- Volume 61 , Number 4
- Page: 597–9
Cytological needle aspiration of the nerve for the diagnosis of pure neural leprosy
ABSTRACT
Pure neural (also called primary neuritic) leprosy manifests itself by involvement of only the nerve in the absence of skin lesions. Therefore, it sometimes can pose a diagnostic problem. Cytological needle aspiration of an affected nerve can be a valuable tool under such circumstances. The method as developed at Anandaban Leprosy Hospital, Nepal, is described and two cases are presented.RÉSUMÉ
La lèpre purement néviritique (également appelée névritique primaire) se manifeste par le seul envahissement de nerfs en l'absence de lésions cutanées. Cela peut donc parfois poser un problème pour le diagnostic. Une aspiration cytologique par aiguille d'un nerf affectée peut être un instrument valide dans de telles circonstances. La métode est décrite telle qu'elle a été développée à l'Hôpital pour la Lèpre d'Anadaban au Népal, et deux cas sont présentés.RESUMEN
La lepra neural pura (también llamada lepra neurítica primaria) se manifiesta por la sola afección de nervios sin la presencia de lesiones en piel, ésto a menudo causa problemas en el diagnóstico de la enfermedad, liajo tales circunstancias, la aspiración citológica de un nervio afectado puede ser de gran utilidad en el diagnóstico. En este trabajo se describe el método desarrollado en el Hospital Anandaban de Nepal, en relación dos casos de lepra neurítica primaria.Due to the scarcity of the cardinal signs of leprosy, pure neural leprosy can be difficult to diagnose. This is because there are no anesthetic skin lesions, only in some cases is there nerve enlargement and, in general, no acid-fast bacilli (AFB) can be demonstrated in the skin or nasal mucosa. The neuritis may express itself in sensory and/ or motor function loss resembling other peripheral nerve diseases, such as M. Charcot-Marie-Tooth, etc.
The skill and facilities for additional examinations, such as histopathology of nerve biopsies, immunological assessments, etc., are usually not available where needed for the diagnosis of most leprosy cases, i.e., in the field. Cytological needle aspiration of an afTected nerve can be a valuable tool under such circumstances. The method developed at Anandaban Leprosy Hospital, Nepal, is described here and two cases are presented.
MATERIALS AND METHODS
In the past 6 months we have performed cytological needle aspirations of enlarged nerves in 11 patients suspected of having pure neural leprosy. Before aspiration the patient was thoroughly screened for changes in motor function and light touch sensation with Semmes-Weinstein nylon monofilaments (GWL Hansen's Disease Center, Carville, Louisiana, U.S.A), and this was repeated both the day and the week after the procedure. The cytological needle aspiration was performed as follows:
We prepared the skin with alcohol and put a nerve block with 5 ml lidocaine 0.5% proximal to the site of the intended cytological needle aspiration. A new disposable needle (18G) and syringe was filled with 0.5 ml physiological saline to be used as a carrier. The nerve to be aspirated was fixed between the thumb and index fingers of one hand while with the other hand the needle was inserted into the nerve as parallel to its fascicles as possible. After positioning the tip of the needle, the body of the syringe was steadied between the thumb and index finger while with the ring and little finger the plunger was pulled outwardly, thus creating a negative pressure inside the syringe and needle (The Figure). While maintaining the negative pressure and with the other hand fixing the nerve, the needle was moved to and fro inside the nerve three times over a distance of about 2 cm. In this way cells from inside the nerve were aspirated into the needle. Then the plunger was carefully and slowly released. An abrupt release would briefly create a positive pressure inside the syringe with the consequent loss of aspirated material. The needle was withdrawn, then it was disconnected, the plunger was pulled back, and the needle was remounted. With the tip of the needle above a glass slide, the plunger was pressed, and thus the aspirated fluid inside the needle together with the saline (3) was discharged onto the slide. The material was stained by the Ziehl-Neelsen method for AFB at the Mycobacterium Research Laboratory of our hospital.
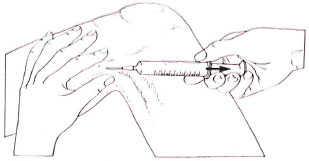
The Figure. Cytological needle aspiration of the left lateral popliteal (common peroneal) nerve.
RESULTS
Multiple AFB were found in the aspirated nerve fluid of 7 out of the 11 examined patients. Two of the seven patients are presented here as case reports.
Case 1. Mr. K. B. A. (Hosp. no. 10362, 26 years of age) was seen on 2 January 1991, referred by another hospital with the possible diagnosis of leprosy because of a 2-month old ulcer of the left foot and footdrop on the same side of 1-year duration. There was a history of a cut injury on the mediodorsal side of the left foot 1 year before. He had been treated with 3 months of multidrug therapy (rifampin 600 nig once monthly, clofazimine 300 mg once monthly, clofazimine 50 mg once daily and dapsone 100 mg once daily).
On physical examination no skin patches were seen. On the left foot total anesthesia was found on the plantar side with complete loss of dorsiflexion (0 on the VMT scale*) and almost complete loss of eversión (1 on the VMT scale) of the ankle joint, this of 1-year duration according to the patient. At the mediodorsal side of the foot a scar was visible 3 cm in length over the tendons of the anterior tibial muscle and the long extensor of the big toe. There was minor enlargement of the left common peroneal (lateral popliteal) and sural nerves with doubtful enlargement of the left ulnar and posterior tibial nerves.
On the suspicion of pure neural leprosy, a cytological needle aspiration was done which revealed AFB 1 +. This added one of the cardinal signs of leprosy and confirmed the diagnosis. With conservative treatment the foot ulcer healed well, and the patient was discharged with a PVC footdrop inlay splint. He is scheduled for surgical treatment of the footdrop within 1 year.
