- Volume 62 , Number 2
- Page: 256–62
Mass survey of leprosy in Lalitpur District, Nepal
ABSTRACT
An intense mass survey of leprosy in Lalitpur District, Nepal, was carried for the period 1986 to 1990. This was the first such large scale survey in Nepal; 85% of the total population was examined. The 5-year case detection rate was 13 per 10,000; the 5-year child detection rate was 4 per 10,000. By the end of the survey the prevalence rate was 6.8 per 10,000; at the end of 1992 this had dropped to 2.2 per 10,000. In 1989, after a 3-year interval, a re-survey was done in three village development committees (VDCs) and 4 new cases were detected, bringing the 3-year case detection rate to 3.3 per 10,000; 36% of the old cases, 20% of the new adult cases, and 3% of the new child cases were classified as multibacillary. Overall, 62.7% of the patients had no disability, 18.8% had disability grade 1, and 12.7% had disability grade 2 while for 5.8% the data were incomplete. By the end of the survey 91% of the patients needing medical treatment were on multidrug therapy (MDT). At present this has increased to 100%. The regularity rate was 86%; at the end of 1992 this had increased to 96%. The cost for detecting one new patient was US$298. Because of the high cost, it is recommended that intense mass surveys not be performed when the estimated prevalence rate is less than 10 per 10,000 inhabitants. F rom the data collected conclusions were drawn and recommendations were formulated for developing new strategies for the National Leprosy Control Programme of the Government of Nepal.RÉSUMÉ
Une enquête intensive de masse pour la lèpre a été réalisée dans le District de Lalitpur, au Népal, pour la période de 1986 à 1990. C'était la première enquête à une telle échelle au Népal; 85% de la population totale fut examinée. Le taux de détection pour les cinq années était de 13 pour 10,000; ce même taux était de 4 pour 10,000 chez les enfants. A la fin de l'enquête, le taux de prévalence était de 6.8 pour 10,000; fin 1992, celuici était descendu à 2.2 pour 10,000. En 1989, après un intervalle de trois ans, une nouvelle enquête fut réalisée dans trois "comités de développement villageois" (CDV), et 4 noveaux cas furent détectés, donnant un taux de détection sur trois ans de 3.3 pour 10,000; 36% des cas anciens, 20% des nouveaux cas adultes, et 3% des nouveaux cas enfants étaient classés comme multibacillaires. Globalment, 62.7% des patients n'avaient pas d'incapacités, 18.8% avaient une incapacité de grade 1, et 12.7% une incapacité de grade 2; les données étaient incomplètes pour 5.8% des cas. A la fin de l'enquête, 91% des cas nécessitant un traitement médical étaient sous polychimiothérapie (PCT). Ceci a présentement augmenté à 100%. Le taux de régularité était de 86%; à la fin de 1992, il avait augmenté à 96%. Le coût pour détecter un patient était de 298 US$. A cause du coût élevé, il est recommandé que les enquêtes intensives de massse ne soient pas réalisées quand la prévalence estimée est inférieure à 10 par 10,000 habitants. A partir des données récoltées, on a tiré des conclusions et on a formulé des recommandations pour développer de nouvelles stratégies pour le Programme National de Lutte contre la Lèpre du Gouvernement du Népal.RESUMEN
De 1986 a 1990 se llevó a cabo un extenso estudio masivo para la búsqueda de casos de lepra en el Distritio Lalitpur de Nepal. Se logró examinar al 85% de la población total. La tasa de detección de casos en ese periodo de 5 años fue de 13 por 10,000, la tasa de detección de casos infantiles fue de 4 por 10,000. Al final del estudio la tasa de prevalência fue de 6.8 por 10,000 y a finales de 1992, ésta había caído a 2.2 por 10,000. En 1991, después de un intervalo de 3 años, se recstudiaron 3 aldeas, detectándose 4 nuevos casos, llevando la tasa de detección a 3.3 por 10,000. Treinta y seis porciento de los casos antiguos, 20% de los nuevos casos adultos, y 3% de los nuevos casos infantiles, se clasificaron como multibacilares. El 62.7% de los pacientes no tuvieron multilaciones, el 