- Volume 62 , Number 4
- Page: 626–33
News and notes
This department furnishes information concerning institutions, organizations, and individuals engaged in work on leprosy and other mycobacterial diseases, and makes note of scientific meetings and other matters of interest.
China. Histopathology course held in Cheng-du. A course on histopathology in leprosy supported by American Leprosy Missions (ALM) was held in Cheng-du 24-28 May 1994. Lecturers were Drs. W. M. Meyers and C. K. Job; the 20 participants were experienced histopathologists in leprosy from 12 different provinces of China. Emphasis was on early diagnosis, reactions, neuropathy, differential diagnosis and experimental leprosy. There were lively discussions during the lectures, and the afternoon sessions and evenings were devoted to the reading of slides provided by the lecturers. Five topics for further study were suggested: 1) autopsy series of Chinese patients; 2) histopathology of monolesions among contacts; 3) rifampin-resistance study among multibacillary patients after MDT; 4) prevalence of leprosy among villagers with and without footwear under similar socioeconomic conditions; 5) survey of wild animals for naturally acquired leprosy, especially the tupias. -Li Huan-Ying
India. XVIII Biennial Conference of Indian Association of Leprologists (IAL). The XVIII Biennial Conference of the IAL was held in Madras, 20-22 January 1994, was attended by about 400 delegates from all over the country. A total of 150 papers were presented, 75 as oral presentations and 75 as posters.
The inaugural session started with a welcome by Dr. J. O. Simon, Organizing Secretary of the Conference. This was followed by the chief guest Mr. Justice N. Krishnaswamy Reddy's inaugural address. Dr. S. P. Tripathy, Director General, Indian Council of Medical Research, delivered the keynote address
The President of IAL, Dr. V. Ekambaram, in his address told about his experiences with chaulmoogra oil for treating leprosy before the sulfone era and the success of sulfone therapy until the emergence of sulfone-resistant strains in the 1960s.
The inaugural session ended with a vote of thanks by Dr. J. A. Ponniah, Hon. Secretary of IAL.
The scientific sessions were held on all three days of the Conference. A total of 11 sessions on various aspects of leprosy were conducted under the chairmanship of eminent scientists. Poster sessions were simultaneously conducted along with the oral session during the last two days. In addition to the scientific session, guest lectures by eminent scientists had also been arranged. These lectures included "Rehabilitation in leprosy" (Dr. S. D. Gokhale), "Chemotherapy past, present and future" (Dr. G. Ramu), "Immunotherapeutic vaccine for leprosy, a useful adjunct to chemotherapy" (Prof. G. P. Talwar), "Experimental leprosy" (Dr. C. K. Job) and "A radically different approach to treatment of drug-resistant tuberculosis and leprosy" (Dr. K. Prabhakaran). Dr. M. D. Gupte presented a report "IAL workshop on impact of MDT on trends of leprosy" on the last day. Dr. K. V. Desikan delivered the valedictory address at the concluding session on the last day of the conference. In his address, he pointed out the hard field realities existing in India and cautioned young leprologists against stopping treatment at an early stage of 4 months and doing away with skin-smear examinations. While he was not against changes, he felt that they should be made gradually. Dr. Ramu thanked the organizers of the Conference on behalf of the delegates. -Indian J. Lepr. 66(1994)286-287.
New IAL officers. At the biennial generalbody meeting of the Indian Association of Leprologists (IAL) held on 21 January 1994 at Madras a new team of office bearers was elected for the years 1994-1996. Ninety-six members of the Association attended the general body meeting. The new office bearers arc: President: Dr. M. D. Gupte, Avadi (T N); Vice-presidents: Dr. J. A. Ponniah, Karigiri (T N) and Dr. P. D. Samson, Vizianagaram (A P); Secretary: Dr. P. S. Rao, Chengalpattu (T N) and Treasurer: Dr. Sreevatsa, Avadi (T N).
