDT remain the top priorities.13 In view of the frequent event of new disabilities in patients already under treatment, disability prevention also should be considered as a matter of priority. Fortunately, this aspect is receiving increasing attention, especially in programs where MDT has been successfully introduced.
Considering the limited resources available for low-endemic diseases, leprosy services will not only have to be effective, but also must be affordable. Cost-effectiveness is therefore a major criterion for the appraisal of the sustainability of these services. This paper docs not compare the cost-effectiveness of leprosy control with that of other diseases. Let me just repeat what Prof. Lechat, as ILA president, stated in his address to the 13th ILA Congress: "Priority docs not mean exclusivity. Although leprosy is not the most important health problem, it still affects millions of people and this is unacceptable as we possess the knowledge and tools to prevent the unnecessary suffering caused by the disease.14
Elements of the strategy
Patient management. Case-finding. Self-reporting based on good quality health services is the most appropriate method for case detection under low-endemic conditions. Active case finding is not cost-effective. It implies a lot of work to find relatively few patients, a large number of patients found have self-healing, nondisabling types of leprosy and are thus unnecessarily treated, and often people are wrongly diagnosed.15 Overdiagnosis is mainly attributed to the system of setting unrealistic case-finding targets and overzealousness of field workers fearing to become unemployed if the caseload is too low.16 If the program would rely on passive case finding, this problem would be virtually nonexistent.
The household source of infection is particularly significant in low-endemic areas.17,18,19 In this situation the examination of contacts is the only cost-effective method of active case finding. All current and former household contacts of new patients should be invited to report for examination. This should only be done once and, at the same time, health education should be given.
In many countries leprosy control is still implemented through vertical programs separate from the other health services, having their own staff, logistics and clinics.20 Clinics arc only conducted periodically, for example, once a month. Moreover, the staff and the clinics of such programs arc often associated with the stigma of leprosy. As such they hamper an optimal relationship between leprosy services and the community which may result in delayed diagnosis. Patients often have consulted several general health facilities before they are referred or decide themselves to consult the specific leprosy service. This demonstrates the importance of involving the general health service in case detection.
Diagnostic procedure. Leprosy should be diagnosed only when the disease is clinically or bacteriologically evident. The vast majority of self-reporting patients can be diagnosed and classified using clinical skills only. This is acceptable on the condition that if there are doubts about the classification patients should be submitted to the multibacillary (MB) regimen.13 Many programs have developed their own criteria for clinical classification.21,22,23 There is a need for agreement on a uniform, simple and reliable method for the allocation of patients to the paucibacillary (PB) or MB MDT regimens. Peripheral skin-smear services arc unreliable.23 Skin-smear services will, however, still be required at referral levels for the examination of difficult cases. A uniform treatment regimen for all types of leprosy would solve the classification problem and would, therefore, mean a significant simplification of operational procedures.
Diagnostic tools basically have remained the same since Armauer Hansen discovered Mycobacterium leprae more than 100 years ago.24 A reliable and cheap diagnostic test which can be applied routinely under field conditions would facilitate the early diagnosis of leprosy by general health workers and would contribute to the decentralization and thus to the cost-effectiveness of leprosy services.
Chemotherapy, case-holding and posttreatment surveillance. The MDT regimens are effective, safe and operationally feasible.8 In 1990 both WHO and ILEP published documents calling for attention to the basic rather than the optimal requirements for the implementation of MDT.13,25 This has substantially increased the feasibility of MDT implementation. Even more simplification and flexibility will be required to reach universal MDT implementation and to sustain this under low-endemic conditions. Creative local approaches, sometimes specific for individual patients, will have to be developed by local health staff.
