- Volume 61 , Number 4
- Page: 581–5
Lack of expression of Intercellular adhesion molecule ICAM-1 in lepromatous leprosy patients
ABSTRACT
It is conceivable that an abnormal expression of cell-adhesion molecules can contribute to the poor inflammatory response seen in some inflammatory skin diseases. Adhesins are cell-surface molecules that are expressed by many cell types. The main function of adhesins appears to be the promotion of cellular interactions, such as those occurring between immune cells. The epidermis of patients with inflammatory skin diseases exhibits an increased expression of ICAM-1, and it has been postulated that such increased expression can be important in the genesis of cutaneous inflammation. The expression of cell-adhesion molecules (LFA-1, LFA-2, LFA-3 and ICAM-1) in skin lesions of leprosy patients was studied, as well as the in vitro expression of these molecules induced with gamma interferon (IFN-γ). A lack of expression of ICAM-1 in the epidermis of lepromatous patients was noted; in addition, no expression of ICAM-1 was seen in the nearly normal skin f rom these patients incubated with IFN-γ. A similar expression of the four molecules studied was noted in the dermis of both the lepromatous and tuberculoid types of leprosy. The epidermis of the lepromatous leprosy patients appears to have a defective expression of ICAM-1.RÉSUMÉ
Il est concevable qu'une expression anormale des molécules permettant l'adhésion cellulaire puisse contribuer à la pauvre réponse inflammatoire observée dans certaines maladies cutanées inflammatoires. Les adhésines sont des molécules de surface cellulaire qui sont exprimées par beaucoup de types cellulaires. La fonction principale des adhésincs semble être la promotion des interactions cellulaires, telles que celles survenant entre des cellules immunitaires. L'épiderme des patients présentant des maladies cutanées inflammatoires montre une augmentation de l'expression d'ICAM-1, et il a été postulé qu'une telle augmentation de l'expression peut être importante dans la genèse de l'inflammation cutanée. On a étudié l'expression des molécules d'adhésion cellulaire (LFA-1, LFA-2, LFA-3 et ICAM-1) dans les lésions cutanées de malades de la lèpre, ainsi que l'expression de ces molécules in vitro, induite par l'interferon-gamma (IFN-γ). On a noté un manque d'expression d'ICAM-1 dans l'épiderme de patients lépromateux; de plus, aucune expression d'ICAM-1 n'a été observée dans la peau normale de ces patients incubée en présence d'IFN-γ. On a noté dans le derme une expression similaire des 4 molécules étudiées pour la lèpre lépromateusc et la lèpre tuberculide. L'épidcrme des patients lépromateux semble avoir une expression déficiente d'ICAM-1.RESUMEN
Es posible que una expresión anormal de las moléculas de adhesión celular pueda contribuir a la pobre respuesta inflamatoria observada en algunas enfermedades inflamatorias de la piel. Las adhesinas son moléculas de superficie expresadas por muchos tipos de células. La principal función de las adhesinas parece ser la promoción de las interacciones celulares tales como aquellas que ocurren entre las células inmunitarias. La epidermis de los pacientes con enfermedades inflamatorias de la piel exhiben una expresión incrementada de ICAM-1, y se ha propuesto que tal expresión incrementada pueda ser importante en la génesis de la inflamación cutánea. En este trabajo se estudió la expresión de las moléculas de adhesión celular (LFA1, LFA-2, LFA-3, e ICAM-1) en las lesiones dérmicas de los pacientes con lepra, así como el efecto del interferon gamma (IFN-γ) en la expresión in vitro de estas moléculas. Se notó una falta de expresión de ICAM-1 en la epidermis de los pacientes lepromatosos así como una falta de expresión de ICAM-1 en la porción de piel normal de estos pacientes cuando ésta se incubó con IFN-γ. Sin embargo, la expresión de las cuatro moléculas de adhesión estudiadas fue