- Volume 62 , Number 3
- Page: 374–9
Quantitative assessment of the visibility of unmyelinated corneal nerves in leprosy
ABSTRACT
Unmyelinated corneal nerves were counted in 383 leprosy patients whose eyes looked normal on clinical examination and in an equal number of healthy controls. Visibility of these nerves was decreased significantly (p < 0.01) in the nasal half of the cornea in both patients and controls. There was a significant (p < 0.01) inverse correlation between age and the visibility of these nerves in patients and controls. There was a significant (p < 0.05) reduction in the visibility of these nerves as the spectrum of the disease moved f rom the tuberculoid to the lepromatous pole. There was no significant correlation between visibility of these nerves and the smear positivity of the patient. Neither did duration of the disease nor the duration of antileprosy treatment alter the visibility of these nerves significantly. Overall, there was a reduction in the visibility of these nerves in patients who had had leprosy reactions.RÉSUMÉ
On a compté les nerfs cornéens non myélinisés chez 383 malades de la lèpre dont les yeux paraissaient normaux à l'examen clinique, et chez un nombre égal de témoins en bonne santé. La visualisation de ces nerfs diminuait de manière significative (p < 0.01) dans la moitié nasale des cornées chez les malades et chez les témoins. Il y avait une correlation inverse significative (p < 0.01) entre l'âge et la visualisation de ces nerfs, chez les malades comme chez les témoins. Il y avait une diminution significative (p < 0.01) de la visualisation de ces nerfs à mesure que le spectre de la maladie passait du pôle tuberculoide au pôle lépromateux. Il n'y avait pas de correlation significative entre la visualisation de ces nerfs et la positivité des frottis du patient. Ni la durée de la maladie, ni la durée du traitement anti-lèpre n'ont modifié de manière significative la visualisation de ces nerfs. Dans l'ensemble, il y avait une diminution de la visualisation de ces nerfs chez les malades qui avaient présenté des réactions lépreuses.RESUMEN
Se contaron los nervios corneales en 383 pacientes con lepra cuyos ojos eran clínicamente normales y en un número igual de controles sanos. La visibilidad de estos nervios estuvo significativamente disminuida (p < 0.01) en la mitad nasal de la córnea tanto en los pacientes como en los controles. Hubo una significativa (p < 0.01) correlación inversa entre la edad y la visibilidad de estos nervios en los pacientes y controles; también hubo una significativa (p < 0.05) reducción en la visibilidad de estos nervios conforme el espectro de la enfermedad se movió del extremo tubcreuloide al extremo lepromatoso. Sin embargo, no hubo una correlación significativa entre la visibilidad de estos nervios y la positividad baciloscópica de los pacientes. Ni la duración de la enfermedad ni la duración del tratamiento antileproso alteraron de manera significativa la visibilidad de estos nervios. De manera global sí hubo una reducción en la visibilidad de estos nervios en los pacientes que habían tenido reacciones leprosas.Leprosy is essentially a disease of the peripheral nervous system. Because of its transparent nature, the cornea provides us with the unique feature of viewing the nerves traversing it, thereby affording an interesting opportunity to visualize the affectations of these peripheral nerves. Investigation of these nerves in leprosy has not been commensurate with the perquisite afforded by this anatomical characteristic. From the limbus about 70 to 80 nerve bundles enter the cornea in its midstromal region and run radially toward the center of the cornea (13). When viewed with a slit lamp they appear as thin, thread-like structures that branch dichotomously. Although covered with a myelin sheath near the limbus, they are divested of their myelin sheath after they traverse 0.5 to 1.5 mm into the cornea. Investigators agree that myelination does not usually extend further than 1.5 mm from the limbus (4,12). The unmyelinated portion of the corneal nerves can be visualized only on careful and specialized biomicroscopic examination, and the smaller fibers may not be seen even with such careful examination (4).
Increased visibility of the corneal nerves has been described in various ocular diseases, such as Fuchs' dystrophy, ocular herpes and in keratoconus (12). Increased visibility of these nerves also has been noted in ichthyosis (10), aging (9), neurofibromatosis, pheochromocytoma (11), multiple endocrine neoplasia (6), and in Refsum's syndrome (1).