MDT coverage is often taken as the only measure of progress in MDT implementation. This is wrong. We must also look at MDT completion ("cure rates"). Poor accessibility and acceptability of health services result in insufficient treatment compliance. Compared to vertical programs, the general health services usually have wider coverage, arc closer to the community, are permanently accessible, and are more acceptable. It is obvious that they must be involved, not only in case detection, as mentioned earlier, but also in the treatment of patients and in the retrieval of absentees.26,27
Although MDT has proven to be highly efficacious, the regimens are in some programs considered as less effective, second-class regimens only for use by less-developed health services. This is reinforced by the ambiguous recommendation of WHO that 24 monthly doses of the MB regimen are adequate but that the treatment, wherever possible, should be continued up to smear negativity.19 Although the recommendation still is in force, many leprosy control programs have for practical reasons already introduced fixed duration MDT for MB patients instead of continuing until smear negativity. A fixed MB regimen of 24 monthly doses taken within a period of 36 months is highly effective, reduces cost, is more convenient for patients, fosters treatment compliance and reduces the workload of staff Moreover, regular smear examination is not required, and the evaluation of treatment compliance is easier.9,13,28,29 Fixed duration regimens facilitate the delegation of leprosy tasks to peripheral health staff and contribute to cost-effective and thus sustainable leprosy control. A substantial shortening of treatment duration, as currently studied in the WHO field trials with ofloxacin, would mean an important operational improvement.
Post-treatment surveillance should only be passive since relapse rates arc very low or will occur very late. Active surveillance would require an unjustifiable amount of resources. During their treatment patients must be carefully instructed on the signs of nerve function impairment and relapse.8 It is obvious that the shortening of treatment duration would imply very intensive patient education.30
Prevention of disability and rehabilitation. Disabilities still occur among treated patients with distressing frequency. After the introduction of MDT, the immediate priority therefore is the establishment of adequate services for disability prevention. This mainly concerns identification and treatment of reactions and the education of patients in self-care. Since this can be implemented under field conditions by relatively simple measures, the establishment of disability prevention proves cost-effective in a short period of time. The cost of preventing disability is extremely modest when compared to the cost of rehabilitation.31 It is important that patients themselves assume responsibility for the prevention of disabilities. It has been shown that, in this respect, patient education is a powerful tool.32
Adequate disability prevention increases the credibility of the services. This promotes earlier self-reporting of new cases and better treatment compliance and, thus, contributes to the eradication of leprosy.
Involvement of general hospitals in the treatment of patients with complications should be increased, not only in the interest of leprosy patients in need of admission but also in view of the future role of district and regional hospitals as possible referral centers for the diagnosis and initiation of treatment.
Effective disability prevention involves the provision of care for chronic problems as well as acute complications. General health services are permanently accessible and closer to the homes of patients. Therefore they are basically more appropriate for the provision of disability prevention services than vertical programs which are only available once a month.
The feasibility of community-based rehabilitation on a wide scale has still to be demonstrated, but it promises to become the best feasible approach for equitable rehabilitation services in leprosy-endemic countries. It promotes self-reliance and encourages the use of simple methods and techniques which arc acceptable and costeffective.33 Leprosy services of a country should have the same quality level (not lower, but also not higher) as services available for other health programs.27 There is no justification for a separate leprosy rehabilitation service alongside general rehabilitation services.
Program management. Planning, manpower development and training. Commitment of policy makers is an important prerequisite for the effective planning of leprosy control. Changes at the decision-maker levels occur frequently, and this often implies major changes in policy and priority setting. It is an important task for leprosy workers, patients and nongovernmental organizations (NGOs) to keep leprosy on the agenda of the decision-makers. In a recent survey of the ILEP Social Aspects Working Group, only one among the 70 responding countries reported that patients arc often involved in the planning and evaluation of the leprosy control program; 11 countries reported that patients sometimes arc involved.34
After successful introduction of MDT the prevalence of leprosy strongly decreases. It is not cost-effective to maintain a vertical service with only a limited number of patients per health worker. The best way to sustain leprosy services is by incorporation in other health services, particularly the general health services. Paramedical general health care providers play a central role in delivering cost-cffective health interventions. Their training costs less, and they receive lower salaries than doctors. They arc easier to employ in rural areas and usually communicate better with their patients. The mere posting of health workers in the periphery docs not solve the problem of incomplete coverage by the health services: these workers must be well-trained, well-supervised, well-provided with logistical support and linked with well-functioning district health services for referral.35
Under low-endemic conditions general peripheral health workers should still be trained appropriately and supervised to recognize the early signs of leprosy. In general, suspect cases will have to be referred to specialized staff at the referral level who have to confirm the diagnosis and initiate treatment. This may, for example, be a leprosy-tuberculosis supervisor at the district level or a dermatologist at the provincial level. The training of general health workers is going to be of crucial importance. Incorporation of leprosy into the curricula of medical faculties and paramedical schools is essential to sustain effective leprosy expertise within the health services.36
Training in public health and health services management is often neglected. The implementation of the WHO training workshops for program management in leprosy control has been shown to be very useful. The complete management cycle is covered by five modules. It is now time to expand the training workshops to health services managers at the regional and district levels. This will facilitate acceptance of leprosy tasks by the district health services. Fortunately, several ILEP members have shown their willingness to assist in a wider implementation of these management courses.