similar en la dermis de los pacientes lepromatosos y tuberculoides. La epidermis de los pacientes con lepra lepromatosa parece tener un defecto en la expresión de ICAM-1.Leprosy patients, particularly lepromatous leprosy patients, are unable to react either in vivo or in vitro against Mycobacterium leprae antigens; this phenomenon is antigen specific. The cause of this specific immune anergy remains unknown. Specific T-suppressor cells and a poor production of cytokines (such as interleukin-2 and gamma interferon) have been postulated as possible causes of such anergy (5,11,13). Usually immune inflammatory skin diseases are mediated by the selective influx and localization of T lymphocytes. Receptor-ligand interactions between skin cells and T lymphocytes play an important role in the tissue migration of T lymphocytes, a phenomenon that involves cytokine production and adhesion molecule expression by lymphocytes and skin cells; these molecules are called adhesins (10). The main functions of adhesins appear to be the promotion of cellular interactions, such as those occurring between immune cells, and the regulation of the cell-extracellular matrix interactions (3,6,9). Adhesins expressed by lymphocytes [LFA-1 (lymphocyte function-associated antigen-1), LFA-2] have specific ligands [ICAM-1 (intercellular adhesion molecule1), LFA-3] that are found in other immune and nonimmune cells (7,8,16). Recently, keratinocyte ICAM-1 expression has been found in inflammatory dermatoses that have in common lymphocyte apposition under the epidermis (10,17-19). In vitro studies have shown that T cells bind to keratinocytes after the epithelial cells are stimulated with gamma interferon (IFN-γ) and/or tumor necrosis factor alpha (TNF-α) (1,2,7,14,16). It is conceivable that an abnormal expression of cell-adhesion molecules, mainly ICAM-1, may contribute to the poor inflammatory response seen in the skin of lepromatous leprosy patients in response to M. leprae. We have studied the expression of intercellular adhesion molecules in skin lesions of leprosy patients, as well as the in vitro expression of these molecules after attempts at induction with IFN-γ in the apparently normal skin of leprosy patients.
MATERIALS AND METHODS
Patients. Eleven lepromatous and eight tuberculoid patients, who were on antimicrobial therapy (dapsone 100 mg daily plus clofazimine 50 mg daily plus rifampin 600 mg once monthly, and dapsone 100 mg daily plus rifampin 600 mg once monthly, respectively) were studied. Patients receiving thalidomide or cortisone were excluded, as were patients with lepra reaction. At the time of biopsy, the patients were inactive bacteriologically. Skin biopsies were taken from lesional and apparently normal skin of each patient. Positive control biopsies for ICAM-1 were taken from lesions of patients with psoriasis and lichen planus.
Detection of cell adhesion molecules. Four-Atm cryostat sections were obtained from frozen specimens, stored in liquid nitrogen, and mounted on glass slides. The slides subsequently were fixed in acetone for 10 min and rehydrated in phosphate-buffered saline (PBS) for 10 min. Then they were incubated with normal horse serum in PBS for 20 min, after which they were incubated for 60 min in a humidified chamber at 37ºC with the following primary mouse monoclonal antibodies: LFA-1 (CD 11a), LFA-2 (CD2), LFA-3 (CD58) (Dakopatts, Glostrup, Denmark) and ICAM-1 (CD54; kindly provided by Dr. T. Lowley and Dr. E. Garcia, Emory University, Atlanta, Georgia, U.S.A.). After the skin sections were washed with PBS, they were incubated for 30 min with the biotinylated secondary antibody at 37ºC. Then they were treated with the avidin-biotin peroxidase system (Vectostain; Vector Laboratories, Inc., Burlingame, California, U.S.A.) for 30 min, followed by incubation for 5 min in 3-amino-ethyl-carbazole, washed with distilled water, and counterstained with Mayer-hematoxylin.