In leprosy, the corneal nerves have been described as being thickened (17), prominent (15), more visible (12), or beaded (14). Since it is not known whether the unmyelinated nerves of the cornea become more visible in leprosy, we quantitatively assessed the number of unmyelinated, visible corneal nerves that could be observed with careful slit-lamp examination in a group of leprosy patients whose eyes looked normal on clinical examination and in an equal number of healthy individuals. We present our findings here.
METHODS AND PATIENTS
Unselected, consecutive leprosy patients attending the outpatient clinic of the Schieffelin Leprosy Research and Training Center from January 1992 to January 1993 who conformed to certain criteria and whose visual acuity was 6/12 or better were included in the study. Patients with corneal conditions that would obscure visualization of the corneal nerves, such as corneal opacities, corneal dystrophies and degenerations, dellens, pterygiums and arcus senilis, as well as patients with active ocular inflammation and those on chronic topical medication, were excluded from the study. However, patients who had had leprosy reactions but who did not demonstrate signs of active reaction at the time of examination were included in the study. After informed consent was obtained, demographic and leprosy data were recorded.
Leprosy data included: a) current type of leprosy according to the Ridley and Jopling classification using bacteriological, clinical and histopathological parameters; b) approximate duration of the disease; c) treatment status of the patient, whether under antileprosy treatment or whether released from treatment; d) duration and doses of dapsone monotherapy and multidrug therapy (MDT); e) occurrence of reversal or erythema nodosum leprosum (ENL) reactions, and 0 highest bacterial index (BI) recorded at any one time during the course of the disease. The control group consisted of healthy friends and relatives accompanying the patients whose socio-demographic characteristics were similar to those of the patients.
The visible corneal nerves were counted using the + 16 magnification of a Haag-Striet slit lamp and using techniques described by Berliner (3) for visualizing corneal nerves. Adjustments were made by altering the angle of illumination, controlling the width of the slit, lifting the upper lids, and by requesting the patient to shift the eye in a required direction, so as to make as many corneal nerves visible as possible.
Counting of the nerves was done in a circumlinear area 2.5 mm from the limbus. This region was first delineated with the help of a slit beam 2.5-mm long. Exactitude of this region was not possible throughout the counting due to the movements deployed in order to visualize the maximum number of corneal nerves. Neither was counting twice possible due to patient fatigue. However, random double checks were done to safeguard against grossly variable counts in the same eye. If a nerve were to have branched before reaching the counting area, it was counted as two nerves.
Counting was done for each quadrant in the following convenient sequence: left upper temporal, left lower temporal, right upper nasal, right lower nasal, right upper temporal, right lower temporal, left upper nasal and, finally, the left lower nasal quadrant. Counting always commenced above and ended below. The methodology was used consistently for patients and controls, making every attempt to make unbiased assessments. Beading of the corneal nerves was also carefully looked for and noted.
Means, standard deviations and standard errors of the mean as well as proportions were computed and compared using t, normal and F tests. The analysis was done using the statistical package SPSS PC+.
RESULTS
This study included 383 leprosy patients and an equal number of nonleprosy individuals, matched for age and sex.
The number ofvisible, unmyelinated corneal nerves (VUCN) did not differ significantly between the right and the left eyes of patients or controls. Neither was there any significant difference in the quadrant-wise distribution of the mean number of VUCN between both eyes in leprosy as well as the controls (depicted in Fig. 1). Combining and comparing the findings in both eyes of the leprosy patients, the mean (S.E.M.) number of VUCN found in the nasal half of the cornea was 7 (0.21) and in the temporal half of the cornea was 14(0.32). Among the controls, the mean (S.E.M.) number of VUCN in the nasal half was 10 (0.28) and in the temporal half was 16 (0.34). This difference in the VUCN between the nasal and temporal halves of the cornea was statistically significant (p < 0.01) in both leprosy patients and controls.
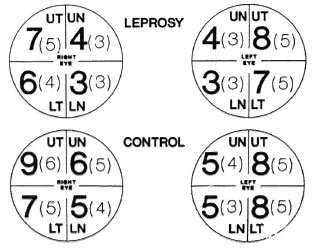
Fig. 1. Mean (S.D.) of the quadrant-wise distri-bution of unmyelinated corneal nerves. UT = Uppertemporal; UN = upper nasal; LT = lower temporal; LN = lower nasal.
