- Volume 61 , Number 4
- Page: 550–5
Intrafamilial transmission of leprosy in Vellore town, India
ABSTRACT
A hospital-based study was done f rom 1968 to 1991 to determine the risk and extent of intrafamilial transmission of leprosy in relation to the characteristics of the index cases and contacts in urban areas in India. Families were examined by doctors annually. Skin smears were done for contacts of multibacillary (MB) leprosy patients. Person years of follow up were computed for each contact and used as the denominator for computation of incidence rates. Specific rates were computed by age, sex, type of leprosy, smear in index cases, age at registration, and sex of contacts. Of the 120 index cases (81 males, 39 females) 44% were MB; 410 contacts (186 males, 224 females) and 14 co-prevalent cases were registered. The cumulative years of follow up was 2725 years. Fourteen contacts developed the disease (9 TT, 3 indeterminate, and 2 BT); 85.7% were in the 0-14 age group; 12 of 14 patients were detected to have leprosy during the first 5 years. The incidence rate (IR) was 5.1/1000 (males 5.15, females 5.12). The IR was 7.3/1000 and 2.3/1000 among contacts of MB and paucibacillary leprosy patients (p < 0.05). The IR in multiple-case families was 1.8. The importance of active surveillance by a hospital-based survey is emphasized. It should be designed to focus on children younger than 15 years and should be limited to 5 years of follow up.RÉSUMÉ
Une étude réalisée à partir de l'hôpital a été réalisée de 1968 à 1991 pour déterminer le risque et l'extension de la transmission intra-familiale de la lèpre en relation avec les caractéristiques des cas index et des contacts dans des zones urbaines en Inde. Des familles ont été examinées chaque année par des médecins. Des frottis cutanés ont été prélevés chez les contacts de patients lépreux multibacillaires (MB). On a calculé le nombre de personnes-années d'observation pour chaque contact et on l'a utilisé comme dénominateur pour le calcul de taux d'incidence. On a calculé des taux spécifiques pour l'âge, le sexe, le type de lèpre et les frottis cutanés des cas index, l'âge à l'enregistrement et le sexe des contacts.Parmi les 120 cas index (81 hommes, 39 femmes), 44% étaient MB; 410 contacts (186 hommes, 224 femmes) et 14 cas co-prévalents on été enregistrés. Le total cumulé d'années de suivi était de 272 5 années. Quatorze contacts ont développé la maladie (9 TT, 3 indéterminés et 2 BT); 85.7 % appartenaient au groupe d'âges 0-1 4 ans; 12 des 14 contacts ont été détectés comme ayant la lèpre au cours des 5 premières années. Le taux d'incidence était de 5.1/1000 (hommes 5.15, femmes 5.12). Le taux d'incidence était de 7.3/1000 et 2.3/1000 respectivement parmi les contacts de patients lépreux MB et PB (p < 0.05). Le taux d'incidence dans les familles à cas multiples était de 1.8. L'importance de la surveillance active par enquêtes réalisées à partir de l'hôpital est soulignée. Celles-ci devraient être planifiées de manière à se concentrer sur les enfants de moins de 15 ans et devraient se limiter à un suivi de 5 ans.