Induction of cell adhesion molecule expression. Specimens of apparently normal skin from leprosy patients were incubated for 48 hr at 37ºC in 100% humidity and 5% CO, in RPMI-1640 medium (GIBCO Laboratories, Grand Island, New York, U.S.A.) supplemented with 5% fetal calf serum (Sigma Chemical Co., St. Louis, Missouri, U.S.A.), with penicillin (100 U/ml) and streptomycin (100 µg/ml) (GIBCO) in the presence of purified recombinant human IFN-γ (5000 U/ml; kindly provided by Dr. J. Calderón, Centro de Investigación y Estudios Avanzados, Mexico). A portion of the same biopsy was incubated under similar conditions but without the addition of IFN-γ.
Analysis. All skin sections were evaluated blindly by three separate investigators. The results were expressed as a "positive" or "negative" for each monoclonal antibody; positivity was further classified as moderate or strong.
RESULTS
In all of the patients with tuberculoid and lepromatous leprosy characteristic histologic features were found. In control biopsies, ICAM-1 expression was present in the epidermis and in the endothelial cells of the dermis.
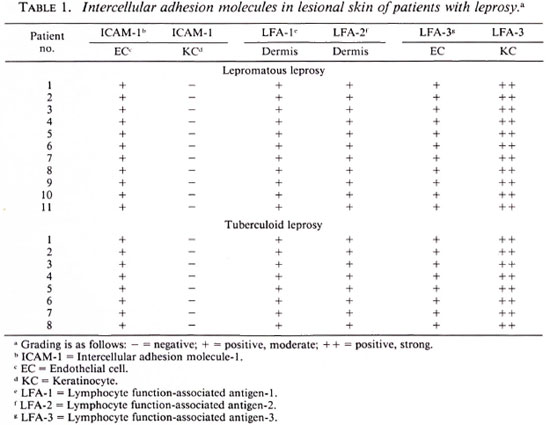
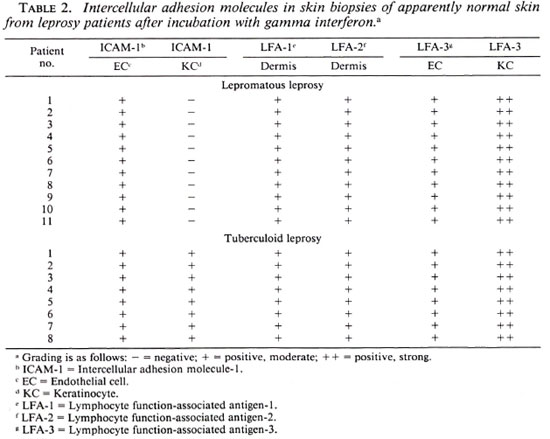
A lack of ICAM-1 expression was found in the epidermis of skin lesions from patients with lepromatous leprosy but ICAM-1 expression was observed in skin lesions from the patients with tuberculoid leprosy. The dermal expression of the other adhesion molecules studied was similar in both tuberculoid and lepromatous leprosy patients. LFA-3 was detected in the epidermis and dermis of both types of patients (Table 1). IFN-γ induced practically no epidermal ICAM-1 expression in the biopsies of the apparently normal skin of lepromatous leprosy patients. In apparently normal skin biopsies of tuberculoid leprosy patients, IFN-γ induced a higher ICAM-1 expression than in the lepromatous leprosy patients, but less than that induced in healthy subjects (Table 2).
DISCUSSION
Leprosy is a chronic infectious disease caused by Mycobacterium leprae. The occurrence or nonoccurrence of the disease is closely interlinked with the absence of an appropriate cell-mediated immune response to M. leprae. The cause of specific immune anergy in lepromatous leprosy patients remains undetermined. Since in other inflammatory diseases the intercellular adhesion molecules play an important role in the initiation of inflammatory response, it is possible that their abnormal expression may contribute to the antigen-specific, poor inflammatory response seen in the lepromatous type of leprosy. This working hypothesis appears to have some support when we consider the results obtained in the present work, since skin lesions of lepromatous leprosy patients in this series did not express ICAM-1 in the epidermis. This fact may impair the ability of these patients to fight the infectious agent, and in that way, a more widespread disease is permitted. Recently, Modlin, et al. (17) showed similar data regarding the tissue expression of adhesion molecules in leprosy. However, we also found that lepromatous leprosy patients are unable to express ICAM-1 in their apparently normal keratinocytes after appropriate incubation with IFN-γ.
