- Volume 62 , Number 3
- Page: 433–5
A case of secondary syphilis with a remarkable resemblance in histopathologic appearance to indeterminate leprosy
It is well known that early skin manifestations of leprosy may clinically mimic many other skin diseases and, in such instances, histopathological examination is an important adjunct for the diagnosis of the skin lesion. Histopathological confirmation of leprosy in its early stages relies mainly on the finding of acid-fast bacilli (AFB) in protected sites, such as Schwann cells, arrector pili muscle cells or endothelial cells, together with periadnexal inflammation. Searching for AFB in an indeterminate leprosy lesion is an arduous task, and in many such cases AFB are not easily found. In the absence of AFB, infiltration by inflammatory cells or granuloma of the dermal nerves, accompanied by disorganization of nerve parenchyma, contributes to a definite diagnosis of leprosy.1
In this communication we record a case report of secondary syphilis in which the histopathological appearance of the dermal nerves resembled so much that of indeterminate leprosy that an error in diagnosis was a distinct possibility.
CASE REPORT
A 45-year-old male reported with several small, hypopigmented, slightly erythematous, vague skin patches over the trunk and extremities of 10 days' duration. There was no itching or loss of sensations over the lesions. The peripheral nerves revealed no abnormal thickening. The routine laboratory examinations of blood and urine showed no abnormalities. Although the patient denied a history of exposure, there was a strong clinical suspicion of secondary syphilis. Therefore, a VDRL test was done and a skin biopsy was performed to make a histopathologic evaluation.
Histopathological study of the skin biopsy showed no significant change in the epidermis. There were focal collections of chronic inflammatory cells in the dermis occupying less than 15% of the tissue. Inflammation of the neurovascular bundles and selective perincurial inflammation of nerves in the papillary and reticular dermis were present. Acid-fast stain showed no organisms. Because of the well-marked, selective, perincurial inflammation of the nerves in the deep dermis, a diagnosis of early leprosy was seriously considered. The biopsy was partly crushed and, consequently, the cellular details were not clear. Therefore, the biopsy was repeated. The VDRL test was reported positive and it also was repeated.
The histopathological appearance of the second skin biopsy was very similar to the one described earlier. Inflammation of many neurovascular bundles, both in the papillary and reticular dermis, was present. There was selective and marked perincurial infiltration with numerous mononuclear cells (Fig. 1). In the superficial dermis small fragments of nerves without the perineurium were seen lying in the midst of inflammatory cells (Fig. 2). Some of the nerve bundles showed evidence of disorganization and disruption (Fig. 1). In addition to all of these nerve changes, marked endothelial swelling and proliferation, endarteritis and periarteritis were seen (Fig. 3). Examination using the high-power objective clearly showed scattered neutrophils and large clumps of plasma cells around nerves and blood vessels (Fig. 4). The second VDRL test was also positive. A diagnosis of secondary syphilis was preferred although there were perineurial and intraneural inflammation and fragmentation of dermal nerves. The patient was duly treated with high doses of penicillin, and all the lesions disappeared within a month.
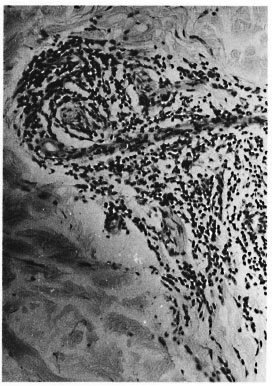
Fig. 1. Several dermal nerves with dense perineurial and intraneural infiltration by mononuclear cellscausing disruption of the nerve bundles (H&E x 90).
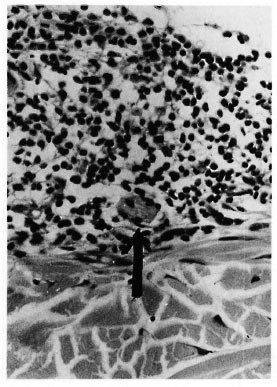
Fig. 2. A remnant of a superficial dermal nervebundle without perineurium lying in the midst of inflammatory cells (H&E x 200).