18.8% tuvieron invalides de grado I, y 12.7% tuvieron invalides de grado 2; para el 5.8% de los pacientes estos datos fueron incompletos. Hacia el final del estudio, el 91% de los pacientes que necesitaban tratamiento, estaban bajo tratamiento con poliquimioterapia (PQT). Actualmente el tratamiento con PQT cubre al 100 de los casos. La frecuencia de regularidad, que al finalizar el estudio era del 86%, a finales de 1992 fue del 96%. El costo de detección de un nuevo paciente fue de US$298. Debido a este elevado costo se recomienda que los estudios masivos de detección de casos sólo se efectúen cuando la tasa de prevalenca estimada sea mayor de 10 por 10,000 habitantes. De los datos colectados se han sacado conclusiones y se han formulado recomendaciones para el desarrollo de nuevas estrategias para el Programa Nacional de Control de la Lepra del gobierno de Nepal.Approximately 1.32 billion people (2) live in areas in developing countries where leprosy is an important problem, i.e., where the prevalence is over 10 cases per 10,000 persons and where an individual thus may be considered at significant risk of contracting the disease. More than one third of all leprosy patients face the threat of permanent and progressive physical and social disability. One of the difficulties in properly assessing and monitoring the leprosy problem is that enumeration of cases in many developing countries is incomplete or irregular (Notes of the WHO Inter-Country Meeting of Leprosy Program Managers, Kathmandu, December 1990).
A country that in particular is struggling with this problem is Nepal, with a population of about 19 million and a prevalence rate of 13.6 leprosy patients per 10,000 inhabitants (Notes of the WHO Inter-Country Meeting of Leprosy Program Managers, Kathmandu, December 1990). In addition to these patients, numerous leprosy patients from northern India are crossing the border for free leprosy treatment. For this reason and as agreed between the Government of Nepal and Anandaban Leprosy Hospital, an intensive mass survey was carried out in the Lalitpur District of Nepal from the Spring of 1986 until the Autumn of 1990 in order to: a) collect reliable epidemiological data on leprosy in this area; b) to provide a baseline of relevant data for monitoring the efficacy of the leprosy control program in this area; and c) to assess the indication and feasibility of this type of survey against the leprosy problem in this district.
This was the first and only survey of leprosy on such a scale in Nepal, and was considered by the Government of Nepal to be of paramount importance for developing future strategies for the National Leprosy Control Programme.
Nepal and the Lalitpur District. Nepal is located between longitude 80º-88º.5' east and latitude 26º.30'-30º north (Fig. 1). About 71% of the country is hilly and mountainous. The total population is around 19 million inhabitants with an average annual growth rate of 2.7%, an estimated crude death rate in 1981 of 13.5 per 1000 and an infant mortality rate in 1987- 1988 of 108 per 1000 live births (3). The per capita gross domestic product (GDP) of US$190 (1990-1991) places it among the very poorest countries in the world. Lalitpur District (Fig. 2), one of the 75 districts of Nepal, is located in the central region of Nepal immediately south of Kathmandu, the country's capital. From north to south the district is divided into the flat area of the Kathmandu valley with the city of Patan as the district's administrative center. In the center is a semi-hilly region forming the most southern extensions of the Kathmandu valley (Anandaban Leprosy Hospital is located in this area). In the south there are hills reaching a maximum height of 2831 meters which form the boundary with the Terai, the strip of Indo-Gangetic plain forming the southern part of Nepal bordering India.
Fig 1. Nepal; located at the northern edge of the Indian subcontinent.
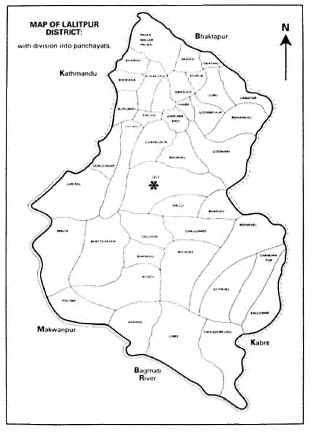
Fig. 2. Lalitpur District with Anandaban Hospital (*) shown in the center of Lele panchyat.
