- Volume 62 , Number 2
- Page: 220–4
Paralysis of facial muscles in leprosy patients with lagophthalmos
ABSTRACT
The objective of the study was to determine the pattern of involvement of facial muscles in lagophthalmos. Fifty-seven patients with lagophthalmos were examined to assess the degree of paralysis of facial muscles. Eighty-one percent of the patients with lagophthalmos had involvement of at least one other muscle group. In patients with lagophthalmos with a gap at mild closure of 5 mm or more, 27 of 30 (90%) had involvement of at least one other facial muscle. In lepromatous leprosy the pattern of involvement was symmetrical and "patchy," the right and left sides being affected equally. In tuberculoid leprosy, the ipsilateral muscles were more often involved, which is the pattern of involvement of a nerve trunk. The upper and lower facial muscles were affected in the same proportion. Hence, on clinical grounds, there is little support for the often postulated statement that the superficial course of the facial nerve above the zygomatic bone is decisive for exclusive paralysis of the zygomatic branch of the facial nerve.RÉSUMÉ
L'objectif de cette étude était de déterminer le mode d'implication des muscles faciaux dans le lagophtalmos. Cinquante-sept patients avec un lagophtalmos ont été examinés pour estimer le degré de paralysie des muscles faciaux. Quatre-vingt-un pourcents des patients avec lagophtalmos avaient au moins un autre groupe musculaire impliqué. Chez les patients qui avaient un lagophtalmos avec une fente de 5 mm ou plus à la fermeture légère des yeux, 27 sur 30 (90%) avaient au moins un autre muscle facial impliqué. Dans la lèpre lépromateuse, le mode d'implication était symétrique et "en taches," les côtés gauche et droit étant également affectés. Dans la lèpre tubereuloide, les muscles ipsilatéraux étaient plus souvent impliqués, ce qui est le mode d'implication d'un tronc nerveux. Les muscles faciaux supéricurset inférieurs étaient affectés dans la même proportion. Donc, sur base clinique, il y a peu d'arguments en faveur de l'affirmation souvent admise que le parcours superficiel du nerf facial au-dessus de l'os zygomatique est décisif pour la paralysis exclusive de la branche zygomatique du nerf facial.RESUMEN
El objetivo de este estudio fue el determinarei patrón de la afección de los músculos faciales en el lagoftalmos. Se examinaron 57 pacientes con lagoftalmos para establecer el grado de parálisis de los músculos faciales. Ochenta y uno por ciento de los pacientes con lagoftalmos tuvieron afección de al menos un nervio de cada grupo. El 90% (27 de 30) de los pacientes con lagoftalmos con un espacio (un gap) al cierre moderado de 5 mm o más, tuvieron afección de cuando menos uno de los músculos faciales. En la lepra lepromatosa el patrón de afección fue simétrico y "en parches," afectándose de igual manera tanto el lado derecho como el izquierdo. En la lepra tubereuloide los músculos ipsilaterales fueron los más frecuentemente afectados; ésto corresponde al patrón de afección de un tronco nervioso. Los músculos faciales superior e inferiorestuvieron afectados en el mismo grado. Según estas observaciones, clínicamente hay poco apoyo a la consideración, frecuentemente mencionada, de que el curso superficial del nervio facial sobre el hueso zigomático es decisivo para la parálisis exclusiva de la rama zigomática del nervio facial.The main dangers for the eye in leprosy are lagophthalmos, corneal hypesthesia and iridocyclitis (6). Lagophthalmos can be found in all types of leprosy. On the lepromatous side of the spectrum nerves are damaged by direct infiltration by Mycobacterium leprae. In the tuberculoid type of leprosy the nerve damage is caused by granulomatous inflammation. Most lagophthalmos cases are, however, the consequence of type 1 leprosy reactions ("reversal reaction") in borderline (BT, BB, BL) leprosy patients. The presence of patches around the eye, together with a type 1 leprosy reaction, is a severe risk for the development of lagophthalmos in borderline leprosy (5). This nerve damage may be reversible if treated promptly with steroids, preferably within 6 months (1,7).
In the literature not much attention has been paid to the paralysis of other facial muscles in leprosy. It is often stated that the zygomatic branch of the facial nerve which supplies the orbicularis oculi muscles is most affected because of the superficial location of this branch (2,4).