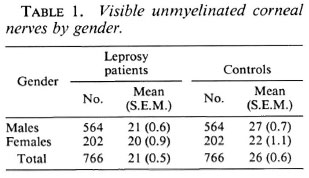
Combining all quadrants of both eyes, the mean (S.E.M.) of the VUCN by gender for leprosy cases and controls are shown in Table 1. The difference between the leprosy cases and controls was statistically significant (p < 0.01). A similar difference was found in males but not in females.
The mean (S.E.M.) of the VUCN by gender for leprosy cases and controls classified in three broad age groups are shown in Figure 2. Male leprosy patients but not female leprosy patients demonstrated a significantly lower (p < 0.01) VUCN than did the controls for all ages except those older than 44 years of age. There is a significant (p < 0.01) inverse correlation between the VUCN and age for both leprosy patients and controls in both males and females.
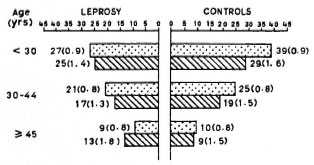
Fig. 2. Mean (S.E.M.) of the distribution of un-myelinated corneal nerves of males and females inthree broad age categories of leprosy patients and controls.  = Males;
= Males;  = females.
= females.
The mean (S.E.M.) of the VUCN for the various types of leprosy by gender is given in Table 2. The mean (S.E.M.) of the VUCN for the various types of leprosy by age is presented in Figure 3. A decreasing trend in the number of VUCN is noted as the type of leprosy moves toward the lepromatous pole. An analysis of variance showed that the difference in means between the different types of leprosy was statistically significant (p < 0.05) on the whole, but the age group below 30 years and females did not exhibit this difference. For each type of leprosy a significant (p < 0.01) inverse correlation of VUCN with age is maintained in both males and females. Although a similar pattern existed on the whole, the correlation coefficient was not significant for the tuberculoid (TT) type of leprosy. This could be due to the lesser number of patients available in this group when compared with those with other types of leprosy. Multibacillary (MB) patients were found to have a significantly (p < 0.01) lower VUCN than paucibacillary (PB) patients.
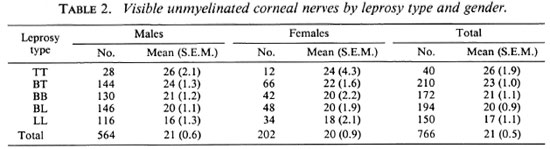
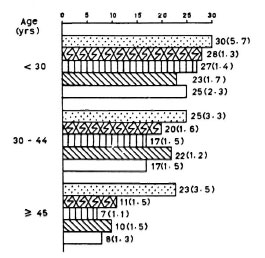
Fig. 3. Mean (S.E.M.) of unmyelinated cornealnerves distributed among the various types of leprosyin three different age groups.  = TT;
= TT;  = BT: ED
= BT: ED  =BB; =
=BB; =  = LL.
= LL.
The bacterial indices (BIs) of smears of the MB patients did not show any significant correlation with the visibility of the unmyelinated corneal nerves. Neither was there any significant association found between the visibility of these nerves and the duration of the disease or the duration of antileprosy treatment. Beading of corneal nerves was found in 18 eyes (2.3%). Among the MB patients, 7% of the eyes had beaded corneal nerves, all associated with a high BI.
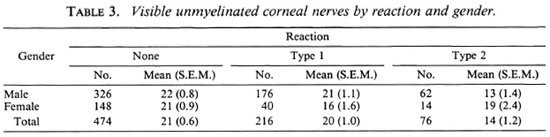
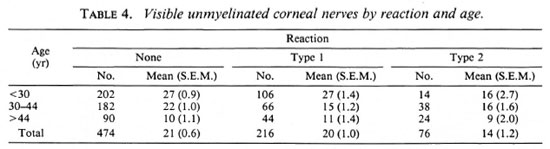
The observations on the VUCN for the various types of leprosy reactions by gender and age are summarized in Tables 3 and 4, respectively. Overall, there was significant difference in the mean number of VUCN by type 1 reactions, but this was noticed in the females (p < 0.01). On the other hand, the mean number of VUCN among patients with type 2 reaction was significantly (p < 0.01) lower than among those with type 1 reaction and those with no reaction, but such a difference was not found among females. Although a significant (p < 0.01) inverse correlation of VUCN with age existed for both types of reactions and for those with no reaction, among males with type 2 reaction and females with type 1 reaction the correlation was not significant.
