- Volume 61 , Number 4
- Page: 592–6
Neuritis of the lateral femoral cutaneous nerve in leprosy
ABSTRACT
Neuritis of the lateral femoral cutaneous nerve (meralgia paresthetica) is observed more frequently in leprosy than in nonleprosy patients, and its symptoms can easily be confused with those suggesting, e.g., ischialgia. The diagnosis can be confirmed by a diagnostic block with a local anesthetic solution. Analgesics, antiinflammatory drugs, bed rest and, in severe cases, therapeutic blocks were successfully applied in the treatment of the neuritis, and no surgical intervention was needed. Three leprosy patients with severe meralgia paresthetica are presented.RÉSUMÉ
Une névrite du nerf fémoro-cutané latéral (méralgie paresthésique) est observée plus fréquemment chez des malades de la lèpre que chez des non-lépreux, et ses symptômes peuvent aisément être confondus avec ceux suggérant par exemple, l'ischialgic. Le diagnostic peut être confirmé par un blocage diagnostique avec une solution anesthésique locale. Des analgésiques, des médicaments anti-inflammatoires, du repos au lit et, dans les cas sévères, des blocages thérapeutiques ont été utilisés avec succès dans le traitement de la névrite, et aucune intervention chirurgicale n'était nécessaire. Trois patients présentant une sévère méralgie paresthésique sont présentés.RESUMEN
La neuritis del nervio cutáneo femoral lateral (meralgia parestesica) se observa con más frecuencia en los pacientes con lepra que en los pacientes sin lepra, y sus síntomas pueden confundirse fácilmente, por ejemplo, con aquellos de la isquialgia. El diagnóstico puede confirmarse por un diagnóstico de bloqueo con una solución de un anestésico local. Los analgésicos, las drogas antiinflamatorias, el reposo en cama y en los casos severos los bloqueos terapéuticos, fueron exitosamente aplicados en el tratamiento de la neuritis sin necesidad de recurrir a la intervención quirúrgica. Se presentan los casos de tres pacientes con meralgia parestésica severa.Leprosy is frequently complicated by localized neuritis of the peripheral parts of the ulnar, median, common peroneal, posterior tibial, facial and radial nerves, causing loss of sensation and/or motor function. Thickening of cutaneous nerves can frequently be found, mostly in the tuberculoid form of leprosy (2). Neuritis of the lateral femoral cutaneous nerve (LFCN) was first described by Hagcr (4) in 1885 and again by both Bernhardt (1) and Roth (7) in 1895. Roth gave it the name meralgia paresthetica. It is now generally accepted that meralgia paresthetica is a neuritis of the LFCN which is due to low-grade, continuous trauma at the site where the nerve leaves the pelvis (8).
In this paper we discuss the relationship between leprosy and the occurrence of meralgia paresthetica, an observation that we have not found in the literature. Three leprosy patients (the basis for this study) are presented as case reports.
MATERIALS AND METHODS
We compared a group of 205 leprosy patients seen at the clinic at Patan Hospital with a matched (age, sex, body weight, and height) control group of 50 nonleprosy patients seen at the general outpatient clinic of Anandaban Hospital.
In both groups the individuals were examined for: a) enlargement of the LFCNs; b) past and present complaints of a tingling, painful sensation over the lateral and anterolateral aspect of the thigh, and c) sensation over the area when measured with a Scmmes-Weinstein nylon monofilament with a bending force of 5 g. Examinations were done with the patient in a supine position by an experienced physiotherapist and a physio-assistant.
The significance of the differences in enlargement, as well as the history and present complaints, were tested with the chi-squared test.
RESULTS
Of the 205 leprosy patients 90 (44%) had loss of sensation as measured with a 5-g nylon monofilament only on the anterolateral side of the thigh; in 37 patients loss of sensation also was found elsewhere in the thigh. None of the control group had loss of sensation in this area when measured in the same way.
In the period prior to this survey we saw six severe cases of meralgia paresthetica in leprosy patients at Anandaban Leprosy Referral Hospital in Nepal. Of these, three are presented as case reports.
Case 1. Mr. B. B. S. (45 years of age) presented at our outpatient clinic and was diagnosed as having borderline lepromatous leprosy. His skin smear was: BI = 4 + , MI = 0, lepromin test = negative.
Treatment was started with multidrug therapy for multibacillary patients (M.MDT) according to the regimen recommended by the World Health Organization (WHO) in 1981. Three weeks later he returned to our clinic 1 week earlier than planned with complaints of pain in multiple nerves in his left thigh and in his swollen facial patches. These were diagnosed as originating from a type 1 or reversal reaction. Treatment With prednisone 20 mg b.i.d. was started.
One week later he complained again of severe pain at the anterolateral side of his left thigh. In the same area no sensation was detected when touched with a nylon monofilament bending at 5-g pressure. On his left side just mediocaudal to his anterosuperior iliac spine he had a greatly enlarged LFCN (Fig. 1). At this site there was a positive Tincl's sign for the above-mentioned pain. There was no sign of infection in the left leg. A cytologic needle aspiration of the nerve showed multiple acid-fast bacilli (AFB). The diagnosis was made ofmcralgia paresthetica in the left thigh as part of the type 1 reaction. This diagnosis was further supported by immediate and complete relief of the pain after blocking the LFCN with 10 cc bupivacaine 1.5% solution with epinephrine to which was added 8 mg dexamethasone acetate. This block was repeated twice after which the LFCN only remained tender on palpation.