The private health sector will play an increasing role in the provision of leprosy services. This may pose problems, such as treatment with nonstandard regimens, incomplete treatment, inadequate instructions to patients, and the consequent risk of drug resistance and increased incidence of disability.37,38 National strategics should, therefore, clearly define the role of the private sector, including training and quality control.
Program manual and guidelines. National operational guidelines are necessary for a uniform and sustainable approach to leprosy control in a country. The guidelines should be a careful trade-off between strict directions (e.g., regarding the drug regimens) and instructions which allow program managers to use their own creativity in finding local solutions to specific local conditions (e.g., regarding the periodicity of supervised drug intake). The ILEP guidelines for writing a health workers' manual for national leprosy control programs, which will be published by the end of this year, answers a widely felt need. Several countries have already used it in its draft form for the preparation of their own national manual.
Health management information system. Most vertical programs have detailed recording and reporting systems. With integration, however, the system needs simplification to allow for appropriate data collection by peripheral multipurpose health workers. Only data directly linked to decision-making should be routinely collected.20
The number of records, forms, reports or registers should be reduced to the lowest possible minimum, and should be incorporated into the already existing general health management information system (HMIS). The wide acceptance of the essential indicators as recently identified by both WHO and ILEP is a significant improvement since the previous ILA congress.39,40 The HMIS was simplified and standardized.
Under low-endemic conditions the basic data requirements can be further limited to the number (and rate) of new cases and the proportion cured. Cohort reporting is the most informative technique for monitoring and evaluating the case-holding performance and treatment effectiveness.41
Public education. Early voluntary reporting depends on a population which is aware of leprosy and which has confidence in the services provided for leprosy.30 The purposes of public education is to promote early self-reporting by patients and to foster the acceptance and support of leprosy patients by their community.
Stigma seems to be worse in the countries with the largest leprosy problem, but it continues to exist at lesser levels in most countries. Discrimination against people with leprosy seeking access to medical or socioeconomic services still occurs very often.34 The isolation of vertical leprosy control programs may encourage sufferers from the disease to be rejected. People may find it difficult to understand why leprosy patients need special health services when it is advocated that the victims should be socially integrated.26 Therefore, integration of leprosy control into the general health services has a very positive educational effect upon the community toward reduction of the stigma. This will promote early self-reporting of patients as well as their access to general community institutions.
With the declining leprosy problem a trade-off has to be made in each country between the magnitude of the problem and the required inputs for raising public awareness. In any case, health education on leprosy should be combined with health education on other diseases. This is less expensive and does not set leprosy apart from other health problems.
Logistics. A regular and reliable supply of drugs is crucial for successful leprosy control. Drug shortages undermine the credibility of services, which has a negative effect on compliance and self-reporting.
In several countries the leprosy drug supply system is still organized separately alongside the drug distribution system of the national health services. This is often imposed by donor agencies demanding close monitoring and control of the flow of funds and supplies. Since spoilage and shortages arc problems in many countries, it is understandable that some donors arc reluctant to leave the distribution of their inputs to the general supply system. Vertical systems, however, may collapse when donors withdraw their assistance. If donors want to support the establishment of sustainable leprosy services, they must invest in the national general health services infrastructures, including drug supply systems.
Health systems research. Inadequate leprosy control may to a great extent be attributed to the lack of proper organization and management of leprosy control programs. In addition to management training, health systems research is a potential tool to improve this situation. This is action-oriented, operational research which aims at finding practical solutions to locally specific health services problems. It is useful as a management tool for the identification of appropriate and cost-effective leprosy control activities.
Fundamental research. Fundamental research has, so far, not resulted in practical tools for routine application in the field. Placing myself in the position of a health services manager, I would ask for sensitive and specific tests which arc appropriate for routine application in the field for the diagnosis of disease and infection, for the prediction and diagnosis of reaction and the prediction of relapse. I would also want improved drug regimens which arc effective, easily applicable, nontoxic and cheap for very short duration antibacterial treatment, preferably one regimen for all types of leprosy, and last but certainly not least, for the treatment of reactions.