DISCUSSION
A search of the available literature did not reveal similar studies attempting to quantify the number of visible unmyelinated corneal nerves. Counting of the unmyelinated portion of the corneal nerve was preferred because the myelinated portion is thicker and easily visualized. One aspect of the methodology that could not be controlled effectively was the sustained accurate maintenance of the exact circumlinear area, 2.5 mm from the limbus, in which the nerves were counted. This area, although located initially by the projection of a slit beam of that size, could not be maintained accurately throughout the counting due to the maneuvers undertaken to make as many as possible of the corneal nerves visible. The use of a calibrated eyepiece on the slit lamp may have helped reduce this problem, but such equipment was not available.
We found unmyelinated corneal nerves to be less visible on the nasal half of the cornea among both patients and controls. Nasal obstruction preventing good biomicroscopic examination seemed a plausible explanation for this finding, but detailed examination using appropriate eye movements to negate nasal obstruction as a cause did not increase the visibility of these nerves on the nasal side. It would be interesting to know whether this finding could be confirmed histologically. At present, without an idea as to whether these nerves are by themselves distributed less on the nasal side, we are unable to suggest reasons why these nerves are more visible on the temporal side than on the nasal side.
It is clear from our study that as age increases, visibility of these nerves decreases. Aging processes in the corneal tissues probably contribute to this. We would like to point out here that although age may make a few of the corneal nerves more prominent or more visible, as has been reported in the literature 12), quantitatively the visibility of these unmyelinated corneal nerves decreases rather than increases with age.
Based on several reports that corneal nerves are thickened, prominent or more visible in leprosy, we assumed that there would be an increase in the visibility of the unmyelinated corneal nerves. Contrary to our expectations, the results of our study show that the reverse is true. Unmyelinated corneal nerves are less visible in leprosy when compared with nonlcprosy controls. One reason for this could be that the aging process of the corneal tissues might, in some way, be hastened by leprosy.
One other reason could be immunological; although nerve destruction mechanisms in leprosy have been studied and described in numerous articles, there still exists a lot of controversy on the role of antibodies to the various nerve antigens that have been implicated in the destruction of these nerves in leprosy (2,7,8,18,19). Cho, et al. (5) in studying the serologic responses in sooty mangaby monkeys with experimental leprosy have shown that antineural antibodies are produced during the course of Mycobacterium leprae infection, and that the levels of these antibodies were strongly associated with the onset and progress of clinical leprosy. It is possible that antineural antibodies produced in leprosy patients are the causative factors that clinically give rise to a decrease in the visibility of the unmyelinated corneal nerves. It would be interesting to see if a definite correlation exists between the decreased visibility of these nerves and the increased antineural antibody production in leprosy patients.
Whatever the reason, the results of our study clearly demonstrate that quantitatively there is a reduction in the visibility of corneal nerves in leprosy and that thickening, prominence or increased visibility of these nerves reported in the literature would either pertain to one nerve bundle or a group of nerves and not to all of the nerves visualized in an affected eye.
Another interesting finding is that as the spectrum of the disease moved from the tuberculoid pole toward the lepromatous pole there is a proportionate decrease in the visibility of these nerves. The reason for this, again, could be immunological, and may have a bearing on the role of antineural antibodies. The MB patients showed a significant decrease in the visibility of these nerves compared to PB patients, but there was no significant correlation between smear positivity and the visibility of these nerves. Since the bacillary load of a patient is not obviously implicated, it appears that the neural antibodies may have more to do with the decreasing visibility of these nerves than would the presence of bacteria in large quantities.
Overall, the patients who had ENL reactions during the course of the disease demonstrated a significant reduction in the visibility of these corneal nerves when compared with patients with no reaction or patients who have had only reversal reactions. This is in accordance with the documented evidence that patients with ENL have their nerves destroyed much faster than nonreactional patients. In lepromatous neuropathy, it is believed that immune complexes may play a significant role in nerve destruction, especially during ENL. Patients who develop ENL also are said to have a higher percentage of nerve complications than do those without ENL (16). In our study we found that in type 1 reactions only females exhibited significantly decreased visibility; in type 2 reactions males exhibited this relationship and females did not. We are, however, unable to explain this gender relationship between reactions and the decreased visibility of corneal nerves.