Studying the paralysis of facial muscles has some special problems. Paralysis of the frontalis muscle does not cause inconvenience to the patient. The discomforts of the paralysis of the buccinator muscle and the orbicularis oris muscle in the form of drooling and difficulty with speech appear only late in the development of the paralysis. All of the muscles contribute to facial expression, which is an important part of communication. Examination of a partial paralysis of the facial muscles is more difficult than the voluntary muscle testing of the hand and feet muscles, so it is hard to assess objectively. There are several scoring systems for facial paralysis but they are not very useful for leprosy (11).
In our study wc investigated the hypothesis, based on clinical impression, that in every clinically significant lagophthalmos other facial muscles also are involved. This was done by studying the pattern of involvement of the facial muscles in different types of leprosy.
SUBJECTS AND METHODS
During a 10-week period in September-November 1992 we examined patients with lagophthalmos presenting at the regional leprosy clinic in Biratnagar and in the five monthly mobile clinics in different districts in eastern Nepal. Patients in these clinics come from the terai (lowland) belt of Nepal, and many patients come from Bihar State in India. Most of the patients were presenting for their monthly multidrug therapy. Some patients were newly diagnosed patients. Others had been released from treatment and presented with some complaint. The registration number, age and sex, classification of leprosy, type and duration of treatment, duration of disease, duration of lagophthalmos, and a possible history of the use of steroids were noted.
We examined the lagophthalmos with a transparent ruler by measuring the gap at straight gaze, mild closure ("as if in sleep" or with slow closing), and strong closure. Only patients with a lagophthalmos of > 1 mm on mild closure were included in this study. We noted the amount of cornea left exposed in mild closure (an indicator of the protective Bell's phenomenon).
Where possible, we drew facial patches on a diagram. Of the facial muscles, we tested the orbicularis oculi, the frontalis, the orbicularis oris, and the buccinator muscles by asking the patient, respectively, to close her/his eyes (as if in sleep and strongly), to frown, to make a snout, to blow up the cheeks and to smile (Figs. 1-3 are some examples). The movements were observed for asymmetry, and the muscles were palpated to perform a grading in which 1 is normal, 2 is slightly but convincingly weak, 3 is obviously weak. Except in clear-cut cases, slides were made of the different "grimaces" for a second opinion to diminish observer bias. In case of doubt the grading was 1 (normal).
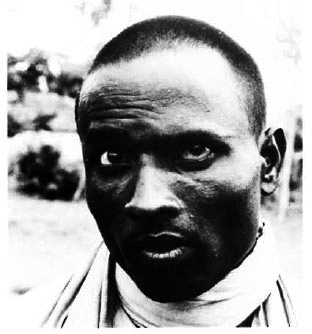
Fig. 1. Frowning: paresis of left fontalis muscle inpatient with right-sided lagophthalmos.
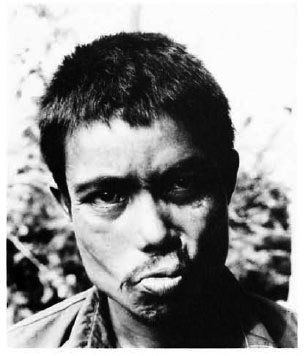
Fig. 2. Making a snout: paresis of left orbicularisoris muscle in patient with left-sided lagophthalmos.
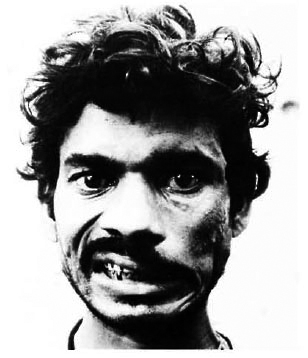
Fig. 3. Showing the teeth: paresis of left buccinatormuscle in patient with left-sided lagophthalmos.
For statistical analysis the statistical program SPSS-PC was used.
RESULTS
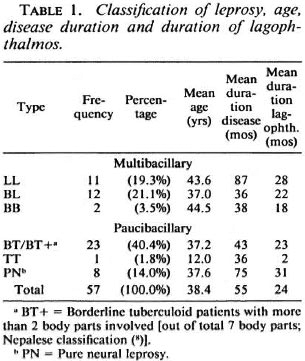
A total of 57 patients were found to have lagophthalmos. Among them were 9 new patients and 3 patients released from treatment; 50 patients were male, 7 female; 25 patients had multibacillary (MB) leprosy (LL, BL, BB) and 32 patients had paucibacillary (PB) leprosy [BT+ (BT with > 2 body parts involved), BT, TT, PN (pure neural)] (2). The mean age was 38.4 years (40.5 years for MB leprosy, 36.7 years for PB leprosy). The mean duration of disease was 55 months (60 for MB, 51 for PB). The duration of the lagophthalmos was known in 52 cases, the mean being 24 months for both MB and PB; in 17.4% the duration was 6 months or less.