The following were elected as members of the Central Council: Dr. B. N. Mittal, New Delhi; Dr. B. K. Girdhar, Agra (U P); Dr. P. R. Mangalani, Gwalior(M P); Dr. N. K. Chopra, Bharuch (Gujarat); Dr. C. R. Revankar, Bombay (Maharashtra); Dr. B. N. Reddy, Raipur (M P); Dr. V. P. Bharadwaj, Agra (U P); Dr. Paul Jayaraj, Vizianagaram (A P); Dr. N. B. B. Reddy, Madras (T N).
At the Central Council meeting of the IAL held on 22 January 1994, the following six members were co-opted to the Central Council: Dr. S. Arunthathi, Karigiri (T N); Dr. V. H. Jadhav, Pune (Maharashtra); Dr. T. Gopinathan, Calicut (Kerala); Dr. D. S. Chaudhury, Calcutta (W B); Dr. C. S. Walter, New Delhi; Dr. T. H. Masood Ahmed, Madras (T N).
The new Secretary of the Association may be contacted at the following address: Dr. P. S. Rao, Secretary, Indian Association of Leprologists, Central Leprosy Teaching & Research Institute, Chengalpattu 603 001, India.-Indian J. Lepr. 66(1994)147-148
The Netherlands. Visual aids for training in ocular leprosy. NSL/INFOLEP has produced two slide series and a video film on ocular leprosy developed by Margreet Hogeweg:
Ocular Complications in Leprosy-Africa is a series of 24 slides accompanied by a booklet of 18 pages. A similar set of slides and booklet but featuring Asian patients is also available. The sets have been designed for teachers and self-teaching. They are available free of charge.
Lagophthalmos and Simple Lid Surgery in Leprosy. This 14-minute video film is targeted at leprosy field staff. It focuses on the commonest cause of lagophthalmos- reversal reaction in patients with facial patches-and covers treatment, protection and surgery. (Cost US$20.00)
The Study Aid Foundation Saint-Lazare (SLSL) has reprinted its poster Dangers to the Eye in Leprosy. (Free of charge)
For information or copies of any of the above contact: NSL/INFOLEP, Wibutstr. 135, 1097 DN Amsterdam, The NetherIands-ilep flash 3 (1994) 3
Spain. Queen Fabiola visits Fontilles. On 18 April 1994, Queen Fabiola of Belgium, honorary President of Damien Foundation Belgium, and the Infanta Elena dc Borbon, presided over the inauguration of the Spanish Damien-Fontilles Solidarity Association (DFS).
Accompanied by the President of Damien Foundation Belgium, Dr. Schenkelaars, the Director of Fontilles, Father Moragues and the Medical Director, Dr. Terencio de las Aguas, and representatives of the Spanish government, Queen Fabiola visited the Fontilles Sanatorium and laid flowers at the tombs of the founders, Father Ferris and Joaquin Ballester. Homage was also paid to Father Damien who is to be beatified this year.
There are currently 1415 people with leprosy in Spain, all of whom are under treatment, and the eradication of the disease within 10 years seems certain. Fontilles, founded in 1904 to provide treatment and care for people with leprosy, is increasingly providing residential care for those with disabilities caused other than by leprosy.