REFERENCES
1. Baum, J., Tannenbaum, M. and Kolodny, E. Refsum's syndrome with corneal involvement. Am. J. Ophthalmol. 60(1965)699-708.
2. Benjamins, J. A., Callahan, R. E., Runft, D., Gerras, G. and Lefford, M. J. Antineural antibodies in leprosy sera: further characterization of the antigens. J. Neuroimmunol. 21(1989)125-135.
3. Berliner, M. L. Biomicroscopy of the Eye; Slit Lamp Microscopy of the Living Eye, Vol. 1. New York: Hoeber, 1949, pp. 227-442.
4. Cho, S. N., Gormus, B. J., Xu, K., Bohm, R. P., Walsh, G. P., Meyers, W. M. and KIM, J.-D. Serological responses to nerve antigen in sooty mangaby monkeys with experimental leprosy. Int. J. Lepr. 61(1993)236-244.
5. Colombo, C. G. and Watson, A. G. Ophthalmic manifestations of multiple endocrine neoplasia, type three. Can. J. Ophthalmol. 11(1976)290-294.
6. Eustis-Turf, E. P., Benjamins, J. A. and Lefford, M. J. Characterization of antineural antibodies in the sera of leprosy patients. J. Neuroimmunol. 10(1986)313-330.
7. Ghaswala, P. S., Mistry, N. F. and Antia, N. H. Serum antibodies of normals and leprosy paticrits show equal binding to peripheral nerve. Int. J. Lepr. 57(1989)690-692.
8. Grayson, M. and Keates, R. Manual of Diseases of the Cornea. Boston: Little Brown, 1969, pp. 112-114; 183; 196.
9. Jay, B., Blanch, R. K. and Liells, R. S. Ocular manifestations of ichthyiosis. Br. J. Ophthalmol. 52(1968)217-226.
10. Koke, M. and Braley, A. E. Bilateral plexiform neuromata of the conjunctive and medullated corneal nerves; report of case. Am. J. Ophthalmol. 23(1940)179-182.
11. Mensher, J. H. Corneal nerves. Surv. Ophthalmol. 19(1974)1-18.
12. Brand, M. E. and Ffytche, T. J. Eye complications in leprosy. In: Leprosy. Hastings, R. C , cd. London: Churchill Livingstone, 1989, p. 226.
13. Millidot, M. A review of research on the sensitivity of the cornea. Ophthalmic Physiol. Opt. 4(1984)305.
14. Pillat, A. Leprosy bacilli in the scrapings from the diseased cornea in a leper, and comments on keratitis punctata superficialis leprosa. Arch. Ophthalmol. 3(1930)306-317.
15. Richards, W. and Arrington, J. Unsuspected ocular leprosy. Am. J. Ophthalmol. 68(1969)492-499.
16. Ridley, D. S. and Job, C. K. The pathology of leprosy. In: Leprosy. Hastings, R. C , ed. London: Churchill Livingstone, 1989, p. 116.
17. Spaide, R., Nattis, R., Lipka, A. and Robert D'a -Mico. Ocular findings in leprosy in the United States. Am. J. Ophthalmol. 100(1985)411-416.
18. Vemuri, N. and Mukherjee, R. Immunorcactivity of nerve lipid antigens in leprosy. J. Clin. Lab. Anal. 5(1991)157-161.
19. Wright, D. J. H., Hirst, R. A. and Waters, M. F. R. Neural auto antibodies in leprosy. Lepr. Rev. 46(1975)157-169.
1. M.B.B.S., M.S., D.O., Department of Ophthalmology, Schieffelin Leprosy Research and Training Center, Karigiri 632106, North Arcot District, Tamil Nadu, India.
2. M.Sc, Department of Community Health.
3. D.P.H., Department of Biostatistics, Christian Medical College, Vellore 632002, India.
Received for publication on 11 April 1994
Accepted for publication in revised form on 6 June 1994.