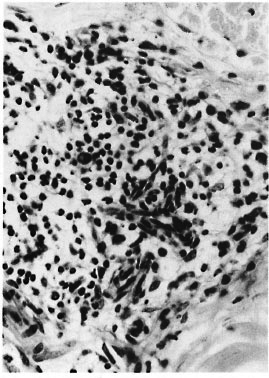
Fig. 3. Endothelial proliferation, endarteritis and periarteritis of the small blood vessels of the skin (H&E x 200).
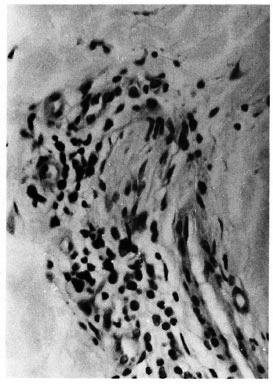
Fig. 4. High-power photomicrograph to show many well-formed plasma cells surrounding a nerve bundle (H&E x 400).
DISCUSSION
Although, in general, selective perineurial and intraneural inflammation with disorganization of dermal nerves are very acceptable criteria for a definite diagnosis of early leprosy, there may be very rarely, as in this case, exceptions. The swelling and proliferation of endothelial cells with endarteritis and periarteritis, the presence of clumps of perivascular plasma cells with scattered neutrophils, a positive VDRL test, and the short duration of the lesion helped to make a definite diagnosis of secondary syphilis in this case. Electronmicroscopic studies of syphilitic lesions have previously shown Treponema pallidum in the endothelial cells of capillaries2 and occasionally even in nerve fibers.3The possibility of the presence of T. pallidum in nerve fibers would explain the marked perineurial and intraneural inflammation and disruption of nerve parenchyma in secondary syphilis.
While diagnosing indeterminate leprosy on the basis of intraneural and perineurial inflammation and even disruption of nerve parenchyma, it would be wise to keep in mind the possibility of occasional nerve involvement in secondary syphilis. The presence of endothelial proliferation with endarteritis and periarteritis and the finding of increased numbers of perivascular plasma cells would certainly help in differentiating the lesion of syphilis from leprosy. Nerve changes suggestive of leprosy have been reported in dermatological conditions with no clinical evidence of leprosy such as lupus vulgaris, secondary syphilis, lichen planus and morphea.4 Therefore, the histopathological diagnosis of indeterminate leprosy in the absence of AFB should always be related with the clinical picture and the results of other relevant laboratory data.
- Charles K. Job, M.D., F.R.C.Path.
G. Anandhan, M.B.B.S., D.L.
J. Jayakumar, M.B.B.S., D.T.M.&H.
M. Aschhoff, M.D.
St. Thomas Hospital and Leprosy Center
Chettupattu 606 801
T.S. District
Tamil Nadu, India
Chettupattu 606 801
T.S. District
Tamil Nadu, India
- S. Kurien, M.D.
Christian Medical College and Hospital
Vellore 632004
N. A. A. District
Tamil Nadu, India
Acknowledgment. The financial support from the American Leprosy Mission International is gratefully acknowledged. We also thank Miss K. Jayanthi for secretarial help.
1. Fine, P. E., Job, C. K., Lucas, S. B., Meyers, W. M., Ponnighaus, J. M. and Stern, A. C. J. Extent, origin and implications of observer variation in histopathological diagnosis of suspected leprosy. Int. J. Lepr. 61(1993)270-282.
2. Sykes, J. A., Miller, J. N. and Kallan, A. J. Treponema pallidum within the cells of a primary chancre from a human female. Br. J. Venereol. Dis. 50(1974)40-44.
3. Poulsen, A., Kobayasi, T., Secher, L. and Weismann, K. Treponema pallidum in macular and papular secondary syphilitic skin eruptions. Acta Derm. Venereol. (Stockh.) 66(1986)251-258.
4. Jacob, M., Chacko, C. J. G., Arunthathi, S. and Chandi, S. M. Significance and interpretation of nerve changes in skin biopsies when present in association with common dermatological conditions. (Abstract) Int. J. Lepr. 52 Suppl.(1984)755.
Present address for Dr. Anandhan: Central Leprosy Teaching and Research Institute, Chingalpattu 603001, India.