- Volume 62 , Number 1
- Page: 32–6
Lymphangiographie evaluation of patients with clinical lepromatous leprosy on clofazimine
ABSTRACT
Pedal edema as a possible adverse effect of clofazimine therapy in leprosy was first reported in 1990. Raasch, et al. reported their lymphangiography findings on ten patients who had clinical lepromatous leprosy in 1969. None of these patients had been on clofazimine therapy. Our study, therefore, was designed to assess the changes that might be seen in the lymphatic system of patients treated with clofazimine for the management of leprosy. Our findings are compared with those of Raasch and his colleagues.RÉSUMÉ
Un oedème en pédale comme effet secondaire possible du traitement à la clofazimine dans la lèpre a été rapporté pour la première fois en 1990. Raasch et al. ont rapporté leurs observations lymphangiographiques sur 10 patients qui avaient une lèpre lépromateuse clinique en 1969. Aucun de ces patients n'avait été sous traitement à la clofazimine. Notre étude, dès lors, a été conçue pour évaluer les modifications qu'on pourrait observer dans le système lymphatique de patients traités à la clofazimine pour la lèpre. Nos observations sont comparées à celles de Raasch et de ses collègues.RESUMEN
El edema del pie como un posible efecto adverso del tratamiento de la lepra con clofazimine fue reportado por primera vez en 1990. Raasch, et al., publicaron en 1969 sus hallazgos linfangiográlicos en 10 pacientes que tenían lepra lepromatosa clínica. Ninguno de éstos habia sido tratado antes con clofazimina. El presente estudio se diseñó con objeto de establecer los cambios que podrían observarse en el sistema linfático de los pacientes con lepra tratados con clofazimina. Nuestros hallazgos se comparan con aquellos de Raasch y sus colaboradores.Lymphangiography, the radiographic demonstration of the lymphatic system using contrast material, is an accepted, useful and recognized procedure to visualize the lymphatic system (8-12, 19). The procedure was designed by Kinmonth and has been modified by Jackson, et al. (8) and Cahill and Kaiser (3).
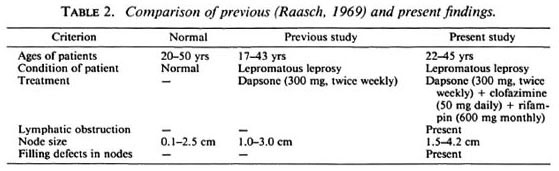
Several studies have been done to show the changes seen in the lymph nodes as a result of leprosy (5-7, 18). The changes that are found in the lymphatic vessels as a result of the disease also have been reported (14). In 1969 Raasch, et al. reported their findings on lymphangiograms done on 10 patients with lepromatous leprosy (17). They also analyzed the extent of involvement of the lymphatic system on the basis of histopathological and lymphangiographic studies. None of the 10 patients studied by Raasch had been on clofazimine therapy.
Clofazimine, a rhiminophenazine dye which is used as a first-line drug in the management of leprosy and lepra reactions, has a tendency to get trapped in lymph nodes and cells of the reticuloendothelial system (1, 4). Involvement of the lymph nodes due to the drug also has been demonstrated histopathologically (13), but the involvement of the lymphatic system has not been demonstrated.
In 1990 an initial report of lymphedema as a possible adverse effect of clofazimine therapy in leprosy was made (15). It was observed that the pedal edema in some patients had become symptomatic and significant after the chemotherapy with clofazim inc had been started. None of the patients reported to have had any history of reactions or plantar ulcerations nor did they have any history of intercurrent illnesses. Baseline investigations done on these patients ruled out the presence of organic illnesses. A second report based on a study of 75 patients was published in 1991 (16).
Our present study, therefore, was designed to determine whether clofazimine could cause lymphatic stasis and, if so, the nature and extent of involvement of the lymphatic system in patients who were on the drug for the management of leprosy.
METHODOLOGY
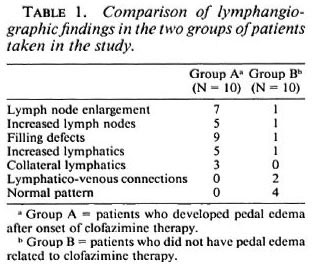
Twenty patients who had been on clofazimine therapy for management of leprosy were selected for the study. Their hematological, biochemical and bacteriological profiles were analyzed to attempt to rule out the possibility of any organic illness that could have caused pedal edema. They also were screened for a history of reactions and steroid therapy and the presence of plantar ulcers. The patients were divided into two groups: 10 who had significant and symptomatic pedal edema which was subjectively observed only after the onset of chemotherapy, and 10 who did not have any demonstrable pedal edema related to clofazimine therapy. With informed consent lymphangiograms were performed on the right lower limb of each patient following the procedure of Kinmonth. These findings were tabulated and compared with those of Raasch, et al. (17). The lymphangiograms were read blind. The observations of the lymphangiograms done on these two groups are tabulated in Table 1 and compared with the findings of Raasch, et al. in Table 2. Only one patient had a minor secondary wound infection which was managed with a course ofantibiotics. The laboratory investigations done on these patients did not reveal any other illnesses or conditions that could have contributed to the pedal edema.