ORGANIZATION OF SUSTAINABLE LEPROSY CONTROL SERVICES
The acceptance of the leprosy elimination goal by the World Health Assembly has promoted the commitment of member states to the fight against the disease and deserves full support as an important and useful initiative. It should, however, not create the unrealistic expectation that the leprosy problem will be solved by the year 2000. In the first place, the elimination goal is not feasible in several areas which currently have a high incidence of leprosy and, secondly, a considerable leprosy problem will continue to exist for many years after the elimination target has been reached. Therefore, whenever the elimination goal is presented to the public, we should make it clear that even if this goal is attained, significant numbers of new cases of leprosy will still occur and that many people with severe psychological, economic and social problems caused by leprosy will need continued assistance. Leprosy control services shall be required for decades to come.
The crucial questions are: What kind of services should be sustained and at what cost for a low-endemic, slowly disappearing disease? In my opinion the possibility of eradication justifies the input of additional resources. Continued donor assistance will be needed, and donors should be prepared to allocate a substantial part of their assistance to upgrading general health services, including management capacity building, training of general health workers, and health systems research.
WHO has estimated the direct cost to diagnose and cure a leprosy patient in different prevalence situations. At a prevalence rate of over 10 per 10,000 population the estimated average cost for a PB patient is US$30 and for a MB patient US$ 150. At a prevalence rate of about 5 per 10,000 the costs arc $70 and $280, respectively, and at a prevalence below 1 per 10,000, $100 for a PB patient and $400 for a MB patient.42
Decreasing endemicity and increasing cost per patient cured go hand in hand. Nevertheless we must try to reach all patients who require treatment. Full utilization will have to be made of the existing general health service. Several integrated programs have shown that leprosy control can be implemented effectively by the general services.26,27,43,44 Although the day-to-day patient management is done by the general health staff, specialized services must be maintained within the general health services at central and intermediate levels for training, supervision and referral.
The combination of vertical control programs, such as for leprosy and tuberculosis, is not the same as integration within the general health services. The combination of vertical programs increases cost-effectiveness because supervision, training, and patient management for both diseases can be implemented by the same personnel. This reduces the costs of salaries, transport and facilities. The same advantages apply to integration, but with integration the gains arc greater. In addition, combined vertical programs arc subject to most of the limitations of a vertical leprosy program.20 Therefore, integration of leprosy control within the general health services is preferable to combination with another vertical program.
Within the integrated services the specialized technical leprosy component can be combined with those for other diseases, such as, for example, those for tuberculosis or skin diseases. Such a combination of specialized components reinforces most of the advantages of integration. This strategy, together with simplification of the operational procedures, is the best option for sustaining leprosy control services in low-endemic situations.20
A prerequisite for integration is the existence of an adequately functioning general health service infrastructure. Where this does not yet exist, combining the vertical leprosy service with other vertical health programs can be useful as a temporary solution within the framework of a well-planned transition toward real integration.
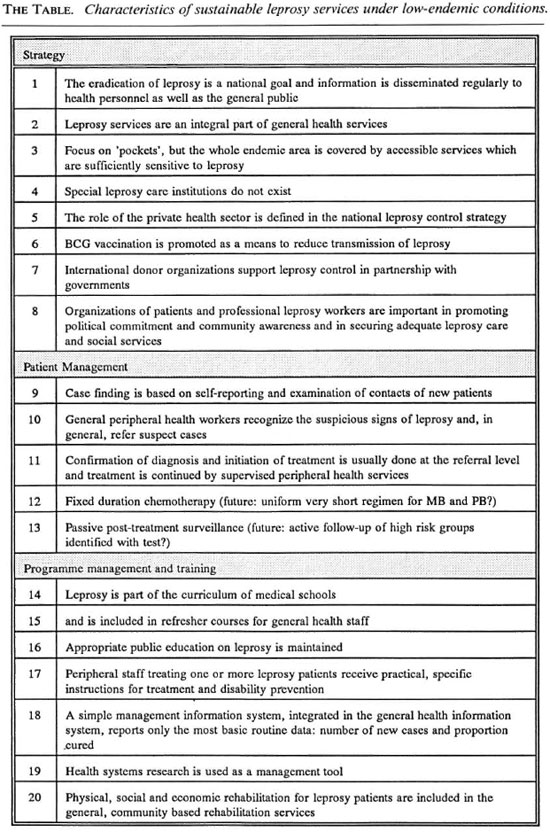
I have tried to show that, although the leprosy problem is declining, leprosy services shall still be needed in many countries during several decades to come. In order to sustain effective and affordable leprosy services, they have to be adapted to the changing situation. I have attempted to identify the major characteristics of such a sustainable approach. The organizational characteristics of sustainable leprosy services in low-endemic situations arc summarized in The Table. This summary is not exhaustive and is certainly not a blueprint for global application. It has to be adapted to the specific situation in each country.