Case 2. Mr. D. B. T. (Hosp. no. 10384, 40 years of age) presented at our clinic because of a tingling sensation in his left hand and foot of 2 months' duration. No diagnosis had been made, and he had taken no medical treatment.
On physical examination a tender, elastic, round, subcutaneous swelling about 8-10 mm in diameter was found at the mid-dorsal aspect of his left lower arm. There were no skin patches and no abnormalities were found with regard to sensation (when measured with 5-g nylon monofilaments) or muscle strength (on the 0 to 5 VMT scale). Slit-skin smears for AFB at five routine sites were negative, his lepromin skin test was negative, and antiphenolic glycolipid-I antibodies were negative.
Since pure neural leprosy was suspected, we performed a cytological needle aspiration of the swelling on the left lower arm which revealed a bacterial index (BI) of 3 + . This confirmed the diagnosis, and multidrug therapy was started with rifampin 600 mg once monthly, clofazimine 300 mg once monthly, clofazimine 50 mg once daily, and dapsone 100 mg once daily.
Because of a persistent local tenderness we explored the tumor and took a biopsy of what appeared to be a tumor of the posterior branch of the antebrachial cutaneous nerve. A histopathological examination (S. Lucas) showed: "a multibacillary leproma (undoubted leprosy) of the borderline leprosy type with a BI of 4.5 + . It could very well be a leprosy colonization of an old traumatic neuroma."
DISCUSSION
There seem to be variations in the epidemiology of pure neural leprosy. In Nepal about 7% of all our patients present with this form of leprosy, but in other areas this amounted to one sixth of all patients (3).
Pure neural leprosy in general will fall from typical tuberculoid to borderline lepromatous leprosy in the Ridley-Jopling classification. A few cases of the lepromatous form of pure neural leprosy have been reported (2). Appropriate typing of pure neural leprosy requires additional study of the immunological, bacteriological and histopathological features (1). Presently available immunological tests have their limitations as diagnostic tools, while for bacteriological and histopathological tests one needs a nerve biopsy specimen.
Skin biopsies from anesthetic areas may fail to show histological changes suggestive of leprosy. When the symptoms of nerve involvement are scarce and where laboratory facilities for the above-mentioned examinations are not available, the diagnosis of pure neural leprosy can offer a challenge to the clinician.
In an attempt to acquire a tool less invasive than a nerve biopsy and still suitable under field conditions, we performed a number of cytological needle aspirations of nerves of patients suspected of having pure neural leprosy. In 7 of the 11 patients in whom cytological aspiration of the affected nerve was done multiple AFB were found, thus strongly supporting the diagnosis of pure neural leprosy.
In none of the patients who underwent cytological aspiration of the nerve was a subsequent iatrogenic loss of motor function or sensation found the next day or 1 week after. Besides minor discomfort on palpation of the nerve at the aspirated site in three patients on the first postoperative day, no local changes could be detected. Since most field programs have limited facilities yet, in general, are capable of doing Zichl-Neelsen staining, a cytological aspiration of the nerve can be a valuable tool in supporting the diagnosis of pure neural leprosy.
In advance research programs aspirated nerve fluid could provide valuable information on the pathoimmunology and serology of, for example, reversal reaction mechanisms inside the nerve. At Anandaban Hospital the multidrug therapy for smear-positive patients is continued for at least 2 years and only discontinued when the slit-skin smear has become negative, conforming to the recommendations of the World Health Organization (4). Therefore, we recommend repeating the cytological aspiration of the nerve for AFB at the same site after completing 24 doses of multidrug therapy in order to determine if additional treatment is needed for pure neural leprosy cases.
Acknowledgment. We arc indebted to Mr. Ross Morgan, graphic designer at our hospital, for helping us with the preparation of the illustration. We are grateful for the assistance of Dr. Sebastian Lucas, Pathologist, Middlesex Hospital, London, U.K.
REFERENCES
1. DHARMENDRA. Classification of leprosy. In: Leprosy. Hastings, R. C, cd. Edinburgh: Churchill Livingstone, 1985, p. 97.
2. JACOB, M. and MATHAI, R. Diagnostic efficacy of cutaneous nerve biopsy in primary' neuritic leprosy. Int. J. Lepr. 56(1988)56-60.
3. NOORDEEN, S. K. Epidemiology of polyneuritic type or leprosy. Lepr. India 44(1972)90-96.
4. WHO STUDY GROUP. Chemotherapy ofleprosy for control programs. Geneva: World Health Organization, 1982. Tech. Rep. Ser. 675.
1. M.D., Plastic and Reconstructive Surgeon and Medical Superintendent; Anandaban Hospital, The Leprosy Mission International, P.O. Box 151, Kathmandu, Nepal.
2. R.N., Assistant Nursing Superintendent; Anandaban Hospital, The Leprosy Mission International, P.O. Box 151, Kathmandu, Nepal.
3. B.Sc, Head, Mycobacterium Research Laboratory; Anandaban Hospital, The Leprosy Mission International, P.O. Box 151, Kathmandu, Nepal.
4. P.M.W., Laboratory Technician, Anandaban Hospital, The Leprosy Mission International, P.O. Box 151, Kathmandu, Nepal.
Reprint requests to Dr. Theuvenet, Plastic, Reconstructive and Hand Surgeon, Lukas Hospital, P.O. Box 9014, 7300 DS Apeldoorn, The Netherlands.
Received for publication on 8 June 1992.
Accepted for publication in revised form on 19 August 1993.
* Muscle strength is measured by voluntary muscle testing (VMT) on a 0-5 scale according to the method recommended by the Medical Research Council (MRC memorandum no. 45, HM50, 1982).