DISCUSSION
Lymph node enlargement due to leprosy has been well documented, and the histopathological profile also has been studied in great detail (6, 7, l8). In this study fine needle aspiration cytology was indicated but could not be done due to the paucity of resources. The findings of Raasch, et al. (17) suggest the possibility that lymph node enlargement occurs with patients who have clinical lepromatous leprosy. None of the patients studied by them were reported to have pedal edema. The enlargement of the lymph nodes in the patients in the present study when compared with those in the previous Raasch study suggests that the enlargement of the lymph nodes present in the former group could be due to the presence of clofazimine in the lymphatic system (Table 1). This could also explain the tendency for the nodes of patients in our present study to show filling defects, increases in the number of lymphatics draining the nodes and also an increasing number of lymph nodes in these patients, with a few patients presenting with collateral lymphatic drainage.
Two patients in group B showed lymphatico-venous connections. Both had a previous history of type 2 reactions and had been on clofazimine 300 mg daily for control of their reactional states. It was interesting to observe that neither of these patients had any demonstrable pedal edema related to clofazimine therapy or type 2 reactions. This could perhaps have been due to the presence of the lymphatico-venous connections which could have drained the region.
It is also interesting to observe that none of the patients who had been on clofazimine and showed pedal edema after the onset of chemotherapy had a normal pattern of lymphatic drainage. One patient, for unknown reasons, showed an elevated total serum protein (9.3 g%, normal 4.5 to 7.5 g%) and slightly elevated transaminase levels (AST or SGOT of 38 mg%, normal < 35 mg%; ALT or SGPT of 35 mg%, normal < 35 mg%). This patient also had pedal edema following the onset of chemotherapy. Since he was otherwise asymptomatic and showed no signs of organic disease involvement, he was included in the study.
Clofazimine has a tendency to get trapped in the lymph nodes and cells of the reticuloendothelial system (4). The presence of the drug within the lymph nodes has been demonstrated even up to 5 years after the drug has been discontinued (1, 7 ). One case of unnecessary laparotomy for an acute abdomen was reported, in which the only significant finding on laparotomy was an enlarged and caseated mesenteric lymph node which was filled with the crystals of the drug (2). The observation that the drug is also found in the cortex of the nodes suggests that the drug reaches the nodes through the lymphatic route and not by a hematogenous route. There is therefore the possibility that after the drug enters the lymph nodes it crystallizes within the nodes and thereby prevents lymphatic flow.
This impedance of lymphatic flow is clinically likely to be manifested by pedal edema. The fact that none of the patients in our study had any significant laboratory or clinical finding that could suggest any other cause of pedal edema suggests that this pedal edema seen in these patients could be caused by lymphatic stasis that could be due to the deposition of the drug in the lymph nodes or lymphatic channels. The lymphangiographic findings of enlarged nodes (Fig.1), filling defects within the nodes (Fig. 2), lymphatic blockade and, in some cases, the presence of collateral channels (Fig. 3) indicate the possibility that the lymphatic stasis is due to the deposition of the drug within the lymph nodes. This corroborates with the kinetics of the drug as reported by Banerjee, et al. (1) and Mansfield (13).

Fig. 1. Patient developed pedal edema after onset of multidrug therapy for multi bacillary leprosy. Lymphangiography shows enlarged inguinal lymph node.

Fig. 2. Patient developed pedal edema after onset of multidrug therapy for multibacillary leprosy. Lymphangiography shows presence of collateral lymphatic vessels and an increase in number of lymphatics.

Fig. 3. Patient developed pedal edema after onset of chemotherapy for multibacillary leprosy. Lymphangiography shows filling defect (central) in the inguinal lymph node.
One patient showed shadows suggestive of gallstones. Since gallstones have been reported in one case to contain clofazimine crystals (13) the possibility of cholelithiasis caused by clofazimine in this patient cannot be ruled out.
In conclusion, the lymphangiographic findings viewed in the context of the pharmacokinetics of the drug indicate that it is quite likely that clofazimine administered to patients with lepromatous leprosy could cause alterations in the pattern of lymphatic drainage. This variation in the lymphatic drainage can, in some cases, be demonstrated by the presence of pedal edema. The drug can affect the lymphatic system to such an extent as to cause nodal filling defects, lymph node enlargements, lymph channel hypoplasia or lymphatic obstruction, with subsequent formation of collateral lymphatic circulation.