In Lalitpur one can distinguish about 11 different cthno-linguistic groups of Burmese-Mongolian and Indo-Aryan origin. The main languages spoken are Nepali, Newarand Tamang. Until the political changes in 1990, each district in Nepal was divided administratively into panchayats (hereafter renamed as Village Development Committees) which, in turn, were subdivided into wards, and these into villages. The area of Lalitpur District covers 413 sq. km. and has 41 Village Development Committees (VDCs). Each VDC has a health post, and each village is visited by a village health worker.
Since 1956 Anandaban Leprosy Hospital has been one of the two leprosy referral hospitals in the country, and receives patients from all over the country as well from India, Tibet and Bhutan. As per agreement with the Government of Nepal, all medical assistance to leprosy patients is provided free of charge. Anandaban Hospital has 110 beds of which 10 beds are reserved for nonleprosy patients. The main reasons for admission are treatment of leprosy complications that cannot be dealt with at the peripheral level.
Once a week the hospital runs a leprosy outpatient clinic at Patan Hospital (a general hospital at the northern edge of the district), twice a week a combined leprosy and nonleprosy outpatient clinic at Anandaban itself and, since 1991, once bimonthly leprosy clinics at Ghotikhel and Bhattedanda. Attached to the hospital are a training center and the Mycobacterium Research Laboratory. The leprosy eradication program of Anandaban Hospital and the mass survey of Lalitpur District is supervised by and operated in close cooperation with the Leprosy Control Programme of the Government of Nepal.
METHODS
The survey itself was performed by nine male paramedical workers, one of whom was also an experienced physiotherapy technician, another who also was trained as a health educator, and a third as a smear technician. Among them were native Nepali, Newar and Tamang speakers. In the survey of the area close to Anandaban Hospital, a female paramedical worker and a female medical aide were added to the team. In the urban areas females were far more reluctant to be examined by a male paramedical worker, so for the survey of the urban area of Patan eight females were trained and used as paramedical assistants, each working side by side with an experienced male paramedical worker. The field work was supervised by a medical officer trained in epidemiology.
The different areas were surveyed depending on weather conditions; in the monsoon, when traveling on foot was often difficult, the areas accessible by road (mainly the northern and central parts of the district) were visited; in the dry season, the southern parts of the district were surveyed. This was mainly done on foot using porters and tents, and the team frequently was away from the hospital for several weeks. Preceding the survey of a specific area, permission was sought from the VDC leader who, in turn, would mediate in getting the cooperation of the ward leaders. After this was established, health education was given in the form of slide shows, films and open-air talks on leprosy at community centers. Thereafter the survey was conducted in a house-to-house manner, at which all household members were listed and the family structure recorded. The household members present were examined for signs of leprosy by at least two paramedical workers or, in the urban area of Patan, by one experienced paramedical worker and a female paramedical assistant. All suspected and diagnosed cases were seen by a medical officer for confirmation of the diagnosis.
Newly found cases were further examined at the leprosy clinic at Patan Hospital or Anandaban Hospital, at which complete body charting would be done. Nerves prone to be affected would be examined and their qualities with regard to sensation and muscle strength assessed and recorded by the physiotherapy department. Skin smears of three standardized sites and one active skin patch were taken, blood was sampled for serological examination, a lepromin test was performed and, again, health education would be given. After the final decision on the classification of the disease, medical treatment would be started. Those listed as suspect cases were revisited at a later stage or instructed to come for re-examination to the leprosy clinic at either Patan Hospital or Anandaban Hospital.
RESULTS
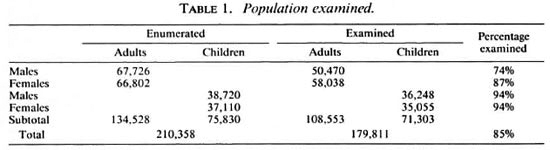
Population examined. The survey provided, at the same time, an accurate census of the population which at the end of the survey appeared to be 210,358. Those up to 15 years of age were counted as children (Table 1).