RESUMEN
De 1986 a 1991 se realizó un estudio con control hospitalario para determinar el riesgo y el grado de transmisión intrafamiliar de la lepra en relación a las características de los casos índice y sus contactos, en áreas urbanas de la India. Las familias se examinaron anualmente por doctores calificados. En los contactos de los pacientes multibacilares (MB) se recurrió a la búsqueda de bacilos en extendidos de linfa cutánea. Para cada contacto se calcularon los años de seguimiento por persona y los resultados se usaron como denominador para el cálculo de los valores de incidencia. Los valores específicos se calcularon tomando en cuenta la edad, el sexo, el tipo de lepra, las baciloscopias en los casos índice, la edad al momento del registro, y el sexo de los contactos.De 120 cases índice (81 hombres, 39 mujeres), de los cuales 44% fueron MB, se registraron 410 contactos (186 hombres, 224 mujeres) y 14 casos coprevalentes. El tiempo acumulativo de seguimiento fue de 2725 años. Catorce contactos desarrollaron la enfermedad (9 TT, 3 indeterminados, y 2 BT); 85.7% estuvieron en el grupo de edades entre los 0 y los 14 años; 12 de los 14 contactos se diagnosticaron como enfermos de lepra en los primeros 5 años. El índice de incidencia fue de 5.1/1000 (hombres 5.15, mujeres 5.12). Los índices de incidencia fueron de 7.3/1000 en los contactos de los pacientes con lepra multibacilar, y de 2.3/ 1000 en los contactos de los pacientes con Iepre paucibacilar (p < 0.05). El índice de incidencia en las familias con múltiples casos fue de 1.8. Se enfatiza la importancia de la vigilancia activa coordinada por el centro hospitalario. Esta debe enfocarse a los niños menores de 15 años y estar limitada a 5 años de seguimiento.
Studies have been reported on the pattern of leprosy in urban areas (6,7,12) but none have been reported on the risk among contacts in such populations. Published data on the risks of intrafamilial transmission of leprosy are mostly from rural areas (3,5,9,10). Due to various demographic, environmental and social factors, both the extent of intrafamilial transmission as well as the underlying factors may be different in urban areas. Passive surveillance of urban areas has not been found to be successful by other workers (2). While cohort studies on leprosy patients and their families resident in an urban population might be done, they can be expensive, frustrating and subject to losses from observation. We have attempted a hospital-based study to determine the risk and extent of transmission within a family in relation to characteristics of both the index case and contacts. This paper presents the findings and also shows how a model for active surveillance of contacts could be integrated into the general health services of any hospital.
MATERIALS AND METHODS
Vellore town, the capital of North Arcot and Ambedkar Districts, covers an area of 15 sq. kms. and has a population of 172, 467. Christian Medical College Hospital is a major tertiary care center located in this town, and our study was done in the Dermatology and STD Clinic of this hospital. The clinic, for survey of contacts, is conducted once a week in the afternoon so as to reduce the inconvenience for those at work and school. Each family is examined annually by a doctor and services are rendered free. Notice of the date of examination is given by letter about 2 weeks in advance. An average of 4-5 families are examined every week and those families who default are visited at their homes by a social worker. Contacts who develop leprosy are registered as new cases and treated.
The study period extended from 1968 to 1991, and included all families currently under surveillance or released within the last 2 years. The index cases and their families included in the study resided in the urban area.
A proforma for each index case was filled with demographic data and details of the disease, such as the duration of disease prior to registration, past antileprosy treatment, number of persons living in the family or household defined as people living in close contact with each other under the same roof and partaking of food from the same kitchen. For each contact, details recorded were age at registration, sex, relationship to the index case, and details of clinical examination (such as the presence of patches, thickened nerves, and areas of sensory loss). A slit-skin smear for acid-fast basilli (AFB) from four sites was done at each yearly visit for each contact of index cases with multibacillary (MB) leprosy. The contacts who were detected to have leprosy at the same time of examination of the index cases were labeled as co-prevalent cases.
Patients were classified as indeterminate (Indet), tuberculoid (TT), borderline tuberculoid (BT), borderline borderline (BB), borderline lepromatous (BL), lepromatous (LL) and primary neuritic (N) on the basis of clinical features and the results of skin smears which were done for all patients in the borderline and lepromatous groups. During the earlier part of the study patients with borderline features were classified as dimorphous based on the Madrid classification (4).
Person years (PYR) of follow up were computed for each contact and used as the denominator for the computation of incidence rates. Specific rates were computed by sex, age, type of leprosy, and smear in index cases as well as by age and sex of contacts. Tests for proportion were done using z and x2 tests.
