- Volume 62 , Number 2
- Page: 295–6
Lepromatous leprosy and HIV infection
To the Editor:
The patient is a 19-year-old heterosexual male with a history of intravenous drug abuse since the age of 15. He is a resident of Buenos Aires, Argentina.
In June 1991 the patient developed erythema nodosum leprosum (ENL). The ENL improved with corticosteroid therapy which the patient self-administered without consulting a physician. In January 1992 he was admitted to the hospital with a reactional episode characterized by ENL, some of which resembled erythema multiforme lesions, and severe bilateral ulnar neuritis with nerve enlargement, tenderness, and loss of function.
Electromyography at that point showed a severe left ulnar sensory neuropathy and a moderate right ulnar motor loss. Skin smears from cutaneous lesions and nasal scrapings were positive for acid-fast bacilli (AFB) with a bacterial index (BI) of 2 + . Skin biopsies from lesions showed ENL and were positive for AFB. The patient tested positive for HIV infection by ELISA, confirmed by Western blot. The patient's serum was negative for antigenemia. The peripheral blood CD4 + count was 1563/mm3.
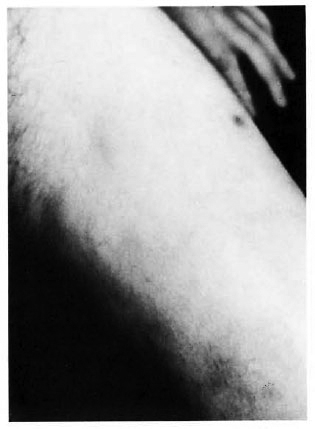
Fig. 1. Macules and nodules on the thigh.
The patient was treated with daily rifampin 600 mg, clofazimine 50 mg, dapsone 100 mg, and prednisolone 80 mg. After slight improvement the prednisolone was gradually tapered. When the dose reached 40 mg daily, the patient again developed neuritis with impaired neural functioning. At that point, the clofazimine was increased to 300 mg daily while the prednisolone was again gradually tapered. After 3 months the patient's prednisolone could be discontinued.
Although the antiinflammatory effect of large doses of clofazimine is well known, the drug may be even more important for a patient with reactions with leprosy and HIV infections. In these cases the possible adverse effects of corticosteroid therapy on the course of the HIV infection by causing immunodeficiency may be particularly important.
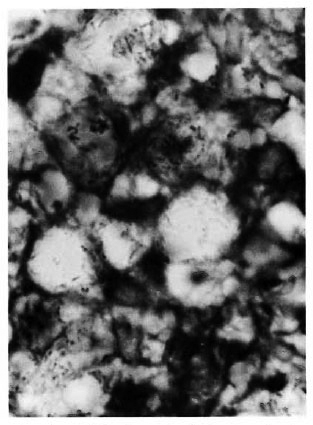
Fig. 2. Ziehl-Neelsen stain of skin biopsy showing numerous acid-fast bacilli in vacuolated cells in the dermis.
- L. M. Olivares
Dermatology Department Staff
- G. E. A. Pizzariello
Dermatology Department Chairman
- J. Benctucci
AIDS Department Chairman
- M. H. Farina
Leprosy Unit Chairman
- C. Kien
Pathologist
- A. Btesh
Dermatology Department Resident
Muniz Hospital
Buenos Aires, Argentina
Reprint requests to Dra. L. M. Olivarcs, Av. Callao 2036, 14A, Buenos Aires 1024, Argentina.