The new association has been formed to raise funds for numerous projects in leprosy-endemic countries throughout the world. According to the director of DFS, Mariana Blanco, one of its first objectives is the development of a pilot project in Nicaragua. The project is training health workers in the early detection and treatment of leprosy and leishmaniasis. Consideration will also be given to the socioeconomic conditions surrounding leprosy. -ilep flash 3 (1994) 2
Switzerland. TDR regional networks offer training in tropical disease research. TDR invites junior researchers in Latin America, South-East Asia and the Pacific regions to apply for grants enabling them to acquire graduate (M.Sc. or Ph.D.) or post-doc training in field or laboratory research on malaria, schistosomiasis, lymphatic filariasis, onchocerciasis, Chagas disease, leishmaniasis or leprosy. Grant recipients will receive multidisciplinary training at two or more centers participating in each of the following regional TDR networks:
Latin American Tropical Disease Research Training Consortium. Participating centers: Institute of Biophysics, Federal University of Rio de Janeiro; Department of Biochemistry and Molecular Biology, Oswaldo Cruz Institute, Rio de Janeiro; Fundación CIDEIM, Cali, Colombia; Centers for Disease Prevention and Control (CDC), Atlanta, Georgia, U.S.A. Topics: molecular entomology, vector biology and control, molecular epidemiology, immunobiology and pathogenesis, molecular genetics of virulence, disease surveillance and prevention [ including geographical information systems (GIS) ] . Level: D.Sc. and post-doc Duration: at least 2 years (shorter-term training by arrangement). Starting: March 1995. Deadlines for submission: 15 September 1994. Information from any one of the following: • Hooman Momem, Ph.D., Department of Biochemistry and Molecular Biology, Instituto Oswaldo Cruz, Rio de Janeiro, Brazil [ fax: 55-21/590.34.95; e-mail: momen@brlncc.bitnet ] • Nancy G. Saravia, Ph.D., Fundación CIDEIM, A.A. 5390, Cali, Colombia [ fax: 57-23/672.989; e-mail: cideim@ujccol.bitnet ] • Ulises Lopez, D.Sc, Institute of Biophysics, Universidade Federal de Rio, Rio de Janeiro, Brazil [ fax: 55-21/265.1903 ] • Daniel G. Collcy, Ph.D., Division of Parasitic Diseases, Centers for Disease Prevention and Control (CDC), Atlanta, Georgia [ fax: 1-404/488.7794 ] .
South-East Asian Tropical Disease Research Training Consortium. Participating centers: Department of Medical Research, Yangon, Myanmar; Centre for Health Economics, Faculty of Economics, Chulalongkorn University, Bangkok, Thailand; -Malaria Research Unit, Department of Parasitology, Faculty of Medicine, University of Colombo, Sri Lanka. Topics: malaria-epidemiology, immunology, health economics, treatment, clinical studies, pathogenesis and parasite biology. Level: postgraduate (M. Phil, or Ph.D.). Duration: 2 to 3 years (shorter-term training by arrangement). Starting: March 1995. Deadline for submission: 15 September 1994. Information from any one of the participating centers • Department of Medical Research, 5 Ziwaka Road, Yangon, Myanmar • Centre for Health Economics, Faculty of Economics, Chulalongkorn University, Bangkok 10330, Thailand • Malaria Research Unit, Department of Parasitology, Faculty of Medicine, University of Colombo, Kynsey Road, Colombo 8, Sri Lanka.
Philippine Tropical Disease Research Training Consortium. Participating centers: College of Public Health, University of The Philippines Manila; Clinical Epidemiology Unit, College of Medicine, University of The Philippines Manila; College of Social Sciences and Philosophy, University of The Philippines Diliman; Research Institute for Tropical Medicine, Department of Health. Topics: biomedical research, public health, clinical and social sciences as related to malaria, schistosomiasis, lymphatic filariasis and leprosy. Level: graduate and post-doc. Duration: at least 2 years (shorter-term training by arrangement). Starting: March 1995. Deadline for submission: 15 September 1994. Information from: Dr. Wilfred U. Tiu, College of Public Health, University of The Philippines Manila, P.O. Box EA-460 Ermita, Manila, The Philippines [tel: 63-2/ 596.808; fax: 63-2/521.1394] -TDR news 44 (1994) 5
WHO IMMYC and THEMYC meetings announced. Tentative upcoming IMMYC and THEMYC meetings are shown below.