RESULTS
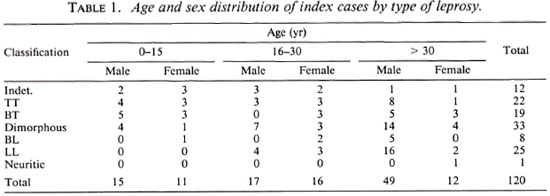
Profile of index cases. A total of 120 index cases (81 males, 39 females) were registered. The age, sex and type of leprosy are shown in Table 1; 50.8% of the cases were between 31 and 60 years and 21.6% were younger than 15 years of age; 50% of the patients were in the borderline group.
In 86% of the families the head of the household was literate; 10% of them had achieved a college-level education, 104 (86.6%) were nuclear families.
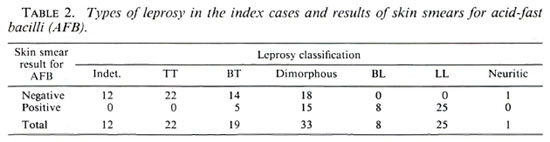
The classification by the different types of leprosy and the results of skin smears for AFB are given in Table 2. All patients in the lepromatous part of the spectrum were positive as were 15 of 33 with dimorphous and 5 of 19 with BT disease. Skin smears were negative in patients with Indet and TT leprosy. The duration of disease was reliably known in 111 of 120 cases, and 20% came to the hospital within 6 months of the onset of the disease. These included 4 Indet, 6 TT, 5 BT, 5 dimorphous, 3 LL, and 1 patient with primary neuritic leprosy; 86 of 120 (71.7%) of the patients denied having taken any prior treatment.
Profile of contacts. Five-hundred-two contacts were registered; 14 were found to have the disease during the first visit and were classified as co-prevalent cases. Of the remaining 488 contacts, 78 (15.9%) were examined only once during the first survey and were not included in the determination of PYR among the contacts. The total cumulative years of follow up in the remaining 410 contacts was 2725 years; 41(14 males, 27 females) of the contacts under surveillance defaulted after varying periods of follow up. Half of them were in the 0 to 14 age group; 27 of 41 (65.8%) defaulted after 5 years of follow up. Sixty-five percent of children in the 0 to 14 age group completed 5 years of follow up.
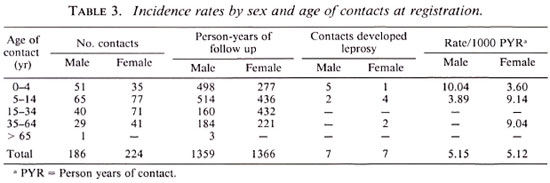
Incidence rates. Fourteen contacts developed leprosy, of whom 12 (85.7%) were in the 0 to 14 age group; the remaining 2 were in the 35 to 64 age group. The male : female (M:F) ratio was 1:1. The incidence rate (IR) per 1000 PYR was 5.1 and varied by age at registration and sex as shown in Table 3. There was no gender bias and the risk was highest in contacts younger than 15 years of age, being 6.9 in males and 7.01 in females.
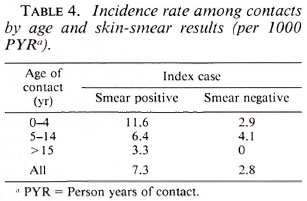
The IR was 7.3 per 1000 and 2.8 per 1000 among contacts of MB and paucibacillary (PB) cases, respectively; the difference was not statistically significant (Table 4).
The disease spectrum in contacts included 9 with TT, 3 Indet, and 2 BT leprosy; 12 of 14 (85.7%) were detected within the first 5 years of surveillance.