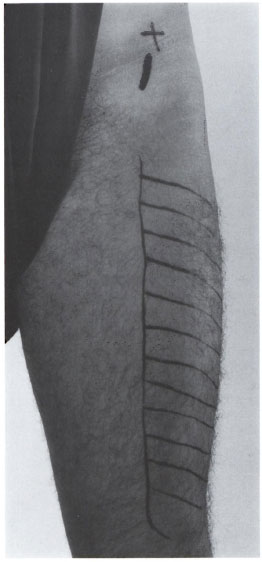
Fig. 1. Case 1. Enlarged lateral femoral cutaneous nerve (LFCN) and loss of sensation at the anterolateral side of left thigh; + = anterosuperior iliac spine.
Case 2. In consultation we saw Mr. B. B. (52 years of age) who had been on the M.MDT-WHO regimen for 14 months because of BT-BB type of leprosy. He complained of severe pain in both of his thighs for 6 months. This was earlier labeled as ischialgia due to a herniated intervertebral disc. At examination we saw that the patient could walk only while bending forward. Both of his LFCNs were grossly enlarged. On palpation a tingling sensation at the anterolateral aspects of both thighs was experienced. There were no other signs of nerves in reaction. His skin smear BI = 2 + , MI = 8%.
A cytological needle aspiration of the affected nerves showed multiple AFB in both nerves. The diagnosis ofmcralgia paresthetica due to leprosy neuritis was supported by bilateral diagnostic blocks each with 15 ml lidocaine 0.5% to which was added 8 mg dexamethasone acetate. Subsequent to administration of the LFCN blocks the patient could walk in an erect position since there was complete relief from the pain. A local physician later repeated the blocks twice and reported that the patient had responded well and had remained free of pain thereafter.
Case 3. Mrs. P. L. (40 years of age from the Lhasa region in Tibet) presented at our Patan clinic with severe osteomyelitis of the left calcaneus with fracture of the corpus. The diagnosis of BL leprosy was made and the M.MDT-WHO regimen was started. Her BI = 3 + , MI = 0, lepromin test = negative. During the subsequent hospital admission the osteomyelitis was successfully treated by septic surgery.
During a readmission for a finger infection 1 year later, the patient developed excruciating pain in her left lower extremity with moderate enlargement of the LFCN which was very tender on palpation. There were no signs of a leprosy reaction and no recurrence of infection of the left foot. Cytological needle aspiration of the LFCN showed AFB in clusters.
The diagnosis of meralgia paresthetica was supported by immediate and complete relief of the pain after blocking the LFCN with 10 cc bupivacaine 1.5% solution with epinephrine to which was added 8 mg dexamethasone acetate. We prescribed bed rest and another two blocks with bupivacaine without dexamethasone were given over the next month. There has been no recurrence of her complaints.
DISCUSSION
We found a significant difference in the occurrence of involvement of the lateral femoral cutaneous nerve (LFCN) in leprosy patients compared to the control group. There was a higher proportion of nerve enlargement, history of complaints (p < 0.001) and of present complaints (p < 0.05) in the patient group compared to the controls. Isolated loss of sensation at the anterolateral side of the thigh was found in 44% of the leprosy patients but in none of the controls. The proportion might have been even higher if lighter filaments had been used in testing for sensation. Sometimes the complaints can be severe, as illustrated in our case reports.
Causative factors. The constituent fibers of the LFCN are derived from varying combinations of the first-to-third lumbar nerves. The nerve emerges from the lateral side of the psoas muscle and passes under the lateral end of the inguinal ligament at the site of its attachment to the anterosuperior iliac spine and becomes cutaneous in the lateral thigh (Fig. 2). Here the nerve is wedged in the angle between the bone, the ligament, and the sartorius muscle. Hereafter it enters the thigh beneath the fascia lata and provides sensation to the lateral and anterolateral aspect of the thigh.
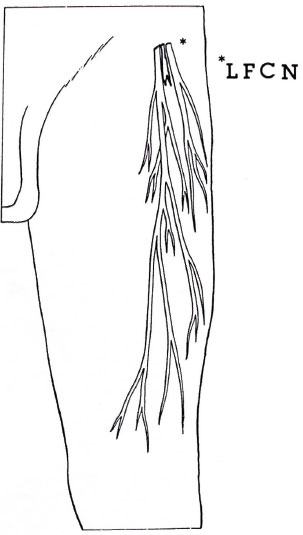
Fig. 2. The lateral femoral cutaneous nerve (LFCN).
It is generally accepted that meralgia paresthetica is due to low-grade continuous trauma at the site where the nerve leaves the pelvis. In leprosy, localized swelling of the LFCN may contribute to the mechanical trauma. In this area the nerve runs at a cool superficial site which in leprosy seems to predispose to leprosy neuritis (2).