As has already been pointed out, T lymphocytes from leprosy patients are unable to produce the molecular signals to carry out a normal cellular-immune response toward M. leprae, particularly IL-2 and IFN-γ. This lack of IFN-γ production, due perhaps to T-cell deletion or excessive down-regulation, could be part of the pathogenesis of this disease. Nevertheless, the finding of no response of apparently normal keratinocytes to IFN-γ stimulation in lepromatous leprosy patients shifts the attention of the source of the immune defect in leprosy from T cells to keratinocytes, cells with macrophage-like functions. It is possible that these cells may play a more important role in this disease than has been thought previously. It may be stated that, among several possibilities, the dermal-epidermal interaction in leprosy is anomalous due to defects in epidermal ICAM-1 expression; it is likely that this abnormality may be connected to the development of the disease in the fashion that we encounter in the clinical setting. Another possibility is that the atrophic lepromatous leprosy skin cannot express ICAM-1. However, several lepromatous skin biopsies showed a minimal degree of atrophy and, even in these cases, no expression of ICAM-1 was found. Furthermore, the atrophic skin of the elderly is capable of expressing ICAM-1 after IFN-γ induction (4).
With the aim of unravelling the immune defect of the host toward M. leprae, it might be helpful to study the expression of other adhesion molecules, such as VCAM-1 or P and E-selectins. Endothelial cells and keratinocytes appear to be relevant in the inflammatory process, and abnormalities in these cells might be related to the spectrum of leprosy.
REFERENCES
1. BARKER, J. N. W. N., SARMA, V., MITRA, R. S., DIXIT, V. M. and NICKOLOFF, B. J. Marked synergism between tumor necrosis factor-alpha and interferon gamma in regulation of keratinocytederived adhesion molecules and chemotactic factors. J. Clin. Invest. 85(1990)605-608.
2. DUSTIN, M. L., SINGER, K. H., TUCK, D. T. and SPRINGER, T. A. Adhesion of T lymphoblasts to epidermal keratinocytes is regulated by interferon gamma and is mediated by intercellular adhesion molecule-1 (ICAM-1). J. Exp. Med. 167(1988)1323-1340.
3. GARCIA-GONZALEZ, E., SWERLICK, R. A. and LAWLEY, T. J. Cell adhesion molecules. Am. J. Dermatopathol. 12(1990)188-192.
4. GILHAR, A., AIZEN, E., PILLAR, T. and EIDELMAN, S. Response of aged versus young skin to intradermal administration of interferon gamma. J. Am. Acad. Dermatol. 27(1992)710-716.
5. GONZALEZ-AMARO, R., SALAZAR GONZALEZ, J. F., BARANDA, L., ABUD, C. and MONCADA, B. Evidence of cell-mediated immune contrasuppression in lepromatous leprosy: modulation of a putative T contrasuppressor cell subset. Clin. Exp. Immunol. 71(1988)399-404.
6. GRIFFITHS, C. E. M., VOORHEES, J. J. and NICKOLOFF, B. J. Characterization of intercellular adhesion molecule-1 and HLA-DR expression in normal and inflamed skin: modulation by recombinant gamma interferon and tumor necrosis factor. J. Am. Acad. Dermatol. 20(1989)617-629.
7. KLEIN, C. E., STEINMAYER, T., MATTES, J. M., KAUFMANN, R. and WEBERT, L. Integrins of normal human epidermis: differential expression, synthesis and molecular structure. Br. J. Dermatol. 123(1990)171-178.