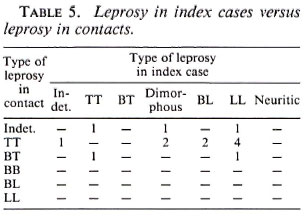
Leprosy in contacts by characteristics of the index cases. The characteristics of the 11 index cases whose contacts developed leprosy were analyzed. The M:F ratio of the 11 index cases was 4.5:1; the overall M:F ratio of the index cases was 2:1. None of the contacts of index cases less than 15 years old developed the disease; 7 of 11 (63.3%) of the source cases were between 31 and 60 years of age, the remaining were in the 16 to 30 age group. Table 5 shows the type of leprosy in the index cases and in the contacts who developed leprosy. The disease spectrum included 6 patients with LL, 2-each with TT and dimorphous, and 1 with Indeter leprosy; 8 of them were in the MB part of the spectrum. In three families there were 2 contacts who each developed leprosy. The source in all was LL. The duration of disease prior to registration was known in only 9 of 11 index cases; the average duration was 55.3 months. The relationships to the contacts were: parent in 7, spouse in 2, and grandparent in 2; husband and wife were infected in 2 families.
Leprosy in contacts of multiple-case families. Eleven multiple-case families were detected at registration (Table 6). Three families had two co-prevalent cases each; 10 of 14 (71.4%) of the co-prevalent cases were on treatment at the time of registration. In this group 25 persons had the disease (11 index cases and 14 co-prevalent cases), 7 were lepromatous and 18 nonlepromatous. Of the 43 contacts, 28 (65%) were in the 0 to 14 age group. The cumulative years of follow up in the contacts of multiple-case families was 528 years; only 1 contact developed the disease, the IR in this group being 1.8.
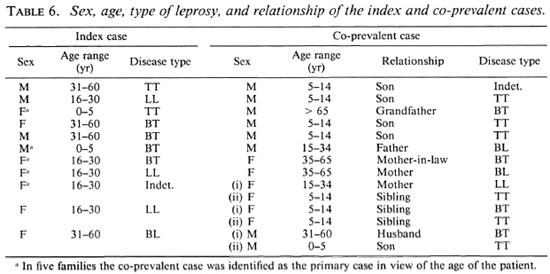
In five families the co-prevalent case was probably the index case taking into consideration the age of the person, the older person probably having acquired the disease earlier. The characteristics of these index cases and the contacts were analyzed to see if the pattern was similar to the rest of the source cases and their contacts. It was seen that although the ages of the source cases were similar to the single-case families where contacts developed the disease there were more females among the index cases. The disease spectrum was similar, 60% were lepromatous. Although the major age group at risk among contacts in the single-case families was children younger than 15 years, contacts aged 16 to 30 years were also found to be susceptible in this group. However, considering the long incubation period, these contacts may have been infected during childhood. Among the contacts who developed leprosy, one each had Indet and LL, and three were in the tuberculoid part of the spectrum.
DISCUSSION
The results from other studies done in urban areas (2,6,7,12) and our results have shown a higher prevalence of leprosy among adults. Although the study was done in an urban area and the majority of cases or the head of the household were literate only 20% of the index cases came to the hospital within 6 months of the onset of the disease. This emphasizes a large reservoir of untreated or inadequately treated persons with leprosy in the community. Data from this study show that there was no added risk to contacts living in multiple-case families, including those families where there were three members with leprosy. This is contrary to the observations of Jesudasan, et al. who found a statistically significant higher risk among multiple-case families of nonlepromatous index cases (5). Our data on the overall risk among household contacts, age group at risk, and the type of leprosy among the contacts compared favorably with results of other workers (5,9,10). It is noted that 12 of 14 (85.7%) contacts developed the disease within the first 5 years of follow up. A study done by Mathur, et al. also found that, irrespective of the type of disease in the index case, the maximum number of contacts developed disease with 5 years of contact (8). Results of our study suggest that the risk of infection is from within the family rather than from outside, even in a leprosy-endemic area, as suggested by Jesudasan, et al (5).
Although a greater number of contacts of MB leprosy developed the disease, the difference in incidence rates among contacts of MB and PB leprosy was not statistically different. It, however, points to the fact that PB leprosy is still a potential source of infection and cannot be ignored (1).