In the nonleprosy literature several anatomical arrangements have been described (3) at the site where the nerve enters the thigh which increase the risk of damage when, for any reason, the nerve is stretched.
Diagnosis. In neuritis of the LFCN the patient may complain of a tingling, dull aching, burning sensation or numbness over the lateral and anterolateral aspect of the thigh. The pain can be aggravated when the limb is extended at the hip and when the patient stands or walks for any length of time. In order to flex the hip and relieve stretch on the nerve, the patient may limp or walk while bending forward. The pain is sometimes severe and incapacitating.
At physical examination one may find: a) localized tenderness and swelling of the LFCN; on palpation the nerve may be tender just below and medial to the anterosuperior iliac spine; in varying degrees the LFCN can be swollen, b) loss of sensation; there may be loss of sensation in the skin area supplied by the LFCN in varying degrees although, of course, other mechanisms also can be responsible for this, especially in leprosy, c) nerve conduction studies; the finding of slowing or absence of LFCN conduction may be helpful, especially when a difference between the LFCN conduction of the affected and contralateral side can be found. But these studies are difficult, often not conclusive (9), and in general not available in developing countries, d) diagnostic block with local anesthetic solution; under field conditions a simple diagnostic block as described by Moore (6) can support the diagnosis.
In leprosy the complaints are often, but not always, associated with a reactional state.
Therapy. In a case with severe pain suspected to be due to neuritis of the LFCN, we inject together with our diagnostic block a single dose of 40 mg methylprednisolone (Depo-Medrol®). If the diagnosis is confirmed by a total disappearance of the complaints, we prescribe bed rest, oral analgesic and antiinflammatory drugs, depending on the severity of the complaints and the extent of leprosy neuritis elsewhere in the body. In a case of very severe, localized neuritis we repeat the blocks with only a local anesthetic solution on alternating days.
When meralgia paresthetica forms a part of a severe leprosy reaction oral corticosteroids also are given; we give oral prednisone in a basic adult dose of 60 mg daily for 2 weeks after which the daily dose is tapered, depending on the clinical situation.
Although various surgical interventions have been described (5,10) in severe, disabling meralgia paresthetica, surgery has not been necessary in our patients suffering from meralgia paresthetica since, so far, all of them have reacted favorably to the therapy we have described.
REFERENCES
1. BERNHARDT, M. Ueber isolirt im Gcbicte des N. Cutaneous Femoris Externus vorkommende Paresthesian. Neurol. Zentbl. 14(1895)242-243.
2. BRAND, P. W. and FRITSCHI, E. P. Rehabilitation in leprosy. In: Leprosy. Hastings, R. C, ed. Edinburgh: Churchill Livingstone, 1985, p. 209.
3. CHUSID, J. G. Spinal nerves. In: Correlative Neuroanatomy and Functional Neurology. New Delhi: Lange, 1976, p. 124.
4. HAGER, W. Neuralgia Femoris. Dt. Med. Wschr. 11(1885)218-219.
5. KEEGAN, J. J.and HOLYOKE, E. A. Meralgia paresthetica, an anatomical and surgical study. J. Neurosurg. 19(1964)341-345.
6. MOORE, D. C. Block of the lateral femoral cutaneous nerve. In: Regional Block. 4th edn. Springfield, IL: Charles C. Thomas, 1978, pp. 294-299.
7. Rani, W. K. Meralgia paresthetica. Med. Ohozr.Mosk. 43(1895)678-679.
8. SUNDERLAND, S. Lateral femoral cutaneous nerve, meralgia paraesthetica. In: Nervos and Nervo Injure. 2nd edn. New York: Churchill Livingstone, 1978, pp. 1007-1010.
9. TAYLOR, R. G. and LIEBERMAN, J. S. Electrodiagnosis in lower extremity nerve compression. In: Nerve Compression Syndromes. Szabo, R. M., ed. Thorofare, NJ: Slack, Inc., 1989, pp. 89-90.
10. TENG, P. Meralgia paresthetica. Bull. Los Angeles Neurol. Soc. 37(1972)75-83.
1. M.D., Medical Superintendent and Plastic and Reconstructive Surgeon; Anandaban Hospital, Kathmandu, Nepal.
2. P.T., Head, Department of Physiotherapy; Anandaban Hospital, Kathmandu, Nepal.
3. M.Sc, Ph.D., Head, Mycobacterium Research Laboratory; Anandaban Hospital, Kathmandu, Nepal.
4. M.B.B.S., Surgeon, Anandaban Hospital, Kathmandu, Nepal.
5. M.D., Ph.D., Head, Department of Anatomy, St. Radboud University Hospital, Nijmegen, The Netherlands.
Reprint requests to Dr. W. J. Theuvenet, Plastic and Reconstructive Surgeon, Lukas Hospital, P.O. Box 9014, 7300 DS Apeldoorn, The Netherlands.
Received lor publication on II June 1993.
Accepted for publication in revised form on 19 August 1993.