We are facing the exciting challenge of eradicating leprosy, which still causes much suffering, particularly in the poorest communities of the world. This task will not be easy and requires the full collaboration of all parties involved, including governments, WHO and NGOs.
Patient organizations also may play an important role to commit policy makers, health services, donor agencies and the community at large to the eradication of leprosy. Here in the U.S.A. I recall the important role of Stanley Stein and his successors who publish The Star.
Leprosy workers should also be organized in national and international associations. The international association of these professionals should be an active, practical, inspiring organization which has effective relationships with national governments, donor agencies and patient organizations in order to keep leprosy on the agenda of the decision-makers. The members of this association, including field workers, should be dedicated to their common goal: the eradication of leprosy. Should this not be the immediate challenge of the International Leprosy Association?
- Pieter Feenstra, M.D., M.P.H.
Royal Tropical Institute
Wibautstraat 134
1097 DN Amsterdam
The Netherlands
1. Feenstra, P. Needs and prospects for epidemiological tools in leprosy control. Lepr. Rev. 63 Suppl. (1992) 3s-10s.
2. Smith, W. C. S. and Jesudasan, K. Elimination of leprosy and prospects for rehabilitation. (Letter) Lancet 341 (1993) 89.
3. WHO Study Group. Epidemiology of leprosy in relation to control. Geneva: World Health Organization, 1985. Tech. Rep. Ser. 716.
4. Noordeen, S. K. Elimination of leprosy as a public health problem. Lepr. Rev. 63 (1992) 1-4.
5. Pirayavaraporn, C. and Peerapakorn, S. The measurement of the epidemiological impact of multidrug therapy. Lepr. Rev. 63 Suppl. (1992) 84s-92s.
6. Fine, P. E. M. Reflections on the elimination of leprosy. (Editorial) Int. J. Lepr. 60 (1992) 71-79.
7. Muliyil, J., Nelson, K. F. and Diamond, E. L. Effect of BCG on the risk of leprosy in an endemic area: a case-control study. Int. J. Lepr. 59 (1991) 229-236.
8. Consensus development statement on the chemotherapy of leprosy. Int. J. Lepr. 60 (1992) 644-652.
9. Ekambaram, V. Present status of multidrug therapy of Hansen's disease. The Star 52 (1993) 11-14.
10. Becx-Bleumink, M. Priorities for the future and prospects for leprosy control. Int. J. Lepr. 61 (1993) 82-101.
11. Cartel, J. L. Leprosy in French Polynesia; the possible impact of multidrug therapy on epidemiological trends. Lepr. Rev. 63 (1992) 223-230.
12. Tiendrebeogo, A. and Blanc, L. MDT for leprosy in eight countries in fracophone West Africa: ten years implementation. (Abstract) Int. J. Lepr. 61 Suppl. (1993) 43A.
13. International Federation of Anti-Leprosy Associations (ILEP). Basic requirements for implementation of multidrug therapy. Medical Bulletin, issue number 1. Lepr. Rev. 61 (1990) 386-390.
14. Lechat, M. F. Address to the 13th ILA Congress. Int. J. Lepr. 57 Suppl. (1989) 255.
15. Pannikar, V. K. Defining a case of leprosy. Lepr. Rev. 63 Suppl. (1992) 61s-65s.
16. WHO. LEP News, Vol. 2, No. 1, 1993.
17. Jesudasan, K., Bradley, D., Smith, P. G. and Christian, M. Time trends in the analysis of incidence rate of leprosy among household contacts. Indian J. Lepr. 56 (1984) 792-806.
18. Lechat, M. F. Control programmes in leprosy. In: Leprosy. Hastings, R. C , cd. Edinburgh: Churchill Livingstone, 1985, 253-268.