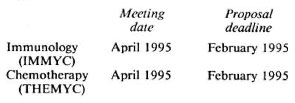
-TDR news 44 (1994) 7
U.K. ILEP expenditures. In 1993, US$3,332,638 (27%) of ILEP expenditure in India directly assisted the activities of the National Leprosy Eradication Programme supplying drugs, and providing for support for district MDT programs and AMPLE programs. With more than 1100 projects in 106 countries, leprosy expenditure (in US dollars) by ILEP members in 1993 was: Control $46.91 million (66%), training $4.12 million (6%), field administration $7.45 million (10%), care/rehabilitation $4.02 million (6%), field support varia $3.53 million (5%), research projects $3.28 million (5%), and journals and congress $1.28 million (2%)-a total of US$70.59 million. ILEP has budgeted US$67 million for leprosy work in 1994.-ilep PANORAMA 1994
Should aid organizations be calculating the cost of death?
"Where should developing countries invest their scarce and precious health care dollars? Is tuberculosis a more important and more easily soluble problem than AIDS? Should the major push be in acute respiratory infections in infancy? Or should developing countries focus on preventing the terrible tobacco scourge of the western world?" (WAT newsletter May 1994, p. 2)
With finite budgets and seemingly limitless disease and disability it is inevitable that governments should make funding decisions based on the comparative economic impact of each disease.
In 1993, in view of limited public health spending, the World Bank published a report which attempted to determine which disease justified the most urgent attention. A common-standard was devised, the "disability-adjusted life year," or DALY, to help make these comparisons. The World Bank is using the DALY to measure the number of health years of life lost through premature death or disability and to assess the cost of a disease to the economy. Should aid organizations, however, be using these comparisons to raise funds?
With 2.7 million annual deaths tuberculosis has become the leading infectious killer of adults. Tuberculosis programs are nevertheless desperately short of funds. Leprosy is the top disabling disease with over 200,000 disabled patients a year. Can disabling diseases be compared with terminal diseases?
Diseases such as tuberculosis and AIDS arc on the increase and quite properly are attracting ever greater attention. It is likely, but not inevitable, that this will cause a drop in funding for leprosy programs. As "competition" increases for ever scarcer funding, leprosy runs the risk of being seen as a disease under control and in decline.
Many organizations, in an effort to maintain funding, are presenting leprosy as a situation where investment pays dividends; by preventing so many people from becoming disabled or deformed, money spent on antileprosy efforts is money saved for countries and their development-money that can be put to other health work. Leprosy work is, in other words, cost-effective. The flip side of this argument is that some diseases are not cost-effective. Should we be using an argument which encourages the calculation of the economic worth of each individual to society?
Equally or perhaps more cost-effective is to utilize the existing leprosy infrastructure for the control of other diseases. This is not a new approach. In Tanzania, to cite but one example, a National Tuberculosis and Leprosy Programme, fully integrated into the national health infrastructure, has been running since 1977. Several ILEP Members fund combined programs tackling more than one health problem (sec FLASH 1/94). DAHW have recently published information stating the many similarities between leprosy and tuberculosis and the advantages inherent in a combined treatment strategy. Both diseases are most widely associated with poverty; both are known to cause a considerable stigma and psychosocial impact; both need a secure regular supply of drugs but can be treated on an ambulatory basis.
In some areas leprosy work is successfully being integrated into the primary health care system. This can only provide an equivalent standard of care for leprosy patients if the primary health system is adequately funded.