It was not possible to assess whether the pedal edema would reverse if the drug were stopped, since this would raise the ethical issue of discontinuation of chemotherapy in these active lepromatous leprosy patients and also raise the risk of drug resistance. Moreover, it was considered that the drug could be present in the lymph nodes even a few years after its being discontinued and, therefore, it would take a very long time before any changes in the status of the edema would be observed.
Acknowledgment. The authors are grateful to The Leprosy Mission and the Presbyterian Church (U.S.A.) for the financial grant received to do the study, and to Ciba Geigy, Switzerland, for the supply of clofazimine used in this study. The expert comments of Prof. Paul Turner, Professor of Clinical Pharmacology, St. Bartholomew's Hospital, London, U.K.; Prof. T. J. Ryan, Churchill Hospital, U.K. and Prof. A. C. McDougall, former editor of Leprosy Review, have been highly valued.
REFERENCES
1. BANERJEE, D. K., ELLARD, G. D., GAMMON, P. T. and WATERS, M. F. R. Some observations on the pharmacology of clofazimine. Am. J. Trop. Med. Hyg. 23(1974)1110-1115.
2. BRYCESON, A. Unnecessary laparotomy for abdominal pain and fever due to clofazimine. Lepr. Rev. 50(1979)258-259.
3. CAHILL, K. M. and KAISER, R. L. Lymphangiography in bancroftian filariasis. R. Soc. Trop. Med. Hyg. 58(1964)358-362.
4. CONALTY, M. L., BARRY, V. C. and JINA, A. The antileprosy agent B-633 and the reticuloendothelial system. Int. J. Lepr. 39(1962)479-484.
5. DESIKAN, K. V. and JOB, C. K. Leprosy lymphadenitis: demonstration of tuberculoid lesions. Int. J. Lepr. 34(1966)147-154.
6. DESIKAN, K. V. and JOB, C. K. Lymph nodes in leprosy. Int. J. Lepr. 36(1968)32-39.
7. FURNISS, A. L. The lymph glands in leprosy. Int. J. Med. Sci. 7(1953)475-481.
8. JACKSON, L., WALLACE, S. and SCHAFFER, B. The diagnostic value of lymphangiography. Ann. Int. Med. 54(1961)870-882.
9. KINMONTH, J. B. Lymphangiography in man. Clin. Sci. II (1953)13-15.
10. KINMONTH, J. B. Lymphangiography in clinical surgery and particularly in the treatment of lymphoedema. Ann. R. Coll. Surg. Engl. 15(1954)300-310.
11. KINMONTH. J. B., TAYLOR G. W. and HARPER, K. Lymphangiography: techniques for its use in lower limbs. Br. Med. J. 1(1955)940-945.
12. KINMONTH, J. B., TAYLOR, G. W., TRACEY, G. D. and MARSH, J. D. Primary' lymphoedema: clinical and lymphangiographic studies of a scries of 107 patients in whom the lower limbs were affected. Br. J. Surg. 45(1960)1-12.
13. MANSFIELD, R. E. Tissue concentrations of clofazimine (B-663) in man. Am. J. Trop. Med. Hyg. 23(1974)1116-11 19.
14. MUKHERJEE, A., RADHEY, S. M. and WAYNE, M. M. An electron microscopic study of lymphatics in the dermal lesions of human leprosy. Int. J. Lepr. 57(1989)507-510.
15. OOMMEN, T. Clofazimine-induced lymphoedema. (Utter) Lepr. Rev. 61(1990)289.
16. OOMMEN, T., NATU, M. V. and WILFRED, D. Clofazimine-induced Iymphocdema: comment. Lepr. Rev. 62(1991)341-342.
17. RAASCH, F. O., CAHILL, K. M. and HANNA, L. K. Histologic and lymphangiographic studies in patients with clinical lepromatousleprosy. Int. J. Lepr. 37(1969)382-388.
18. SHARMA, K. D. and SHRIVASTAV, J. B. Lymph nodes in leprosy. Int. J. Lepr. 26(1958)41-51 .
19. WALLACE, S., JACKSON, L., SCHAFFER, B., GOULD, J., GREENING, R. R., WEISS, A. and KRAMER, S. Lymphangiograms: their diagnostic and therapeutic potential. Radiology 76(1961)179-199.
1. B.Sc, M.D.; Department of Pharmacology; Department of Dermatology, Christian Medical College, Ludhiana 141008, Punjab, India.
2. M.D., M.A.M.S.,Department of Pharmacology; Department of Dermatology, Christian Medical College, Ludhiana 141008, Punjab, India.
3. M.D., M.A.M.S., Department of Radiology; Department of Dermatology, Christian Medical College, Ludhiana 141008, Punjab, India.
4. M.D., Dip.N.B., Department of Dermatology, Christian Medical College, Ludhiana 141008, Punjab, India.
Received for publication on 29 April 1993.
Accepted for publication in revised form on 7 December 1993.