In Table 1 the findings for the whole group and for the different types of leprosy are summarized. Of the 57 patients 44 (17 MB, 27 PB) had unilateral lagophthalmos and 13 (8 MB, 5 PB) had bilateral lagophthalmos.
Thirty (52.6%) patients had "clinically significant lagophthalmos" with a gap on mild closure of 5 mm or more, 25 (8 MB, 17 PB) unilateral, and 5 (3 MB, 2 PB) bilateral. In 6 (3 MB, 3 PB) patients (10.5%), a tarsorrhaphy had been done on one or both eyes. In 21 patients (36.8%; 12 MB, 9 PB) the cornea remained exposed on mild closure; in two of them in both eyes.
The number of affected muscles in the group of lagophthalmos patients is indicated in Table 2. The number of affected facial muscles in individual patients is indicated in Table 3.
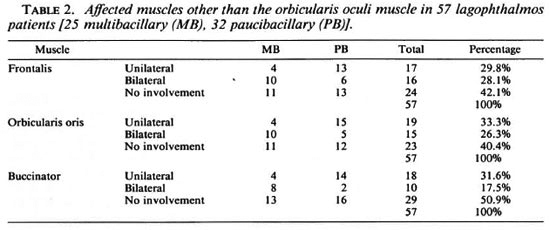
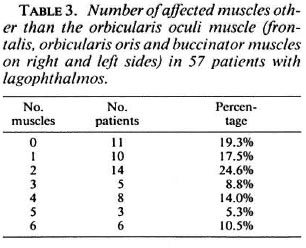
In 11 cases of lagophthalmos (19.3%) there was no weakness of any of the facial muscles except the orbicularis oculi muscle (6 MB, 5 PB).
In clinically significant unilateral lagophthalmos only 3 out of 25 cases (12%) demonstrated no involvement of any of the facial muscles on the same side.
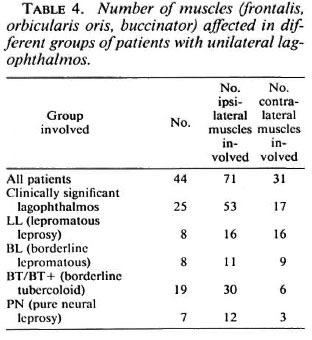
If we look at the number of muscles affected in unilateral lagophthalmos in the groups with a different classification separately, it becomes clear that in LL and BL leprosy cases there is a symmetrical pattern of paralysis and in BT/BT+ cases there is an asymmetrical pattern: the facial muscles on the side of the lagophthalmos are much more often involved than the contralateral side (12). These results are summarized in Table 4.
DISCUSSION AND CONCLUSIONS
Fifty-seven patients were found to have lagophthalmos, giving a group large enough to analyze. The mean duration of the disease was less than 5 years (54.5 months) and the mean duration of the lagophthalmos was nearly 2 years (23.8 months), both relatively short time periods. The group presented here is different from inpatient groups used in other studies (3, 8, 9).
We found that the tested facial muscles both "upper" and "lower" were affected to the same degree. The frontalis and the orbicularis oris muscles are involved in 57.9% and 59.6% of the patients (Table 2). We did not find that impaired power of the "deep" buccinator muscle (in 49.1 % of the patients) is much less common than weakness of the other muscles (Table 2). Complete paresis of facial muscles is exceptional, and in old patients weakness is more difficult to establish because it might be physiological. In LL patients it is sometimes difficult to confirm symmetrical but mild paralysis and diminished facial expression because of wrinkling of the skin. This probably implies that the real number of involved muscles may be higher, especially in LL patients.
Table 4 shows the symmetrical involvement of facial muscles in lepromatous leprosy and the asymmetrical, ipsilateral involvement in BT/BT+ cases, suggesting involvement of mainly one nerve trunk. There is little clinical indication that the superficial course above the zygomatic bone is decisive. In this study there is, of course, a selection bias for the examination of facial muscles because we only examined lagophthalmos patients. We did not study partial paralysis of the facial muscles without involvement of the orbicularis oculi muscle.