It is important to evolve a hospital-based surveillance program for contacts of leprosy patients since the early detection and treatment of contacts developing leprosy are important measures to reduce the reservoir of infection in the community. We have intcgrated the contact surveillance program into the existing hospital services since this will reduce stigmatization and social problems arising therein. The existing resources and services of the health care personnel have been utilized. Health education is given to increase the awareness of the disease and the importance of periodic surveillance of family members. Interest in the family encourages both compliance in patients and family members to come to the hospital. Data from our study and by other workers has shown a greater risk of acquiring the disease in children younger than 15 years of age (5,9). Further, because the majority developed the disease within 5 years of surveillance, a hospital-based survey should be designed to focus on contacts younger than 15 years of age for a period of 5 years. Compliance was also seen to be better the first 5 years in our study. This will help to reduce the load on the overburdened health care system in urban areas.
Revankar, et al. have shown that treatment of leprosy can be integrated successfully into the general health services in urban areas (11). However, the feasibility of hospital-based surveillance of contacts of persons with leprosy has not been studied. The present study recommends that contact surveillance should be integrated into the existing hospital services since treatment of the index cases alone would only partially address the problem of control of the transmission of leprosy.
Acknowledgment. We are grateful to Mr. David Selvapandian, B.Sc, for help in data entry and analysis and to Mrs. Linda Robert for secretarial assistance.
REFERENCES
1. BROWN, J. A. K. Factors influencing the transmission of leprosy. Trans. R. Soc. Trop. Med. Hyg. 53(1959)179-189.
2. GANAPATI, R., REVANKAR, C, PANDYA, S. S. and ACHAREKAR, M. Y. Prevalence of leprosy among inpatients in a general hospital-a survey in Bombay. Lepr. Rev. 51(1980)325-328.
3. GEORGE, K., JOHN, K. R., MULIYIL, J. P. and JOSEPH, A. The role of intra-household contact in the transmission of leprosy. Lepr. Rev. 61(1990)60-63.
4. INTERNATIONAL CONGRESS OF LEPROSY, MADRID 1953. Report ofCommittec on Classification. Int. J. Lepr. 21(1953)504-516.
5. JESUDASAN, K., BRADLEY, D., SMITH, P. G. and CHRISTIAN, M. Incidence rates of leprosy among household contacts of "primary cases" Lepr. India 56(1984)600-614.
6. KAUR, S., KUMAR, B. and ROY, S. M. Endemicity of leprosy in the union territory of Chandigarh and surrounding state. Lepr. India 54(1982)428-440.
7. MARSHALL, J. T., AMAR, D. S. and RAMESH, H. C. Prevalence of leprosy among slum dwellers, Lepr. India 53(1981)70-82.
8. MATHUR, N. K., SHARMA, M., BUMB, R. A. and YEGI, G. A study of multiple case families. Lepr. India 56(1974)200-206.
9. RAO, P. S. S., JESUDASAN, K., MANI, K. and CHRISTIAN M. Impact of MDT on incidence rates of leprosy among household contacts. Part 1. Baseline data. Int. J. Lepr. 57(1989)647-651.
10. RAO, P. S. S., KARAT, A. B. A., KALAIPERUMAL, V. G. and KARAT, S. Transmission of leprosy within households. Int. J. Lepr. 43(1975)45-54.
11. REVANKAR, C. R., JHA, S., DONGRI, V. V., DESHPANDE, S. and GANAPATI, R. Integration of leprosy into general health services in an urban area; a feasibility study. Lepr. Rev. 53(1982)297-305.
12. sehgel, V. N., Ghorpade, A. and SAHA, K. Urban leprosy-an appraisal from northern India. Lepr. Rev. 55(1984)159-166.
1. M.D.; Christian Medical College and Hospital, Vellore, South India 632004.
2. F.R.C.P.; Christian Medical College and Hospital, Vellore, South India 632004.
3. M.N. A.M.S., Department of Dermatology; Christian Medical College and Hospital, Vellore, South India 632004.
4. Dr. P.H., Department of Biostatistics, Christian Medical College and Hospital, Vellore, South India 632004.
Received for publication on 2 April 1993.
Accepted for publication on 28 June 1993.