Instead of competing aggressively for a bigger share of a limited pool of funds with a concurrent risk of alienating donors from medical development work altogether should not resources be combined? All diseases demand that we strive together to overcome, worldwide, the poverty that allows them to inflict such lasting damage on societies.-ilep flash 3 (1994) 3, 5
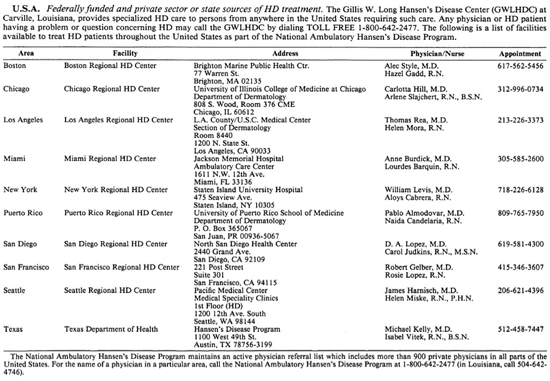
U.S.A. Hansen's Disease in Hawaii. "The first cases of Hansen's disease in Hawaii were recognized as early as 1830. Originally there was no Hawaiian word to describe Hansen's disease, but as cases became more common the term Ma 'i Pake came into use. The translation of this term is Chinese sickness. It is commonly believed that Chinese immigrants introduced the disease to Hawaii, although there is no evidence. There is evidence, however, that immigrant Chinese workers did introduce Hansen's disease to other countries in the Pacific. Hansen's disease may have also been introduced to Hawaii by crews on whaling ships from other countries with endemic Hansen's disease.
"Once the disease was introduced to Hawaii it spread widely through the local population, with particularly high morbidity in the Hawaiian population due to lack of immunity. Hansen's disease cases peaked at approximately 300 cases per year during the 1890s. In 1865, An Act to Prevent the Spread of Leprosy was enacted by the territorial legislature and signed by King Kamchamcha V. It allowed for the establishment of facilities for enforced isolation of people with Hansen's disease.
"As a result of the act, Kalihi Hospital and Detention Station was established near Honolulu Harbor for initial evaluation and treatment of mild and suspect cases. Kalaupapa Settlement (actually the initial settlement was in Kalawao) was the second of the two facilities and received its first patients of nine men and three women on 6 January 1866. Only those patients with advanced disease were sent to Kalaupapa. During this time approximately 92% of all the Hansen's disease cases were Hawaiian or part Hawaiian.
"The first important breakthrough in the care and treatment of Hansen's disease patients occurred in the early 1940s with the advent of sulfone drugs which rendered patients noninfectious and arrested disease progression. At that time, patient care changed from being merely custodial care of the incurable to rehabilitative care. Dapsone therapy was started in Hawaii in 1946.
"With the closing of the Kalihi Hospital and Detention Center, Hale Mohalu Hospital in Pearl City was opened in 1949. Most new patients were managed at Hale Mohalu. The mandatory isolation policy was repealed in 1969 and became the last year in which any new patients were sent to Kalaupapa. Very few patients (32 all voluntary between 1949-1969) were sent to Kalaupapa Settlement. All new patients were then seen on an outpatient basis at Hale Mohalu.
"Beginning in 1982, the Hansen's Disease Community Program (HDCP) was created to manage all newly diagnosed Hansen's disease patients on an outpatient basis. Hansen's disease is notifiable and can be reported to the program by calling 735-2472. The program coordinates medical care for patients through private physicians, Hansen's disease specialists, nurses, and other health care providers. All medical care services and treatment for Hansen's disease are provided free of charge by the state of Hawaii and the federal government as prescribed by Hawaii statutes.
"The occurrence of new Hansen's disease cases in Hawaii has remained relatively stable over the last 5 years, averaging just about 20 new cases per year. Hawaii has an incidence of 1.8 new cases per 100,000, which is the highest state or territorial rate in the U.S.
"The vast majority of Hawaii's newly diagnosed Hansen's disease cases arc immigrants from The Philippines or the South Pacific. Each year there are only one to two cases in Hawaii-born residents. In recent Hawaii-born cases, most have been linked to a previously diagnosed patient and arc often diagnosed through their annual contact screenings. Household contacts of patients are examined annually for 5 years.
"Although all immigrants are medically examined upon entering the United States, Hansen's disease symptoms often go undetected or are ignored by the patient until the patient presents to a physician with much more severe symptoms. Case detection is further hampered by immigrants' difficulty with accessing health care either due to language/cultural barriers or because of a lack of health care coverage. As a result, the median number of months from first symptoms to Hansen's disease diagnosis in Hawaii has been about 12 months over the last 3 years. Recognizing this fact, the HDCP stresses Hansen's disease education for both community physicians seeing immigrants and the immigrant populations themselves.