8. KONTER, U., KELLNER, I., KLEIN, E., KAUFMANN, R., MIELKE, V. and STERRY, W. Adhesion molecule mapping in normal human skin. Arch. Dermatol. Res. 281(1989)454-462.
9. KRENSKY, A. M., SANCHEZ-MADRID, F., ROBBINS, E., NAGY. J. A.. SPRINGER, T. A. and BURAKOFF, S. J. The functional significance, distribution and structure of LFA-1, LFA-2, LFA-3: cell surface antigens with CTL-target interactions. J. Immunol. 131(1983)611-616.
10. KUPPER, T. S. Mechanisms of cutaneous inflammation interactions between epidermal cytokines, adhesion molecules and leukocytes. Arch. Dermatol. 125(1989)1406-1412.
11. MAKONKAWKEYYOON, S., KASINRERK, W., SUPA-JATURA, V., HIRUNPETCHARAT, C. and VITHAYASAI, V. Immunologic defects in leprosy patients. II interleukin-1, interleukin-2 and interferon production in leprosy patients. Int. J. Lepr. 58(1990)311-318.
12. MOH AG HEG H POUR, N., GELBER, R. H., LARRICK, J. W., SASAKI, D. T., BRENNAN, P. J. and ENGLE-MAN, E. G. Defective cell-mediated immunity in leprosy: failure of T-cells from lepromatous leprosy to respond to M. leprae is associated with defective expression of interleukin-2 receptors and is not reconstituted by IL-2. J. Immunol. 135(1985)1443-1449.
13. MOLLOY, A., GAUDERNACK. G., LEVIS, W. R., COHN, Z. A. and KAPLAN, G. Suppression of T-cell proliferation by Mycobacterium leprae and products: the role of lipopolysaccharidc. Proc. Natl. Acad. Sci. U.S.A. 87(1990)973-977.
14. NICKOLOFF, B. J. Role of interferon gamma in cutaneous trallicking of lymphocytes with emphasis on molecular and cellular adhesion events. Arch. Dermatol. 124(1988)1835-1843.
15. NORRIS, D. A. Cytokine modulation of adhesion molecules in the regulation of immunologic cytotoxicity of epidermal targets. J. Invest. Dermatol. 95(1990)11IS-120S.
16. SINGER, K. H., TUCK, D. T., SAMPSON, H. A. and HALL, R. P. Epidermal keratinocytes express the adhesion molecule intercellular adhesion molecule-1 in inflammatory dermatoses. J. Invest. Dermatol. 92(1989)746-750.
17. SULLIVAN, L., SANO, S., PIRMEZ, C, SALGAME, P., MUELLER, C, HOFMAN, F., UYEMURA, K., REA, T. H., BLOOM, B. R. and MODLIN, R. L. Expression of adhesion molecules in leprosy lesions. Infect. Immun. 59(1991)4150-4160.
1. M.D.; Hospital Central, School of Medicine of San Luis Potosi, Av. V. Carranza 2405, 78210 San Luis Potosi, S.L.P., México.
2. M.D.; Hospital Central, School of Medicine of San Luis Potosi, Av. V. Carranza 2405, 78210 San Luis Potosi, S.L.P., México.
3. M.D.; Hospital Central, School of Medicine of San Luis Potosi, Av. V. Carranza 2405, 78210 San Luis Potosi, S.L.P., México.
4. Biol.; Hospital Central, School of Medicine of San Luis Potosi, Av. V. Carranza 2405, 78210 San Luis Potosi, S.L.P., México.
5. M.D.; Hospital Central, School of Medicine of San Luis Potosi, Av. V. Carranza 2405, 78210 San Luis Potosi, S.L.P., México.
6. Biol., Hospital Central, School of Medicine of San Luis Potosi, Av. V. Carranza 2405, 78210 San Luis Potosi, S.L.P., México.
7. M.D., Centro de Salud, Ministry of Health, León, Gto., México.
Received for publication on 25 January' 1993.
Accepted for publication in revised form on 18 August 1993.