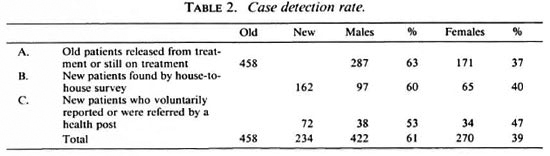
Case detection rate. In the group of 179,811 inhabitants of Lalitpur District who were examined for leprosy, 458 old cases and 232 new cases were found (Table 2). The sex ratio male-to-female was in group A 1.66/1, in group 13 1.36/1, and in group C 1.12/1. Out of the 234 new patients 49 were not registered as taking treatment at Anandaban Hospital by the end of the survey: a) 12 new patients were still unwilling to commence treatment (in spite of repeated visits to motivate them for treatment); b) 8 patients were free of signs and symptoms of leprosy by the time they reported at the clinic and were listed as subsided; c) 21 patients were taking treatment at another center; d) 3 cases had moved out of the district; e) 2 patients died before starting treatment; and 0 1 patient could not be traced back. The number of new patients was therefore set at 232. New patients found in 179,811 people examined gave a 5-year case detection rate of 13 per 10,000 inhabitants examined (2.6 per 10,000 per year).
Child detection rate. In the period 1978-1980 and in the year 1985, a total of 144 schools were surveyed; 33,058 children were examined and a total of 29 new child cases were found. In the 1986-1990 mass survey group of 71,303 children examined, 31 new child cases were found, and the 5-ycar child detection rate was, therefore, 4 per 10,000 (0.8 per 10,000 per year).
Prevalence rate. In 1990 the measured prevalence rate (patients needing antileprosy treatment/population examined) was 6.8 per 10,000. By the end of 1992 this had dropped to 3.1 per 10,000.
Incidence rate. Three VDCs (Lele, Champi and Badiikhel) with a total population of 14,462 were re-surveyed in 1989 after an interval of 3 years; 11,964 people were examined (82.7% of the population) and 4 new patients were found in Lele VDC (3 females and 1 male). Only the male was skin-smear positive (0.1+), and was classified as borderline lepromatous. The 3 females were all smear negative and were classified as 2 borderline tuberculoid and 1 midborderline. The 3-year incidence rate for these three VDCs was, therefore, 3.3 per 10,000 (1.1 per 10,000 per year).
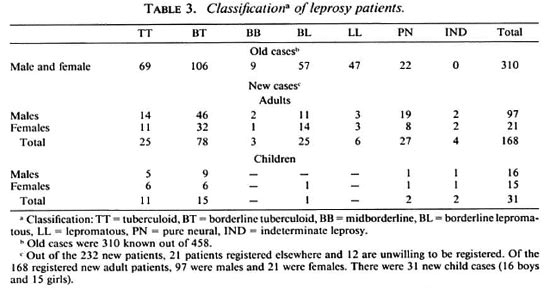
Classification. The classification of the patients registered during the survey is presented in Table 3. Approximately 36% of all old cases, 20% of all new adult patients, and 3% of all new child cases were classified as multibacillary; 20% of all new patients were skin-smear positive, and all of this group of patients were taking multidrug therapy regularly.
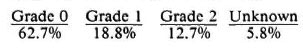
Disability. The disability grading* of hands and feet among new cases was:
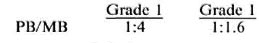
In the total population of leprosy patients of the Lalitpur District the disability ratio for paucibacillary (PI3) patients versus multibacillary (MB) patients was:
Therapy. Of all the patients not yet released from treatment, 82% took multidrug therapy (MDT) as recommended by the World Health Organization (WHO) in 1982 by the end of the survey. Of the remaining proportion, 16% were on dapsone monotherapy and 2% took other medical treatment. By the end or 1992 full MDT coverage had been reached. By 31 December 1992, 644 patients were released from M DT and 56 were still on treatment.