At the end of 1993, there were 460 patients on the Hansen's disease registry. A total of 378 are on the outpatient registry, with 79 and 3 on the registry at Kalaupapa and Hale Mohalu Hospital, respectively. New Hansen's disease patients are seen on an outpatient basis with only previously institutionalized patients remaining on the Kalaupapa and Hale Mohalu registries.- Mike Maruyama, MPH Planner, Hansen's Disease Community Program, in Communicable Disease Report (Jan./Feb. 1994, pp. 1-3), Hawaii Department of Health Communicable Disease Division.
Vietnam. ILEP at global MDT conference. The following is a statement by Member-Associations of the International Federation of Anti-Leprosy Associations (ILEP) on the occasion of the International Conference on the Elimination of Leprosy as a Public Health Problem, Hanoi, 4-7 July 1994:
-1- ILEP brings together 20 nongovernmental donor associations which together are the most important source of external funding for antileprosy work in endemic countries. Members also offer a considerable fund of expertise.
-2- The Members of ILEP join with the World Health Organization, with governments, and with local partners, in wishing to bring multidrug therapy (MDT) to people with leprosy as quickly as possible, recognizing that it is the most effective available tool for curing the disease, reducing the pool of transmission, and avoiding the disabilities that result from leprosy. In 1990 the Members of ILEP adopted the target of MDT for all by the year 2000. Concerned to bring the best known treatment to every individual who needs it, this target is in a sense even more ambitious than achieving a prevalence rate of 1 per 10,000 population. In projects supported by Members, 64% of all registered patients and 79% of new patients were receiving MDT by the end of 1992. The ILEP Medical Commission is currently consulting projects to identify blocks to 100% coverage.
-3- ILEP Members consider, however, that it is important to speak in terms of the total number of people affected by leprosy and not only in terms of those requiring chemotherapy. The current ILEP estimate for the number of people worldwide affected by leprosy is 6.5 million. Although there may be some overlap, this figure includes around 4 million people with or at risk of deformity as a result of leprosy (ILEP Medical Commission estimate 1992) and around 2.4 million people who are in need of chemotherapy (WHO estimate 1994).
-4- Achievement of MDT for all (ILEP target) and of elimination of leprosy as a public health problem defined as a prevalence of 1 per 10,000 population (WHO target) will be an historic step in the battle against leprosy. Members of ILEP believe, however, that it is most important always to keep in mind that achievement of these objectives does not mean the end of leprosy or of work on behalf of all those people who are and will be affected by the disease. Many heavy tasks will remain beyond the year 2000:
♦ New cases will continue to appear and a number of fully treated cases will relapse. Despite the positive experience of some localities that have had effective leprosy control programs for many years, the number of new cases worldwide has so far shown no sign of decline. It will be essential to sustain highly effective services under conditions of low endemicity, both for the individuals affected and to avoid resurgence of the disease. This will necessitate maintenance of a cadre of people expert in clinical management of the disease.
♦ Many patients after chemotherapy remain with deformities or at risk of them because of permanent nerve damage and loss of sensation. They have a continuing need of medical services.
♦ The tragedy of leprosy for many of those affected is the social stigma that surrounds it. Patients often have need of social and economic assistance to ensure re-integration into their community and normalization of their lives.
-5- Great resources are needed to achieve MDT for all, as well as for the other continuing needs. It would be counter-productive to present the successes achieved with MDT in such a way that those who provide resources-both governments and the hundreds of thousands of individual donors who give to ILEP Members -come to think that the race is over when many laps remain to be run.
-6- Member-Associations of ILEP have for decades been working against leprosy and remain committed to doing so for many years to come. We look forward to continuing to work in partnership with governments, with WHO, and with local associations in the best interests of all who are or who will in future be affected by leprosy.
Signed by the 20 Member-Associations of ILEP-ilep flash 3 (1994) 1,4