19. WHO Expert Committee on Leprosy. Sixth report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
20. Feenstra, P. Leprosy control through general health services and/or combined programmes. Lepr. Rev. 64 (1993) 89-96.
21. Becx-Bleumink, M. Allocation of patients to paucibacillary or multibacillary drug regimens for the treatment of leprosy: A comparison of methods based mainly on skin smears as opposed to clinical methods; Alternative clinical methods for classification of patients. Int. J. Lepr. 59(1991)292-303.
22. van Brakel, W. H., dc Soldenhoff, R. and Mc-Dougall, A. C. The allocation of leprosy patients into paucibacillary and multibacillary groups for multidrug therapy, taking into account the number of body areas affected by skin, or skin and nerve lesions. Lepr. Rev. 63(1992)231-246.
23. Georgiev, G. D. and McDougall, A. C. A re-appraisal of clinical and bacteriological criteria in the implementation of multidrug therapy for leprosy control programmes and proposals for their better use. Lepr. Rev. 61(1990)64-72.
24. Meyers, W. M. Closing address to the 13th ILA Congress. Int. J. Lepr. 57 Suppl. (1989)270-271.
25. World Health Organization. Report of the consultation on technical and operational aspects of leprosy, Male, June 1990 (WHO/CTD/LEP 90.3). Geneva: World Health Organization, 1990.
26. Feenstra, P. and Tadele, T. A broader scope for leprosy control. World Health Forum 9(1988)53-58.
27. Yuasa, Y. MDT for all; target oriented leprosy control program in the 1990s. Int. J. Lepr. 59 (1991) 624-638.
28. Becx-Bleumink, M. Experiences with WHO-recommended multidrug therapy (MDT) for multibacillary (MB) leprosy patients in the leprosy control programme of the All Africa Leprosy and Rehabilitation Center in Ethiopia. Int. J. Lepr. 59(1991)558-568.
29. Ellard, G. A. Assuring the quality of drugs used for the treatment and control of leprosy. Lepr. Rev. 63(1992)305-316.
30. Ross, W. F. The future of leprosy and leprosy work. (Address given at the occasion of the 25th anniversary of ILEP, Berne, June 1991).
31. International Federation of Anti-Leprosy Associations (I LEP). Prevention of disability; guidelines for leprosy control programmes. Brussels, Belgium: Damien Foundation, 1993.
32. Joint China-TLM Evaluation team: evaluation report; the collaboration project (first stage) of leprosy rehabilitation between the Ministry of Public Health, People's Republic of China and the Leprosy Mission International (1993).
33. Noordeen, S. K. A look at world leprosy. Lepr. Rev. 62(1991)72-86.
34. ILEP Social Aspects Working Group. Social aspects questionnaire: global view of social aspects of leprosy in individual countries and in the world, 1993.
35. World Bank. World Development Report 1993; investing in health (Report no. 11778). Oxford: Oxford University Press, 1993.
36. McDougall, A. C. and Georgiev, G. D. Priorities in leprosy control. Lepr. Rev. 60 (1989) 1-7.
37. Bhat, R. The private/public mix in health care in India. Health Policy Plan. 8 (1993) 43-56.
38. van der Veen, K. W. Government and private health care: two competing institutions. In: Managing Rural Development. Streefkerk, H., Moulik, T. K., cds. New Delhi: Sage Publications, 1991.
39. World Health Organization. Report on the group discussions on the needs and prospects for epidemiological tools in leprosy control. International meeting on epidemiology of leprosy in relation to control, Jakarta, June 1991. Lepr. Rev. 63 Suppl.(1992)114s122s.
40. International Federation of Anti-Leprosy Associations (ILEP). ILEP-B form.
41. Daumerie, D. Surveillance and monitoring of multidrug therapy using cohort analysis. Lepr. Rev. 63(1992)66s-72s.
42. World Health Organization. Global Strategy for the elimination of leprosy as a public health problem. Working document for the third meeting of the WHO working group on leprosy control. Geneva: World Health Organization, 1993.
43. World Health Organization. Report of the consultation on implementation of leprosy control through primary health care. Geneva: World Health Organization, 1986 (WHO/CDS/LEP/86.3).
44. Buchmann, H. Leprosy control services as an integrated part of primary health care programmes in developing countries. Würzburg, Germany: German Leprosy Relief Association, 1978.