Regularity rate. As per the WHO definition, more than 86% of the patients on MDT took regular treatment by the end of the survey. For those patients taking dapsone monotherapy, 43% were regular. By the end of 1992 full MDT coverage was achieved and 96% of all of our patients were taking regular treatment.
Cost of the survey. The total cost of the intensive mass survey over its 5-year period amounted to Nepali rupees 2,205,667 (about US$71,150 at the exchange rate of January 1991); 70% of this amount was spent on salaries. The approximate cost for detecting one new patient was Nepali rupees 9551.42 (about US$298).
DISCUSSION AND CONCLUSIONS
The percentage of examined people of the Lalitpur District of 85% was sufficient, according to WHO standards, to draw reliable conclusions for an epidemiological assessment of the area. The lower percentage of adult males examined possibly was due to the fact that many of the males have accepted employment away from home. The difference in the sex ratio between the already registered, the newly found cases, and the voluntarily reporting patients perhaps can be explained by the fact that female leprosy patients, in general, are more reluctant to seek medical help. We assume that our intense health education in the district has helped in decreasing the ratio in the last two categories.
The 1986-1990 child detection rate for Lalitpur was 4 per 10,000 over the 5 years or 0.8 per 10,000 per year. One should consider though that in the earlier school surveys almost half of the children of Lalitpur District already had been examined, which may have influenced the proportion of new child cases found at the mass survey. The child rate of the newly detected cases in Nepal was officially 5.57% in 1988-1989. The value of school surveys in low leprosy-endemic areas may be merely in providing a chance to give health education.
The measured prevalence rate in 1990 of 6.8 per 10,000 inhabitants means that by the end of the survey one could speak of leprosy being endemic in the Lalitpur District. Thanks to full MDT coverage and a regularity rate of 96%, the number of patients still needing treatment had decreased greatly by the end of 1992, resulting in a prevalence rate at that point of 3.1 per 10,000. Only a few VDCs have been resurveyed as yet and, therefore, reliable data on the incidence rate are pending.
Of all newly detected cases the MB rate was 20%; for the whole of Nepal this was 45% for the years 1988-1989. Fourteen percent of all our new patients were classified as having pure neural leprosy; for the whole of Nepal this was 7%. The difference may be explained by the fact that we developed a new technique for diagnosing this form of leprosy. The method was called "cytological needle aspiration of nerve fluid for the diagnosis of pure neural leprosy" and enabled us to simply screen the nerve for acid-fast bacilli (1).
Overall 62.7% of the patients had no disability, 18.8% had disability grade 1 and 12.7% had disability grade 2; while for 5.8% the data were incomplete. In the Western Region of Nepal a disability grade 2 was found in about 16% of all new cases. For the whole of Nepal (Notes of the WHO Inter-Country Meeting of Leprosy Program Managers, Kathmandu, December 1990), grade 1 was 18% and grade 2 was 12% in 1988-1989. At the end of the survey, 86% of all registered Lalitpur patients took MDT regularly; by the end of 1992 this had increased to 96%. For the whole of Nepal, 52% of the patients took MDT in 1990 (2).
The differences with regard to the MB rate, disability grades, and the proportion of patients on MDT between the Lalitpur District data and the data for the rest of Nepal can be explained by the fact that the mass survey in Lalitpur made early case detection and control feasible. Loss of sensation in the extremities is often the first symptom motivating patients to seek medical help. Intense health education, also employing "cured" patients and early case finding, is needed to diagnose new cases before nerve damage has occurred.
The difference in the regularity rate between patients taking MDT and monotherapy was explained by the fact that the monotherapy group mainly consists of patients living in the relatively inaccessible southern part of the district from where they have to walk for several days to collect their medicines. For this reason, two bimonthly clinics were opened in the villages of Bhattedanda and Ghotikhel in 1991.
One has to be cautious in extrapolating Lalitpur data to the situation in other hill districts in Nepal. Anandaban Hospital, being one of the two leprosy referral hospitals in the country, is located in the heart of Lalitpur District and has been providing assistance to leprosy patients of this district for more than 30 years.