The observation that not only the zygomatic branch is involved in nerve damage of the facial nerve can be explained in several ways. The course of most of the nerve beyond the parotid gland is quite superficial. As stated before, the main factor in developing nerve damage in borderline leprosy is type 1 leprosy reaction. There is a strong relation between lagophthalmos and location of the patches (5). In BT the pattern is unilateral and sometimes bilateral, depending on the location of the reaction patches. In PN there seems to be the same pattern. Thus, in large patches the other branches of the facial nerve are also involved. This may be explained by anastomoses between the fifth and seventh cranial nerve (4). In lepromatous leprosy the development of lagophthalmos is not a result of type 1 leprosy reaction but, rather, the result of (symmetrical) diffuse infiltration and secondary atrophy, not only in the branches of the facial nerve but also within the muscles themselves (10). This is in agreement with the long duration of disease in our LL patients.
The significance of calling attention to facial muscles other than the orbicularis oculi is that an asymmetry in or weakness of facial expression can call attention to a facial nerve in reaction and allow prompt action to preserve sight. We hope to have demonstrated that lagophthalmos in leprosy is not an isolated event.
REFERENCES
1. BECX-BLEUMINK, M. , BERHE, D. , AND 'T MANNETJE, W. The management of nerve damage in the leprosy control services. (Editorial) Lepr. Rev. 61(1990)1-11.
2. BRAND, M. E. and FFYTCHE, T. J. Eye complications of leprosy. In: Hastings R. C , ed. Leprosy. Edinburgh: Churchill Livingstone, 1985, p. 224.
3. COURTRIGHT, P., GREEN, R., PILANSKI, R. and SINVENY, J. A survey of the eye complications of leprosy in South Korea. Lepr. Rev. 55( 1984)229-237.
4. DASTUR, D. K., ANTIA, N. H. and DIVEKAR SC. The facial nerve in leprosy 2. Pathology, pathogenesis, electromyography and clinical correlations. Int. J. Lepr. 34(1966)118-138.
5. HOGEWEG, M., KIRAN, K. U. and SUNEETHA, S. The significance of facial patches and type I reaction for the development of facial nerve damage in leprosy. A retrospective study among 1226 paucibacillary leprosy patients. Lepr. Rev. 62(1991)143-149.
6. JOFFRION, V. C. and BRAND, M. E. Leprosy of the eye-a general outline. Lepr. Rev. 55(1984)105-114.
7. KIRAN, K. U., HOGEWEG, M. and SUNEETHA, S. Treatment of recent facial nerve damage with lagophthalmos, using a semistandardized steroid regimen. Lepr. Rev. 62(1991)150-154.
8. MALLA, O. K., BRANDT, F. and ANTEN, J. G. F. Ocular findings in leprosy patients in a institution in Nepal (Khokana). Br. J. Ophthalmol. 65(1981)226-230.
9. REICHART, P. A., SRISUWAN, S. and METAH, D. Lesions of the facial and trigeminal nerve in leprosy. Int. J. Oral Surg. 11(1982)14-20.
10. SLEM, G . Clinical studies of ocular leprosy. Am. J. Ophthalmol. 71(1971)431-434.
11. SMITH, I. M., MURRAY, J. A. M. , CULL, R. E. and SLATTERY, J. S. A comparison of facial grading systems. Clin. Otolaryngol. 17(1992)303-307.
12. VAN BRAKEL, W. H., DE SOLDENHOFF, R. and MCDOUGALL, A. C. The allocation of leprosy patients into paucibacillary and multibacillary groups for multidrug therapy, taking into account the number of body areas affected by skin, or skin and nerve lesions. Lepr. Rev. 63(1992)231-246.
1. M.D.; State University of Groningen, Groningen, The Netherlands.
2. M.D.; Ophthalmologist, Department of Ophthalmology, State University of Leiden and Consultant Ophthalmologist, Netherlands Leprosy Relief Organization (NSL), Wibautstraat 135, 1097 DN Amsterdam, The Netherlands.
3. M.B., Ch.B. D(Obst.), R.C.O.G., D.T.M&H., M.R.C.G.P.; Project Leader, NSL/Eastern Leprosy Control Project, P. O. Box 134, Biratnagar, Nepal. Reprint requests to: Dr. M. Hogeweg, Department of Ophthalmology, Leiden University, P. O. Box 9600, 2300 RC Leiden, The Netherlands.
Received for publication on 5 November 1993.
Accepted for publication in revised form on 2 March 1994.