The costs of Nepali rupees 9951.42 (US$298) for the detection of each new leprosy case in Lalitpur District stands in sharp contrast with the amount of Nepali rupees, 44.00 per person, that the Nepali Government had available for health care in 1992.
Plans are prepared to re-survey the 10 VDCs with the highest prevalence within 2 years of the last survey in order to monitor the 2-year incidence, multibacillary rate, child rate and deformity rate. These will be used as key parameters to assess the success of the leprosy control program in the district.
All contacts of already diagnosed cases will be kept under surveillance. Health education will be continued and combined with radio spots on leprosy. Patient self-care will be further stimulated while the facilities for rehabilitation are reinforced. Irregular patients and defaulters will continue to be followed up.
Based upon our experiences gained by this survey, we came to the following recommendations:
Infrastructure. Adequate training of health post staff and village health workers and the handing out of drugs through the health posts may improve compliance and the earlier detection of nerve damage. Clinical facilities providing possibilities for, e.g., the treatment of immune reactions, foot problems, reconstructive surgery, eye care, and a rehabilitation program should be available in the region since this will stimulate patients to comply with medical treatment.
Medical. Disability prevention and control should receive the same priority and timing as the implementation of MDT. The old WHO disability grading (grade 0 to 3) offers more realistic parameters than the present one (grade 0 to 2) in assessing the outcome of the disability prevention and control program and, to some degree, by this the success of patient self-care.
Finance. An intensive mass survey as conducted in Lalitpur District serves well as a scientific study, but the cost per newly detected patient renders it far too expensive for an area with such a low prevalence rate. More than 30% of the new cases were referred or self-reporting. For this reason in hilly regions like Lalitpur with a prevalence of < 10 per 10,000 only flash surveys combined with intense health education should be done. For all these activities it is of great benefit to employ staff who are familiar with or originate from a population similar to the one to be surveyed.
Acknowledgment. Thanks to the great efforts made by all field staff, often under very' difficult conditions, this survey was successfully completed.
REFERENCES
1. THEUVENET, W. J., MIYAZAKI, N., ROCHE, P. and SHRESTHA, I. Cytological needle aspiration of the nerve for the diagnosis of pure neural leprosy. Int. J. Lepr. 61(1993) 597-599.
2. WHO EXPERT COMMITTEE ON LEPROSY. Sixth report. Geneva: World Health Organization, 1988. Tech. Rep. Ser. 768.
3. WORLD HEALTH ORGANIZATION. Health Care in South-East Asia. New Delhi: World Health Organization 1989. S.E. Asia Ser. 14.
1. M.D., former Medical Superintendent and Plastic and Reconstructive Surgeon. Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
2. M.D., Senior Medical Officer and Surgeon. Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
3. M.D., S.Gr. Medical Officer. Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
4. M.B.B.S., B.Sc, S.Gr. Medical Officer. Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
5. Senior Paramedical Worker. Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
6. Paramedical Worker, Physiotechnician. Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
7. M.B.B.S., B.Sc; Administrative Superintendent, Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
8. M.B.A., Administrative Superintendent, Anandaban Hospital, The Leprosy Mission, Tikah Bhairab, Lalitpur, Nepal.
9. M.B.B.S., Dermatologist, Chief of Leprosy Control Programme of the Government of Nepal.
10. M.D., Ph.D., Epidemiologist, Head, Evaluation Unit, The Leprosy Mission, Singapore.
Reprint requests to Dr. W. J. Theuvenet, Consultant for Plastic, Reconstructive and Hand Surgery, Lukas Hospital, P.O. Box 9014, 7300 DS Apeldoorn, The Netherlands.
Received for publication on 6 September 1993.
Accepted for publication in revised form on 17 February 1994.
* Present WHO disability grading system as recommended in 1980 for hands and feet: Grade 0 = no anesthesia, no visable deformity or damage; Grade 1 = anesthesia present but no visable deformity or damage; Grade 2 = visable deformity or damage present.